Abstract
Purpose of Review
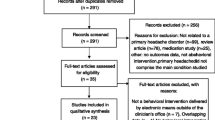
This narrative review examines the use of behavioral interventions for acute treatment of headache and pain in the emergency department (ED)/urgent care (UC) and inpatient settings.
Recent Findings
Behavioral interventions demonstrate reductions of pain and associated disability in headache, migraine, and other conditions in the outpatient setting. Behavioral treatments may be a useful addition for patients presenting with acute pain to hospitals and emergency departments.
Summary
We review challenges and limitations and offer suggestions for implementation of behavioral interventions in the acute setting. Some evidence exists for relaxation-based treatments, mindfulness-based treatments, hypnosis/self-hypnosis, and immersive virtual reality for acute pain, migraine, and headache. There are few high-quality studies on behavioral treatments in the inpatient and emergency department settings. Further research is warranted to determine the efficacy and cost-effectiveness of these interventions. Given the general safety and cost-effectiveness of behavioral interventions, healthcare professionals may want to include these therapies in treatment plans.
Similar content being viewed by others
Data Availability
Not applicable
Abbreviations
- MBSR:
-
Mindfulness-based stress reduction
- MBCT:
-
Mindfulness-based cognitive therapy
- ACT:
-
Acceptance and commitment therapy
- CBT:
-
Cognitive behavioral therapy
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Weiss, A.J., et al., Overview of emergency department visits in the United States, 2011: statistical brief #174, in Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006: Rockville (MD).
Levin M. Approach to the workup and management of headache in the emergency department and inpatient settings. Semin Neurol. 2015;35(6):667–74.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624–45.
Penzien DB, Irby MB, Smitherman TA, Rains JC, Houle TT. Well-established and empirically supported behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19(7):34.
Flor H. Psychological pain interventions and neurophysiology: implications for a mechanism-based approach. Am Psychol. 2014;69(2):188–96.
Nicholson RA, Buse DC, Andrasik F, Lipton RB. Nonpharmacologic treatments for migraine and tension-type headache: how to choose and when to use. Curr Treat Options Neurol. 2011;13(1):28–40.
Haddock CK, Rowan AB, Andrasik F, Wilson PG, Talcott GW, Stein RJ. Home-based behavioral treatments for chronic benign headache: a meta-analysis of controlled trials. Cephalalgia. 1997;17(2):113–8.
Holroyd KA, O'Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, Carlson BW. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA. 2001;285(17):2208–15.
Powers SW, Kashikar-Zuck SM, Allen JR, LeCates SL, Slater SK, Zafar M, et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents: a randomized clinical trial. JAMA. 2013;310(24):2622–30.
Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN guidelines for prevention of episodic migraine: a summary and comparison with other recent clinical practice guidelines. Headache. 2012;52(6):930–45.
Powers SW, Coffey CS, Chamberlin LA, Ecklund DJ, Klingner EA, Yankey JW, et al. Trial of amitriptyline, topiramate, and placebo for pediatric migraine. N Engl J Med. 2017;376(2):115–24.
Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19(4):13.
Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45(1):5–31.
Hughes LS, Clark J, Colclough JA, Dale E, McMillan D. Acceptance and commitment therapy (ACT) for chronic pain: a systematic review and meta-analyses. Clin J Pain. 2017;33(6):552–68.
Seng E, Singer AB, Metts C. Does mindfulness-based cognitive therapy for migraine reduce migraine-related disability in people with episodic and chronic migraine? A phase 2b pilot randomized clinical trial. Headache. 2019;59:1448–67.
Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407.
Henschke N, et al. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev. 2010;7:CD002014.
Monticone M, et al. Cognitive-behavioural treatment for subacute and chronic neck pain. Cochrane Database Syst Rev. 2015;5:CD010664.
Fisher E, et al. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2015;3:CD011118.
Eccleston C, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2014;5:CD003968.
Abbott RA, et al. Psychosocial interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;1:CD010971.
Adachi T, Fujino H, Nakae A, Mashimo T, Sasaki J. A meta-analysis of hypnosis for chronic pain problems: a comparison between hypnosis, standard care, and other psychological interventions. Int J Clin Exp Hypn. 2014;62(1):1–28.
Sielski R, Rief W, Glombiewski JA. Efficacy of biofeedback in chronic back pain: a meta-analysis. Int J Behav Med. 2017;24(1):25–41.
Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91.
Fisher E, et al. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2014;2014.
Flynn N. Systematic review of the effectiveness of hypnosis for the management of headache. Int J Clin Exp Hypn. 2018;66(4):343–52.
Hammond DC. Review of the efficacy of clinical hypnosis with headaches and migraines. Int J Clin Exp Hypn. 2007;55(2):207–19.
Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Whear RS, Thompson Coon J, et al. Recurrent abdominal pain in children: summary evidence from 3 systematic reviews of treatment effectiveness. J Pediatr Gastroenterol Nutr. 2018;67:23–33.
Montgomery GH, DuHamel KN, Redd WH. A meta-analysis of hypnotically induced analgesia: how effective is hypnosis? Int J Clin Exp Hypn. 2000;48(2):138–53.
Yang CP, Wang SJ. Sleep in patients with chronic migraine. Curr Pain Headache Rep. 2017;21(9):39.
Cheatle MD, Foster S, Pinkett A, Lesneski M, Qu D, Dhingra L. Assessing and managing sleep disturbance in patients with chronic pain. Sleep Med Clin. 2016;11(4):531–41.
Smith KE, Norman GJ. Brief relaxation training is not sufficient to alter tolerance to experimental pain in novices. PLoS One. 2017;12(5):e0177228.
Juhasz G, Zsombok T, Gonda X, Nagyne N, Modosne E, Bagdy G. Effects of autogenic training on nitroglycerin-induced headaches. Headache. 2007;47(3):371–83.
Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing--an experimental study. Pain Med. 2012;13(2):215–28.
Emery CF, France CR, Harris J, Norman G, VanArsdalen C. Effects of progressive muscle relaxation training on nociceptive flexion reflex threshold in healthy young adults: a randomized trial. Pain. 2008;138(2):375–9.
Esch T, et al. Neurobiological aspects of mindfulness in pain autoregulation: unexpected results from a randomized-controlled trial and possible implications for meditation research. Front Hum Neurosci. 2016;10:674.
Petter M, McGrath PJ, Chambers CT, Dick BD. The effects of mindful attention and state mindfulness on acute experimental pain among adolescents. J Pediatr Psychol. 2014;39(5):521–31.
Petter M, Chambers CT, MacLaren Chorney J. The effects of mindfulness-based attention on cold pressor pain in children. Pain Res Manag. 2013;18(1):39–45.
Grant JA, Rainville P. Pain sensitivity and analgesic effects of mindful states in Zen meditators: a cross-sectional study. Psychosom Med. 2009;71(1):106–14.
• Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, et al. Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. J Neurosci. 2015;35(46):15307–25. Study of mindfulness vs. several active controls for a thermal pain condition in healthy volunteers. The authors found improved pain tolerance in the mindfulness group. On fMRI, the mindfulness group was found to have differential activity in multiple areas involved in the cognitive processing of pain.
Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators. Pain. 2011;152(1):150–6.
Grant JA. Meditative analgesia: the current state of the field. Ann N Y Acad Sci. 2014;1307:55–63.
Schuyler BS, Kral TRA, Jacquart J, Burghy CA, Weng HY, Perlman DM, et al. Temporal dynamics of emotional responding: amygdala recovery predicts emotional traits. Soc Cogn Affect Neurosci. 2014;9(2):176–81.
Smith CA, et al. Acupuncture or acupressure for pain management in labour. Cochrane Database Syst Rev. 2011;7:CD009232.
• Duncan LG, Cohn MA, Chao MT, Cook JG, Riccobono J, Bardacke N. Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. BMC Pregnancy Childbirth. 2017;17(1):140. An RCT of mindfulness tailored to addressing fear of childbirth which found important maternal and fetal benefits, including reduction in postpartum depression.
• Minen M, et al. Introduction to progressive muscle relaxation therapy for migraine in the emergency department: a pilot feasibility study (P2.168). Neurology. 2017;88(16 Supplement). A pilot study demonstrating the feasibility of administering a relaxation exercise to patients with severe migraine in the ED setting.
• Ziehm S, et al. Psychological interventions for acute pain after open heart surgery. Cochrane Database Syst Rev. 2017;7:CD009984. A large meta-analysis of psychological treatments for post-surgical pain, finding benefits for mental distress but not pain.
Seers K, Carroll D. Relaxation techniques for acute pain management: a systematic review. J Adv Nurs. 1998;27(3):466–75.
•• Garland EL, Baker AK, Larsen P, Riquino MR, Priddy SE, Thomas E, et al. Randomized controlled trial of brief mindfulness training and hypnotic suggestion for acute pain relief in the hospital setting. J Gen Intern Med. 2017;32(10):1106–13. A recent RCT of 2 brief psychological interventions delivered by social workers for acute pain relief in hospitalized patients, showing benefit in both interventions compared to an active control condition.
• Ardigo S, Herrmann FR, Moret V, Déramé L, Giannelli S, Gold G, et al. Hypnosis can reduce pain in hospitalized older patients: a randomized controlled study. BMC Geriatr. 2016;16:14. A recent RCT of 3 short sessions of hypnosis (aimed at teaching the patient self-hypnosis) vs. massage for elderly patients with chronic pain, showing benefit to the hypnosis intervention.
Katz ER, Kellerman J, Ellenberg L. Hypnosis in the reduction of acute pain and distress in children with cancer. J Pediatr Psychol. 1987;12(3):379–94.
Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014;30(12):1089–98.
•• Won AS, et al. Immersive virtual reality for pediatric pain. Children (Basel). 2017;4(7). A recent review of IVR for pediatric pain, with practical suggestions of which hardware and software can be used.
•• Tashjian VC, Mosadeghi S, Howard AR, Lopez M, Dupuy T, Reid M, et al. Virtual reality for management of pain in hospitalized patients: results of a controlled trial. JMIR Ment Health. 2017;4(1):e9. A recent RCT demonstrating superiority of IVR vs. a 2-D movie distraction condition for diverse types of pain in hospitalized patients.
Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, et al. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin Psychol Rev. 2018;59:52–60.
Ernst MM, O'Brien HL, Powers SW. Cognitive-behavioral therapy: how medical providers can increase patient and family openness and access to evidence-based multimodal therapy for pediatric migraine. Headache. 2015;55(10):1382–96.
Kroon Van Diest AM, et al. Adherence to biobehavioral recommendations in pediatric migraine as measured by electronic monitoring: the adherence in migraine (AIM) study. Headache. 2016;56(7):1137–46.
Minen MT, Torous J, Raynowska J, Piazza A, Grudzen C, Powers S, et al. Electronic behavioral interventions for headache: a systematic review. J Headache Pain. 2016;17:51.
Funding
Dr. Mia Minen: NIH NCCIH: K23 AT009706-01
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dan Vekhter and Mia Minen declare no conflict of interest. Matthew Robbins receives book royalties from Wiley and an editorial stipend from Springer. He serves in non-remunerative positions as a member of the American Headache Society Board of Directors and on the editorial board for Headache. Dawn Buse has received grant funding, research support, and honoraria from Amgen, Allergan, Biohaven, Lilly, and Teva and is a section editor for Current Pain and Headache Reports but has not been involved in the review of this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Code Availability
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Psychological and Behavioral Aspects of Headache with Pain
Rights and permissions
About this article
Cite this article
Vekhter, D., Robbins, M.S., Minen, M. et al. Efficacy and Feasibility of Behavioral Treatments for Migraine, Headache, and Pain in the Acute Care Setting. Curr Pain Headache Rep 24, 66 (2020). https://doi.org/10.1007/s11916-020-00899-z
Published:
DOI: https://doi.org/10.1007/s11916-020-00899-z