Abstract
The perceived advantages of endovascular treatment for acute ischemic stroke in terms of recanalization, the multimodal and targeted approaches, and perhaps the more permissive rules on devices than on medications for their licensing favored the assumption that endovascular treatment is superior to intravenous thrombolysis for acute treatment of ischemic stroke, and its adoption in more advanced stroke centers. However, this assumption has been questioned by recent clinical trial experience showing that endovascular treatment is not superior to intravenous thrombolysis. The new evidence has changed the perception and the importance of conducting randomized trials in this area. This summary examines the background and outcomes of the latest experience with endovascular techniques in acute stroke treatment based on historical data. The new challenge is how to study the latest generation of devices called stent retrievers, which are faster in recanalizing and easier to use, in selected patients with acute ischemic stroke. In the meantime, the available evidence does not provide support for the use of endovascular treatment of acute ischemic stroke in clinical practice.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012;379:2364–72.
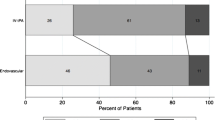
•• Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous rt-PA versus rt-PA alone for stroke. N Engl J Med. 2013;368:893–903. Randomized trial comparing ET in patients pre-treated with i.v. rt-PA within 3 hours of symptom onset, with standard i.v. rt-PA; endovascular approach chosen by the site neurointerventionalist (i.e., thrombectomy with the Merci retriever, Penumbra System, or Solitaire, or endovascular delivery of rt-PA by means of the Micro-Sonic SV infusion system or a standard microcatheter) in 656 patients with acute ischemic stroke (NIHSS score, ≥ 10). The trial showed similar safety outcomes and no significant difference in functional independence with ET after intravenous rt-PA compared with i.v. rt-PA alone.
•• Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368:904–13. Randomized trial comparing ET with standard i.v. rt-PA alone in 362 patients with acute ischemic stroke. Patients had to be eligible for i.v. rt-PA; ET approach was chosen by site neurointerventionalist and the use of any device available on the market at the time of the study was allowed. The trial showed that ET is not superior to standard treatment with i.v. rt-PA alone.
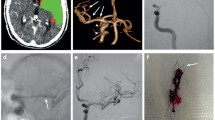
•• Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–23. Randomized trial comparing mechanical embolectomy (Merci Retriever or Penumbra System) with standard care in 127 patients with large vessel, anterior-circulation strokes, within 8 hours of onset; randomization was stratified according to whether the patient had a favorable penumbral pattern (substantial salvageable tissue and small infarct core) or a non-penumbral pattern (large core or small or absent penumbra) at pre-treatment multimodal CT or MRI of the brain. The trial showed that a favorable penumbral pattern on neuroimaging did not identify patients who would differentially benefit from ET for acute ischemic stroke, nor was embolectomy shown to be superior to standard care.
del Zoppo GJ, Zeumer H, Harker LA. Thrombolytic therapy in acute stroke: Possibilities and hazards. Stroke. 1986;17:595–607.
Fletcher AP, Alkjaersig N, Lewis M, et al. A pilot study of urokinase therapy in cerebral infarction. Stroke. 1976;7:135–42.
Hanaway J, Torack R, Fletcher AP, et al. Intracranial bleeding associated with urokinase therapy for acute ischemic hemispheral stroke. Stroke. 1976;7:143–6.
Caplan L. "Top of the basilar" syndrome: selected clinical aspects. Neurology. 1980;30:72–9.
Archer CT, Horenstein S. Basilar artery occlusion. Clinical and radiological correlation. Stroke. 1977;8:383–7.
Nenci GG, Gresele P, Taramelli M, et al. Thrombolytic therapy for thromboembolism of vertebrobasilar artery. Angiology. 1983;34:561–71.
Hacke W, Zeumer H, Ferbert A, et al. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–22.
•• del Zoppo GJ, Ferbert A, Otis S, et al. Local intra-arterial fibrinolytic therapy in acute carotid territory stroke: a pilot study. Stroke. 1988;19:307–13. First evidence of the feasibility of recanalization and safety with direct infusion of PAs in thrombotic/thromboembolic stroke in the carotid artery territory within 6–8 hours of symptom onset in a two-center collaborative effort..
•• Mori E, Tabuchi M, Yoshida T, et al. Intracarotid urokinase with thromboembolic occlusion of the middle cerebral artery. Stroke. 1988;19:802–12. First evidence of the feasibility of recanalization and safety with direct infusion of a PA in thrombotic/thromboembolic stroke in the carotid artery territory within 6–12 hours of symptom onset..
Zeumer H, Freitag HJ, Grzyka U, et al. Local intra-arterial fibrinolysis in acute vertebrobasilar occlusion. Technical developments and recent results. Neuroradiology. 1989;31:336–40.
Krause KH, Jackenkroll R, Betz H, et al. Recanalization of the internal carotid artery in a case of prolonged reversible ischemic neurological deficit. Nervenarzt. 1981;52:197–201.
•• del Zoppo GJ, Higashida RT, Furlan AJ, et al. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. Stroke. 1998;29:4–11. The only closed double-blinded prospective placebo controlled trial of a PA by direct i.a. delivery at an acute thrombotic occlusion in patients presenting with ischemic stroke. The agent, recombinant single chain urokinae (pro-urokinase), produced a significant increase in early recanalization. The heparin infusion used for maintaining sheath patency contributed to both recanalization efficacy and to the appearance of hemorrhagic transformation..
Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999;282:2003–11.
Ogawa A, Mori E, Minematsu K, et al. Randomized trial of intra-arterial infusion of urokinase within 6 hours of middle cerebral artery stroke. The Middle Cerebral Artery Embolism Local Fibrinolygic Intervention Trial (MELT) Japan. Stroke. 2007;38:2633–9.
Macleod MR, Davis SM, Mitchell JP, et al. Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovascular Dis. 2005;20:12–7.
Nogueira RG, Schwamm LH, Hirsch JA. Endovascular approaches to acute stroke, Part 1: Drugs, devices, and data. Am J Neurorad. 2009;30:649–61.
Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36:1432–8.
• Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39:1205–12. Multi MERCI was an international, multicenter, prospective, single-arm trial of thrombectomy in patients with large vessel stroke treated within 8 hours of symptom onset. Patients with persistent large vessel occlusion after i.v. tissue PA treatment were included. One hundred and sixty-four patients received thrombectomy and 131 were initially treated with the L5 Retriever. Overall, favorable clinical outcomes (modified Rankin Scale 0–2) occurred in 36% and mortality was 34%; both outcomes were significantly related to vascular recanalization. Symptomatic intracerebral hemorrhage occurred in 16 patients (9.8%). Clinically significant procedural complications occurred in nine (5.5%) patients..
• Penumbra Pivotal Stroke Trial Investigators. The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8. Prospective, multicenter, single-arm study to assess the safety and effectiveness of the Penumbra System in the revascularization of patients with acute ischemic stroke presented within 8 hours of symptom onset and with an angiographic occlusion of a treatable large intracranial vessel. Patients who presented within 3 hours of symptom onset had to be ineligible or refractory to rt-PA therapy. A total of 125 target vessels in 125 patients was treated by the Penumbra System. After the procedure, 81.6% of the treated vessels were successfully revascularized to TIMI 2 to 3. There were 18 procedural events reported in 16 patients (12.8%); three patients (2.4%) had events that were considered serious. A total of 14 (11.2%) suffered from a symptomatic intracranial hemorrhage. All-cause mortality was 32.8% at 90 days with 25% of the patients achieving a modified Rankin Scale score ≤ 2. The authors concluded that the Penumbra System allows safe and effective revascularization..
• Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380:1231–40. Randomized comparison of efficacy, in terms of recanalization rate, and safety of the Trevo Retriever with the Merci Retriever in 178 patients with angiographically-confirmed large cerebral artery occlusion strokes ineligible for or failure to respond to i.v. rt-PA. The endovascular procedure started within 8 hours of the time last assessed at baseline were eligible for the study. This trial demonstrated the superiority of Trevo over Merci Retriever..
• Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–9. Randomized comparison of efficacy, in terms of recanalization rate, and safety of the Solitaire Retriever with the Merci Retriever in 113 patients with angiographically-confirmed large cerebral artery occlusion strokes ineligible for or failure to respond to i.v. rt-PA. The endovascular procedure started within 8 hours of the time last assessed at baseline were eligible for the study. The trial demonstrated the superiority of Solitaire over the Merci retriever..
Mikulik R, Dusek L, Hill MD, et al. Pattern of response of National Institutes of Health Stroke Scale components to early recanalization in the CLOTBUST trial. Stroke. 2010;41:466–70.
Balucani C, Alexandrov AV. Ultrasound- and microspheres-enhanced thrombolysis for stroke treatment: state of the art. Curr Cardiol Rep. 2010;12:34–41.
• Mullen MT, Pisapia JM, Tilwa S, et al. Systematic review of outcome after ischemic stroke due to anterior circulation occlusion treated with intravenous, intra-arterial, or combined intravenous+intra-arterial thrombolysis. Stroke. 2012;43:2350–5. The authors performed a literature review and meta-analysis comparing the relative efficacy of six reperfusion strategies: i) 0.9 mg/kg i.v. tissue-type PA; ii) i.a. chemical thrombolysis; iii) i.a. mechanical thrombolysis; iv) i.a. combined chemical/mechanical thrombolysis; v) 0.6 mg/kg i.v. tissue-type PA and i.a. thrombolysis; and vi) 0.9 mg/kg i.v. tissue-type PA and i.a. thrombolysis. This study found no evidence that one reperfusion strategy is superior with respect to efficacy or safety, supporting clinical equipoise between reperfusion strategies..
Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet. 1998;351:1722–5.
Bailar 3rd JC. The powerful placebo and the Wizard of Oz. N Engl J Med. 2001;344:1630–2.
Hussein HM, Georgiadis AL, Vazquez G, et al. Occurrence and predictors of futile recanalization following endovascular treatment among patients with acute ischemic stroke: a multicenter study. AJNR Am J Neuroradiol. 2010;31:454–8.
Sorimachi T, Fujii Y, Tsuchiya N, et al. Recanalization by mechanical embolus disruption during intra-arterial thrombolysis in the carotid territory. AJNR Am J Neuroradiol. 2004;25:1391–402.
Ringer AJ, Qureshi AI, Fessler RD, et al. Angioplasty of intracranial occlusion resistant to thrombolysis in acute ischemic stroke. Neurosurgery. 2001;48:1282–8.
Qureshi AI, Siddiqui AM, Suri MF, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery. 2002;51:1319–27.
Bergui M, Stura G, Daniele D, et al. Mechanical thrombolysis in ischemic stroke attributable to basilar artery occlusion as first-line treatment. Stroke. 2006;37:145–50.
Leys D, Ringelstein EB, Kaste M, Hacke W. The main components of stroke unit care: Results of a European expert survey. Cerebrovasc Dis. 2007;23:344–52.
Consoli D, de Falco FA, Lenzi GL, Miceli G, Palombo F, Rosati G, Simonetti G, Stanzione P, Ugenti R, Zangrillo A. Cap 4. Le Stroke Unit: definizioni, criteri di accreditamento, indicatori e verifiche di qualità. Pp 13–19. In: Organizzazione dell’assistenza all’ictus: le Stroke Unit. Ministero della Salute Editor. Quaderni del Ministero della Salute, n.2, marzo-aprile 2010. Available at: http://www.quadernidellasalute.it/archivio-quaderni/2-marzo-aprile-2010.php. Accessed 20 Oct 2013.
Ciccone A, Valvassori L, Gasparotti R, et al. Debunking 7 myths that hamper the realization of randomized controlled trials on intra-arterial thrombolysis for acute ischemic stroke. Stroke. 2007;38:2191–5.
Johnston SC, Hauser SL. The dangers of clinical conviction: an “M&M” of endovascular therapies for stroke. Ann Neurol. 2013;73:A5–6.
Goyal M, Swartz RH. Epistemology, parachutes, and "yeah, but" interventional stroke trials. Stroke. 2013;44:2036–8.
Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–74.
Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–93.
Nogueira RG, Smith WS, Sung G, et al. Effect of time to reperfusion on clinical outcome of anterior circulation strokes treated with thrombectomy: pooled analysis of the MERCI and Multi MERCI trials. Stroke. 2011;42:3144–9.
Liebeskind DS, Sanossian N, Yong WH, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011;42:1237–43.
Legrand L, Naggara O, Turc G, et al. Clot burden score on admission T2*-MRI predicts recanalization in acute stroke. Stroke. 2013;44:1878–84.
Bang OY, Saver JL, Kim SJ, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011;42:693–9.
McVerry F, Liebeskind DS, Muir KW. Systematic review of methods for assessing leptomeningeal collateral flow. AJNR Am J Neuroradiol. 2012;33:576–82.
Compliance with Ethics Guidelines
Conflict of Interest
Alfonso Ciccone serves on the Clinical Events Committee of the TREVO (Thrombectomy REvascularization of large Vessel Occlusion in acute ischemic stroke) study for Concentric Medical Inc. Preparation of didactic material for the Stroke Day organized by the Italian Stroke Forum for Pierrel Research Italy SPA.
Gregory J. del Zoppo declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Ciccone, A., del Zoppo, G.J. Evolving Role of Endovascular Treatment of Acute Ischemic Stroke. Curr Neurol Neurosci Rep 14, 416 (2014). https://doi.org/10.1007/s11910-013-0416-6
Published:
DOI: https://doi.org/10.1007/s11910-013-0416-6