Abstract
Purpose of Review
Anemia is the most common complication as well as an extra intestinal manifestation of inflammatory bowel disease (IBD). It is associated with a significant impact on patient’s quality of life (QoL); as well it represents a common cause of frequent hospitalization, delay of hospital inpatient discharge and overall increased healthcare burden. In spite of all these, anemia is still often underdiagnosed and undertreated. Our aim in this review is to provide a pathway for physicians to help them achieve early diagnosis as well as timely and appropriate treatment of anemia which in turn would hopefully reduce the prevalence and subsequent complications of this condition among IBD patients.
Recent Findings
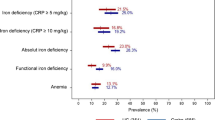
The etiology of anemia among IBD patients is most commonly due to iron deficiency anemia (IDA) followed by anemia of chronic disease. Despite this, more than a third of anemic ulcerative colitis (UC) patients are not tested for IDA and among those tested and diagnosed with IDA, a quarter are not treated with iron replacement therapy. A new algorithm has been validated to predict who will develop moderate to severe anemia at the time of UC diagnosis. While oral iron is effective for the treatment of mild iron deficiency-related anemia, the absorption of iron is influenced by chronic inflammatory states as a consequence of the presence of elevated levels of hepcidin. Also, it is important to recognize that ferritin is elevated in chronic inflammatory states and among patients with active IBD, ferritin levels less than 100 are considered to be diagnostic of iron deficiency. Newer formulations of intra-venous (IV) iron have a good safety profile and can be used for replenishment of iron stores and prevention of iron deficiency in the future.
Summary
Routine screening for anemia is important among patients with IBD. The cornerstone for the accurate management of anemia in IBD patients lies in accurately diagnosing the type of anemia. All IBD patients with IDA should be considered appropriate for therapy with iron supplementation whereas IV administration of iron is recommended in patients with clinically active IBD, or for patients who are previously intolerant to oral iron, with hemoglobin levels below 10 g/dL, and in patients who need erythropoiesis-stimulating agents (ESAs). As the recurrence of anemia is common after resolution, the monitoring for recurrent anemia is equally important during the course of therapy.


Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn's disease. Aliment Pharmacol Ther. 2006;24:1507–23.
de la Morena F, Gisbert JP. Anemia and inflammatory bowel disease. Rev Esp Enferm Dig. 2008;100:285–93.
Gasche C. Anemia in IBD: the overlooked villain. Inflamm Bowel Dis. 2000;6:142–50.
Gisbert JP, Gomollon F. Common misconceptions in the diagnosis and management of anemia in inflammatory bowel disease. Am J Gastroenterol. 2008;103:1299–307.
Danese S, Hoffman C, Vel S, et al. Anaemia from a patient perspective in inflammatory bowel disease: results from the European Federation of Crohn’s and Ulcerative Colitis Association’s online survey. Eur J Gastroenterol Hepatol. 2014;26:1385–91.
Stein J, Bager P, Befrits R, et al. Anaemia management in patients with inflammatory bowel disease: routine practice across nine European countries. Eur J Gastroenterol Hepatol. 2013;25:1456–63.
Blumenstein I, Dignass A, Vollmer S, et al. Current practice in the diagnosis and management of IBD-associated anaemia and iron deficiency in Germany: the German AnaemIBD Study. J Crohns Colitis. 2014;8:1308–14.
Bager P, Befrits R, Wikman O, et al. The prevalence of anemia and iron deficiency in IBD outpatients in Scandinavia. Scand J Gastroenterol. 2011;46:304–9.
Voegtlin M, Vavricka SR, Schoepfer AM, et al. Prevalence of anaemia in inflammatory bowel disease in Switzerland: a cross-sectional study in patients from private practices and university hospitals. J Crohns Colitis. 2010;4:642–8.
Bager P, Befrits R, Wikman O, et al. High burden of iron deficiency and different types of anemia in inflammatory bowel disease outpatients in Scandinavia: a longitudinal 2- year follow-up study. Scand J Gastroenterol. 2013;48:1286–93.
• Filmann N, Rey J, Schneeweiss S, et al. Prevalence of anemia in inflammatory bowel diseases in european countries: a systematic review and individual patient data metaanalysis. Inflamm Bowel Dis. 2014;20:936–45. A recent analysis of the frequency of anaemia in IBD patients in European countries.
Rejler M, Tholstrup J, Andersson-Gare B, et al. Low prevalence of anemia in inflammatory bowel disease: a population-based study in Sweden. Scand J Gastroenterol. 2012;47:937–42.
Bergamaschi G, Di Sabatino A, Albertini R, et al. Prevalence and pathogenesis of anemia in inflammatory bowel disease. Influence of anti-tumor necrosis factor-alpha treatment. Haematologica. 2010;95:199–205.
Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev. Gastroenterol Hepatol. 2010;7:599–610.
Gomollon F, Gisbert JP. Anemia and inflammatory bowel diseases. World J Gastroenterol. 2009;15:4659–65.
Pizzi LT, Weston CM, Goldfarb NI, Moretti D, Cobb N, Howell JB, et al. Impact of chronic conditions on quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2006;12(1):47–52.
Wells CW, Lewis S, Barton JR, Corbett S. Effects of changes in hemoglobin level on quality of life and cognitive function in inflammatory bowel disease patients. Inflamm Bowel Dis. 2006;12:123–30.
Ershler WB, Chen K, Reyes EB, Dubois R. Economic burden of patients with anemia in selected diseases. Value Health. 2005;8:629–38.
Ott C, Liebold A, Takses A, et al. High prevalence but insufficient treatment of iron-deficiency anemia in patients with inflammatory bowel disease: results of a population-based cohort. Gastroenterol Res Pract. 2012;2012:595970.
Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846–53. e841–42
• Khan N, Patel D, Shah Y, Yang YX. Factors predicting testing and treatment of iron deficiency in a nationwide cohort of anemic UC patients. Inflamm Bowel Dis. 2016;22(12):2894–2901. https://doi.org/10.1097/MIB.0000000000000947.
Beutler E, Waalen J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107:1747–50.
Perry GS, Byers T, Yip R, Margen S. Iron nutrition does not account for the hemoglobin differences between blacks and whites. J Nutr. 1992;122:1417–24.
WHO, UNICEF, UNU. Iron deficiency anemia: assessment, prevention and control. Report of a joint WHO/UNICEF/UNU consultation. Geneva: World Health Organization 1998.
Gasche C, Berstad A, Befrits R, Beglinger C, Dignass A, Erichsen K, et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis. 2007;13(12):1545–53.
Murawska N, Fabisiak A, Fichna J. Anemia of chronic disease and iron deficiency anemia in inflammatory bowel diseases: pathophysiology, diagnosis, and treatment. Inflamm Bowel Dis. 2016;22(5):1198–208.
Mucke V, Mucke MM, Raine T, Bettenworth D. Diagnosis and treatment of anemia in patients with inflammatory bowel disease. Ann Gastroenterol. 2017;30(1):15–22.
Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352(10):1011–23.
Zarychanski R, Houston DS. Anemia of chronic disease: a harmful disorder or an adaptive, beneficial response? CMA J. 2008;179:333–7.
• Battat R, Kopylov U, Szilagyi A, et al. Vitamin B12 deficiency in inflammatory bowel disease: prevalence, risk factors, evaluation, and management. Inflamm Bowel Dis. 2014;20:1120–8. This very comprehensive review shows that vitamin B12 deficiency anaemia is not uncommon after restorative proctocolectomy, and that it has negative effects on the patient’s quality of life
M’Koma AE, Wise PE, Schwartz DA, et al. Prevalence and outcome of anemia after restorative proctocolectomy: a clinical literature review. Dis Colon Rectum. 2009;52:726–39.
Onal IK. Folatedeficiency in Crohn’s disease. Scand J Gastroenterol. 2014;49:253–4.
Bermejo F, Algaba A, Guerra I, et al. Should we monitor vitamin B12 and folate levels in Crohn’s disease patients? Scand J Gastroenterol. 2013;48:1272–7.
• Devalia V, Hamilton MS, Molloy AM, et al. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol. 2014;166:496–513. https://doi.org/10.1111/bjh.12959.
De Clerck YA, Ettenger RB, Ortega JA, Pennisi AJ. Macrocytosis and pure RBC anemia caused by azathioprine. Am J Dis Child 1980;134:377–9. European Consensus on the Diagnosis and Management of Iron Deficiency 221.
Formea CM, Myers-Huentelman H, Wu R, et al. Thiopurine S-methyltransferase genotype predicts azathioprine-induced myelotoxicity in kidney transplant recipients. Am J Transplant. 2004;4:1810–7.
Agrawal A, Parrott NR, Riad HN, Augustine T. Azathioprine induced pure red cell aplasia: case report and review. Transplant Proc. 2004;36:2689–91.
Old CW, Flannery EP, Grogan TM, Stone WH, San Antonio RP. Azathioprine-induced pure red blood cell aplasia. JAMA. 1978;240:552–4.
Taffet SL, Das KM. Sulfasalazine. Adverse effects and desensitization. Dig Dis Sci. 1983;28(9):833–42.
Gutierrez-Ureña S, Molina JF, García CO, Cuéllar ML, Espinoza LR. Pancytopenia secondary to methotrexate therapy in rheumatoid arthritis. Arthritis Rheum. 1996;39(2):272.
Giannadaki E, Potamianos S, Roussomoustakaki M, et al. Autoimmune hemolytic anemia and positive Coombs test associated with ulcerative colitis. Am J Gastroenterol. 1997;92:1872–4.
Manosa M, Doménech E, Sánchez-Delgado J, Bernal I, García-Planella E, Gassull MA. Autoimmune hemolytic anemia associated with ulcerative colitis. Gastroenterol Hepatol. 2005;28(5):283–4.
Wilson A, Reyes E, Ofman J. Prevalence and outcomes of anemia in inflammatory bowel disease: a systematic review of the literature. Am J Med. 2004;116(Suppl 7A):44S–9S.
•• Dignass AU, Gasche C, Bettenworth D, et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9:211–22. This paper highlights the current standards in the diagnosis and management of anaemia in IBD patients and is the result of a European consensus process under the guidance of the European Crohn’s and Colitis Organisation [ECCO]
Duerksen DR, Fallows G, Bernstein CN. Vitamin B12 malabsorption in patients with limited ileal resection. Nutrition. 2006;22:1210–3.
Hou JK, et al. Assessment of gaps in care and the development of a care pathway for anemia in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2016;23(1):35–43.
Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013;7:1–33.
Polin V, Coriat R, Perkins G, et al. Iron deficiency: from diagnosis to treatment. Dig Liver Dis. 2013;45(10):803–9.
Wish JB. Assessing iron status: beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol. 2006;1(Suppl 1):S4–8.
Auerbach M, Adamson JW. How we diagnose and treat iron deficiency anemia. Am J Hematol. 2016;91(1):31–8.
Kulnigg S, Teischinger L, Dejaco C, Waldhor T, Gasche C. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment. Am J Gastroenterol. 2009;104:1460–7.
Beguin Y. Soluble transferrin receptor for the evaluation of erythropoiesis and iron status. Clin Chim Acta. 2003;329:9–22.
Oustamanolakis P, Koutroubakis IE, Messaritakis I, et al. Soluble transferrin receptorferritin index in the evaluation of anemia in inflammatory bowel disease: a casecontrol study. Ann Gastroenterol. 2011;24:108–14.
Infusino I, Braga F, Dolci A, Panteghini M. Soluble transferrin receptor [sTfR] and sTfR/log ferritin index for the diagnosis of iron-deficiency anemia: a meta-analysis. Am J Clin Pathol. 2012;138:642–9.
Skikne BS, Punnonen K, Caldron PH, et al. Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: a prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am J Hematol. 2011;86:923–7.
Martin J, Radeke HH, Dignass A, Stein J. Current evaluation and management of anemia in patients with inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2017;11(1):19–32.
Yakut M, Ustun Y, Kabacam G, Soykan I. Serum vitamin B12 and folate status in patients with inflammatory bowel diseases. Eur J Intern Med. 2010;21:320–3.
Alkhouri RH, Hashmi H, Baker RD, Gelfond D, Baker SS. Vitamin and mineral status in patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2013;56:89–92.
Green R. Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94:666S–72S.
Camaschella C. Iron-Deficiency Anemia. N Engl J Med. 2015;373(5):485–6.
Anker SD, Comin Colet J, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361:2436–48.
Favrat B, Balck K, Breymann C, et al. Evaluation of a single dose of ferric carboxymaltose in fatigued, iron-deficient women—PREFER, a randomized, placebo-controlled study. PLoS One. 2014;9:e94217.
Krayenbuehl PA, Battegay E, Breymann C, Furrer J, Schulthess G. Intravenous iron for the treatment of fatigue in nonanemic, premenopausal women with low serum ferritin concentration. Blood. 2011;118:3222–7.
Waldhoer T, Feichtenschlager T, et al. Prediction of response to iron sucrose in inflammatory bowel disease-associated anemia. Am J Gastroenterol. 2001;96:2382–7.
Schroder O, Mickisch O, Seidler U, et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease—a randomized, controlled, open-label, multicenter study. Am J Gastroenterol. 2005;100:2503–9.
de Silva AD, Tsironi E, Feakins RM, Rampton DS. Efficacy and tolerability of oral iron therapy in inflammatory bowel disease: a prospective, comparative trial. Aliment Pharmacol Ther. 2005;22(11–12):1097–105.
Ruiz-Arguelles GJ, Diaz-Hernandez A, Manzano C, Ruiz-Delgado GJ. Ineffectiveness of oral iron hydroxide polymaltose in iron-deficiency anemia. Hematology. 2007;12(3):255–6.
Kaltwasser JP, Werner E, Niechzial M. Bioavailability and therapeutic efficacy of bivalent and trivalent iron preparations. Arzneimittelforschung. 1987;37(1A):122–9.
Malhotra S, Garg SK, Khullar GK, et al. Kinetics of two different iron formulations and their effect on diurnal variation of serum iron levels. Methods Find Exp Clin Pharmacol. 2004;26(6):417–20.
Gasche C, Ahmad T, Tulassay Z, et al. Ferric maltol is effective in correcting iron deficiency anemia in patients with inflammatory bowel disease: results from a phase-3 clinical trial program. Inflammatory Bowel Dis. 2015;21(3):579–88.
Schmidt C, Ahmad T, Tulassay Z, et al. Ferric maltol therapy for iron deficiency anaemia in patients with inflammatory bowel disease: long-term extension data from a phase 3 study. Aliment Pharmacol Ther. 2016;44(3):259–70.
Stoffel NU, Cercamondi CI, Brittenham G, Zeder C, Geurts-Moespot AJ, Swinkels DW, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4(11):e524–33.
Tolkien Z, Stecher L, Mander AP, et al. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and metaanalysis. PLoS One. 2015;10:e0117383.
Tay HS, Soiza RL. Systematic review and meta-analysis: what is the evidence for oral iron supplementation in treating anaemia in elderly people? Drugs Aging. 2015;32:149–58.
Goldberg ND. Iron deficiency anemia in patients with inflammatory bowel disease. Clin Exp Gastroenterol. 2013;6:61.
Kara M, Hasinoff BB, DW MK, Campbell NR. Clinical and chemical interactions between iron preparations and ciprofloxacin. Br J Clin Pharmacol. 1991;31(3):257–61.
Hallberg L, Rossander L, Skånberg AB. Phytates and the inhibitory effect of bran on iron absorption in man. Am J Clin Nut. 1987;45(5):988–96.
Disler P, Lynch SR, Charlton RW, Torrance JD, Bothwell TH, Walker RB, et al. The effect of tea on iron absorption. Gut. 1975;16(3):193–200.
Kortman GA, Raffatellu M, Swinkels DW, et al. Nutritional iron turned inside out: intestinal stress from a gut microbial perspective. FEMS Microbiol Rev. 2014;38:1202–34.
Okam MM, Koch TA, Tran MH. Iron deficiency anemia treatment response to oral iron therapy: a pooled analysis of five randomized controlled trials. Haematologica. 2016;101:e6–7.
Evstatiev R, Alexeeva O, Bokemeyer B, et al. Ferric carboxymaltose prevents recurrence of anemia in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2013;11:269–77.
Kulnigg S, Stoinov S, Simanenkov V, et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose [FERINJECT] randomized controlled trial. Am J Gastroenterol. 2008;103:1182–92.
Onken JE, Bregman DB, Harrington RA, et al. A multicenter, randomized, active-controlled study to investigate the efficacy and safety of intravenous ferric carboxymaltose in patients with iron deficiency anemia. Transfusion. 2014;54:306–15.
Lyseng-Williamson KA, Keating GM. Ferric carboxymaltose: a review of its use in iron-deficiency anemia. Drugs. 2009;69:739–56.
Rodgers GM, Auerbach M, Cella D, Chertow GM, Coyne DW, Glaspy JA, et al. High-molecular weight iron dextran: a wolf in sheep’s clothing? J Am Soc Nephrol. 2008;19(5):833.
Auerbach M, Ballard H. Clinical use of intravenous iron: administration, efficacy, and safety. Hematol Am Soc Hematol Educ Program. 2010;2010:338.
Yessayan L, Sandhu A, Besarab A, et al. Intravenous iron dextran as a component of anemia management in chronic kidney disease: a report of safety and efficacy. Int J Nephrol. 2013;2013:703,038.
Koutroubakis IE, Oustamanolakis P, Karakoidas C, Mantzaris GJ, Kouroumalis EA. Safety and efficacy of total-dose infusion of low molecular weight iron dextran for iron deficiency anemia in patients with inflammatory bowel disease. Dig Dis Sci. 2010;55:2327–31.
Lindgren S, Wikman O, Befrits R, et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anemia and restoring iron stores in IBD patients: a randomized, controlled, evaluator-blind, multicentre study. Scand J Gastroenterol. 2009;44:838–45.
Auerbach M, Deloughery T. Single-dose intravenous iron for iron deficiency: a new paradigm. Hematol Am Soc Hematol Educ Program. 2016 Dec;2016(1):57–66.
Reinisch W, Staun M, Tandon RK, et al. A randomized, open-label, noninferiority study of intravenous iron isomaltoside 1000 [Monofer] compared with oral iron for treatment of anemia in IBD [PROCEED]. Am J Gastroenterol. 2013;108:1877–88.
Ford D, Cohen M, Strauss W, et al. Evaluation of ferumoxytol treatment for iron deficiency anemia in patients with gastrointestinal disorders who have a history of unsatisfactory oral iron therapy: results of a Phase III, randomized, placebo-controlled trial. Gastroenterology. 2013;144:S754.
Geisser P, Baer M, Schaub E. Structure/histotoxicity relationship of parenteral iron preparations. Arzneimittelforschung. 1992;42:1439–52.
Aksan A, Işık H, Radeke HH, Dignass A, Stein J. Systematic review with network meta-analysis: comparative efficacy and tolerability of different intravenous iron formulations for the treatment of iron deficiency anaemia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2017;45:1303–18. https://doi.org/10.1111/apt.14043.
Dahlerup JF, Jacobsen BA, van der Woude J, Bark LÅ, Thomsen LL, Lindgren S. High-dose fast infusion of parenteral iron isomaltoside is efficacious in inflammatory bowel disease patients with iron-deficiency anaemia without profound changes in phosphate or fibroblast growth factor 23. Scand J Gastroenterol. 2016;51(11):1332–8.
Vikrant S, Parashar A. The safety and efficacy of high dose ferric carboxymaltose in patients with chronic kidney disease: a single center study. Indian J Nephrol. 2015;25(4):213.
Ganzoni AM. Intravenous iron-dextran: therapeutic and experimental possibilities. Schweiz Med Wochenschr. 1970;100:301–3.
Miller HJ, Hu J, Valentine JK, Gable PS. Efficacy and tolerability of intravenous ferric gluconate in the treatment of iron deficiency anemia in patients without kidney disease. Arch Intern Med. 2007;167(12):1327.
Cavill I, Auerbach M, Bailie GR, et al. Iron and the anemia of chronic disease: a review and strategic recommendations. Curr Med Res Opin. 2006;22:731–7.
Reinisch W, Altorjay I, Zsigmond F, et al. A 1-year trial of repeated high-dose intravenous iron isomaltoside 1000 to maintain stable hemoglobin levels in inflammatory bowel disease. Scand J Gastroenterol. 2015;50:1226–33.
Nissenson AR, Wade S, Goodnough T, Knight K, Dubois RW. Economic burden of anemia in an insured population. J Manag Care Pharm. 2005;11:565–74.
Tsiolakidou G, Koutroubakis IE. Stimulating erythropoiesis in inflammatory bowel disease associated anemia. World J Gastroenterol. 2007;13:4798–806.
Weiss G, Gasche C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica. 2010;95:175–8.
Rubin DT, Mulani P, Chao J, et al. Effect of adalimumab on clinical laboratory parameters in patients with Crohn’s disease: results from the CHARM trial. Inflamm Bowel Dis. 2012;18:818–25.
Gasche C, Dejaco C, Waldhoer T, et al. Intravenous iron and erythropoietin for anemia associated with Crohn disease. A randomized, controlled trial. Ann Intern Med. 1997;126:782–7.
Gasche C, Dejaco C, Reinisch W, et al. Sequential treatment of anemia in ulcerative colitis with intravenous iron and erythropoietin. Digestion. 1999;60:262–7.
Koutroubakis IE, Karmiris K, Makreas S, Xidakis C, Niniraki M, Kouroumalis EA. Effectiveness of darbepoetin-alfa in combination with intravenous iron sucrose in patients with inflammatory bowel disease and refractory anemia: a pilot study. Eur J Gastroenterol Hepatol. 2006;18:421–5.
Schreiber S, Howaldt S, Schnoor M, et al. Recombinant erythropoietin for the treatment of anemia in inflammatory bowel disease. N Engl J Med. 1996;334:619–23.
Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013;368:149–60.
Kemna EH, Tjalsma H, Willems HL, Swinkels DW. Hepcidin: from discovery to differential diagnosis. Haematologica. 2008;93(1):90–7.
Hashizume M, Uchiyama Y, Horai N, et al. Tocilizumab, a humanized anti-interleukin-6 receptor antibody, improved anemia in monkey arthritis by suppressing IL-6-induced hepcidin production. Rheumatol Int. 2010;30:917–23.
• Vadhan-Raj S, Abonour R, Goldman JW, Smith DA, Slapak CA, Ilaria RL, et al. A first-in-human phase 1 study of a hepcidin monoclonal antibody, LY2787106, in cancer-associated anemia. J Hematol Oncol. 2017;10(1):73. https://doi.org/10.1186/s13045-017-0427-x.
Leung D, Hill KA, De Rosa DC, et al. LY2928057, an antibody targeting ferroportin, is a potent inhibitor of hepcidin activity and increases iron mobilization in normal cynomolgus monkeys. Blood. 2013;122:3433.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dhruvan Patel declares that he has no conflict of interest. Chinmay Trivedi declares that he has no conflict of interest. Nabeel Khan declares that he has no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Inflammatory Bowel Disease
Rights and permissions
About this article
Cite this article
Patel, D., Trivedi, C. & Khan, N. Management of Anemia in Patients with Inflammatory Bowel Disease (IBD). Curr Treat Options Gastro 16, 112–128 (2018). https://doi.org/10.1007/s11938-018-0174-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-018-0174-2