Abstract
Purpose of Review
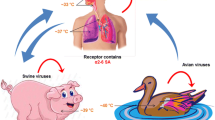
Zoonotic influenza viruses are those influenza viruses that cross the animal-human barrier and can cause disease in humans, manifesting from minor respiratory illnesses to multiorgan dysfunction. The increasing incidence of infections caused by these viruses worldwide has necessitated focused attention to improve both diagnostic as well as treatment modalities. In this second part of a two-part review, we discuss the clinical features, diagnostic modalities, and treatment of zoonotic influenza, and provide an overview of prevention strategies.
Recent Findings
Illnesses caused by novel reassortant avian influenza viruses continue to be detected and described; most recently, a human case of avian influenza A(H7N4) has been described from China. We continue to witness increasing rates of A(H7N9) infections, with the latest (fifth) wave, from late 2016 to 2017, being the largest to date. The case fatality rate for A(H7N9) and A(H5N1) infections among humans is much higher than that of seasonal influenza infections. Since the emergence of the A(H1N1) 2009 pandemic, and subsequently A(H7N9), testing and surveillance for novel influenzas have become more effective. Various newer treatment options, including peramivir, favipiravir (T-705), and DAS181, and human or murine monoclonal antibodies have been evaluated in vitro and in animal models.
Summary
Armed with robust diagnostic modalities, antiviral medications, vaccines, and advanced surveillance systems, we are today better prepared to face a new influenza pandemic and to limit the burden of zoonotic influenza than ever before. Sustained efforts and robust research are necessary to efficiently deal with the highly mutagenic zoonotic influenza viruses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This article is the second part of the two-part series titled “Zoonotic Influenza and Human Health.” In the previous issue of this journal, we described the structure of influenza virus and its effect on pathogenesis, the epidemiology of zoonotic influenza, and the major pandemics ascribed to zoonotic influenza described in human history. In this second and concluding part, we describe the clinical features, diagnosis and treatment of zoonotic influenza, and provide an overview of prevention strategies.
Clinical Features
Avian Influenza A(H5N1)
For human influenza A(H5N1) infections, bird-to-human is the predominant route of transmission; however, some degree of non-sustained human-to-human transmission has also occurred, and environment-to-human spread is also thought to occur [1]. Most patients with H5N1 infection give a history of recent exposure to dead or ill poultry. Current data indicate an incubation period of 7 days or less, with a mean of 2 to 5 days and ranging up to 17 days [2]. A distinct feature of avian influenza H5N1 is the predominance of cases in children and young adults. Patients have ranged in age from 3 months to 75 years, with the median age being 20 years. Half of all cases have occurred in people aged younger than 20 years, and 90% of cases have been in those younger than 40 years of age [3]. Most affected individuals present with respiratory symptoms, but patients with only gastrointestinal or central nervous system involvement have also been described. In most cases, respiratory symptoms may be accompanied by gastrointestinal symptoms, headache, myalgia, sore throat, rhinorrhea, or uncommonly conjunctivitis or bleeding gums. In severe cases, complications include multiorgan failure with renal dysfunction and cardiac compromise, pulmonary hemorrhage, pneumothorax, and pancytopenia. The case fatality rate is as high as 60%, with deaths resulting from respiratory failure [2]. Patients with severe disease often have leukopenia, neutropenia, lymphopenia, and thrombocytopenia on hospital admission [4,5,6]. Other laboratory abnormalities include transaminitis (AST > ALT), elevated lactate dehydrogenase, creatine kinase, and hypoalbuminemia [1, 4]. Radiographic findings of H5N1 avian influenza may be include diffuse, multifocal, or patchy infiltrates, interstitial infiltrates, and segmental or lobular consolidation [7]. Pleural effusions are usually not seen. Progression to respiratory failure is associated with diffuse bilateral ground-glass infiltrates [5]. Pathological changes observed at autopsy have included severe pulmonary injury with diffuse alveolar damage, alveolar hemorrhage, hyaline-membrane formation, lymphocytic infiltration into the interstitium, and the presence of reactive fibroblasts [8, 9].
Avian Influenza A(H7N9)
For both the H5N1 and H7N9 avian influenza viruses, the average incubation period is longer than that for seasonal influenza (2 days) [10]. The usual incubation period for H7N9 influenza has been estimated to be from 1 to 7 days (mean 5 days), but has been reported to be as long as 10 days [10]. Unlike H5N1 infections, fewer cases of H7N9 infection have been detected in children, with less than 3% of H7N9 infections occurring in children less than 10 years of age [11]. To date, there is no evidence of sustained human-to-human transmission, with most cases developing after exposure to infected poultry [12]. Presenting signs and symptoms may include fever, cough, dyspnea, headache, myalgias, and malaise [13, 14]. On laboratory examination, patients have been found to have lymphopenia and thrombocytopenia [15]. Elevated levels of aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, creatine kinase, and C-reactive protein have been reported [15, 16]. Complications including fulminant pneumonia, respiratory failure, acute respiratory distress syndrome (ARDS), septic shock, multiorgan failure, rhabdomyolysis, disseminated intravascular coagulation, and encephalopathy have been described [15,16,17]. The case fatality rate for A(H7N9) (approximately 40%) [18] virus infections among humans is much higher than that of seasonal influenza infections, but not as high as that of A(H5N1) (approximately 60%) [3, 12].
Other Avian Influenzas
Among individuals affected by avian influenza H5N6 infection, all cases but one were hospitalized, and in severe or critical condition, with 11 (69%) of cases fatal [11]. Avian influenza H7N7 and H7N3 viruses seem to have a preference for conjunctival epithelium, and affected individuals may present with isolated conjunctivitis following direct contact with poultry or inoculation with contaminated material [19, 20]. So far, one case of death due to avian influenza H7N7 has been recorded; a Dutch veterinarian reported having conjunctivitis, which developed 1 day after he had visited an affected farm, and he died a week later from respiratory distress [21]. H9N2 influenza viruses have been reported to cause mild, self-limited upper respiratory illnesses in children [22]. There has only been one fatal H9N2 infection documented, in an adult with underlying conditions, among the approximately 45 cases reported to WHO between 1998 and August 2017 [11]. Most recently, on 14 February 2018, the National Health and Family Planning Commission (NHFPC) of China notified the World Health Organization (WHO) of one case of human infection with avian influenza A(H7N4) virus. This is the first human case of avian influenza A(H7N4) infection to be reported worldwide. The case patient was a 68-year-old woman from Jiangsu Province with pre-existing cardiac disease, who was admitted to hospital for treatment of severe pneumonia after experiencing symptoms for a week, and she eventually improved after 21 days. The index case patient reported exposure to live backyard poultry prior to illness onset [23••].
Swine Influenza
From case series of humans infected with swine influenza, there are no clinical features that can distinguish swine influenza in humans from typical seasonal influenza, resulting in a likely underreporting of cases. Although a number of cases had predisposing underlying immunocompromising conditions, healthy persons were also at risk for illness and death from swine influenza [24]. The duration of illness also appears to be similar to typical uncomplicated seasonal influenza, lasting approximately 3 to 5 days [25••]. It is expected that exacerbation of underlying medical conditions is possible. Therefore, the same people at increased risk for complications of seasonal influenza would also likely be at a high risk for serious complications from variant virus infection [25••].
During the 2009 pandemic, deaths were observed in both immunocompetent and immunocompromised patients [26]. In addition to extremes of age and chronic underlying medical illness, other risk factors for severe disease or complications included immunosuppressive therapy, underlying neurological conditions, and obesity [27]. Globally, hospitalization rates of children with confirmed A(H1N1)pdm09 influenza were higher than those seen for seasonal influenza. Previously healthy young people and pregnant women (especially in their second and third trimester) also developed severe respiratory failure, occasionally associated with multiorgan failure and death. This was in contrast to seasonal influenza where fatal disease occurs mostly in the elderly (> 65 years old) [28].
Diagnostic Considerations for Zoonotic Influenzas
The identification of zoonotic influenzas and discrimination from human strains is a diagnostic challenge. Routine influenza testing often involves reverse transcription real-time PCR (RT-PCR) targeting the matrix (M) gene for influenza A, and the NS1 gene for influenza B, which is more sensitive than virus culture [29]. Subtyping PCRs targeting the HA and NA genes of seasonal influenzas are also available, and mostly used in reference laboratories, though incorporated in several commercial multiplex assays. Zoonotic IAVs are suspected when influenza A viruses do not match any of the seasonal subtypes when their respective HA and/or NA gene PCRs are run. If this occurs, such specimens should always be investigated further for the possible presence of a zoonotic influenza using subtyping PCRs targeting novel avian and/or swine subtypes and gene sequencing.
Zoonotic influenzas may also be detected if suspected clinically and specific subtyping PCRs are performed (e.g., avian H5, H7, H9, N1, N9), and followed up by gene sequencing of HA, NA, and other gene segments to further characterize the virus present in a clinical specimen. Because some swine variant influenza viruses can cross react with seasonal IAV subtyping PCRs, specimens can be screened with a swine NP gene PCR, or through gene sequencing, to identify them as swine variant viruses when clinically suspected.
Because the influenza A typing PCR targeting the M gene of influenza A is generally more sensitive than HA and NA subtyping PCRs, on occasion a sample containing a seasonal IAV with low viral load and high cycle threshold (CT) value will be influenza A-positive but not match any of the seasonal subtypes. The extent to which such samples are further investigated depends on the risk factors for zoonotic influenza in the particular patient being evaluated, and extensive further investigations are usually not required in such circumstances if there are no risk factors for zoonotic influenza infection.
Rapid or point of care (POC) modules have been gaining traction in recent years and are generally reliable for the detection of influenza type A and B antigens or nucleic acid. These tests yield results in a clinically actionable time frame (15–30 min) and are generally simple to perform. Most are capable of detecting human influenzas (A/B) but sensitivity and specificity can vary based on the IAV subtype [30, 31•, 32]. Of additional concern is the observed poorer analytical and clinical sensitivities when detecting zoonotic influenzas. In one study, several POC tests had “in-use” clinical sensitivities of 40–60% to avian H7N9 and swine H3N2v [33]. Poor performance for some subtypes might be due to predilection for lower respiratory tract mucosal cells with more α2-3-SA receptors, with typically sampled URT specimens not containing sufficient viral loads for detection [33].
Another challenge is that most tests often do not identify the influenza A virus subtype, which is an important first step in identifying zoonotic IAV strains causing human infection. Multiplex approaches have been devised that permit the detection of human influenza while providing some subtyping information, but these are generally aimed at identifying currently circulating seasonal strains [A(H1N1)pdm09 and A(H3N2)]and not viruses from a zoonotic source.
The World Health Organization gold standard for typing takes a more specific approach using type-, subtype-, or strain-specific antibodies and detection of their ability to inhibit virus hemagglutination of red blood cells. This assay requires a ≥ 8-fold difference in hemagglutination activity between isolates and reference strains to indicate antigenic variance of HA within strains and for identifying novel viruses or zoonotic IAV [34, 35]. However, these methods are time consuming and technically demanding, requiring banked virus isolates, antibodies, and virus culture to be conducted. The requirement of virus culture is especially challenging given the BSL3 containment requirement for suspected novel/zoonotic influenzas. Furthermore, molecular subtyping assays require periodic re-evaluation due to change in test performance (primarily sensitivity and specificity) as a result of natural genetic drift which alters HA antigenic targets. Because of these limitations, there has been an increased interest in molecular assays for typing and identifying zoonotic IAV infections in humans. Oftentimes, these molecular approaches rely on multiplexing, hybridization of specific probes, or direct sequencing of gene segments [36, 37, 38•]. Regardless of test used, results should be interpreted within context of overall setting in which infections occur, considering potential exposures with zoonotic IAV-carrying animals.
Treatment
Antiviral Medications
The two classes of drugs approved for influenza infections are adamantanes and neuraminidase inhibitors (NAI). Adamantanes such as amantadine and rimantadine block the M2 hydrogen ion channel of influenza A virus, interrupting the viral life cycle [39]. NAIs inhibit the viral NA of influenza A and B, preventing viral cleavage from host cell and subsequent spread [40]. The most widely available NAIs are oseltamivir and zanamivir, but other NAIs such as peramivir and laninamivir are licensed in a limited number of countries.
Avian Influenza A(H5N1)
Adamantanes
To date, the benefit of adamantanes for H5N1 treatment is still unclear for several reasons. First, there is a lack of randomized controlled trials (RCTs) and only a few case series are available, thus making conclusions about clinical efficacy difficult [7]. Moreover, resistance to adamantanes is widespread, mostly because of a S31N mutation in the M2 protein [41, 42], although this mutation is less widespread in Europe and some Asian countries compared to other Asian countries [43,44,45,46]. The S31N mutation does not seem to alter viral fitness, which might explain why the mutant virus has become dominant in the population without antiviral pressure [47•].
Neuraminidase Inhibitors
Because of widespread resistance to adamantanes, neuraminidase inhibitors (NAIs) have been the first-line therapy for H5N1 infection and among those, oseltamivir has been the most widely used NAI in humans. Animal data show that oseltamivir is efficient for H5N1 treatment [48]. There are no RCTs evaluating oseltamivir for H5N1 treatment and initial case series only suggested a modest reduction in mortality [49]. However, more recent data show that oseltamivir treatment is associated with a survival benefit, especially when started within the first 6–8 days after symptom onset [50, 51]. These differences in the benefit of oseltamivir might be related to the late treatment onset in early series, as a delay in treatment onset has been associated with poorer prognosis [52]. Further, another NAI, zanamivir, has been shown to be effective in vitro and in vivo against H5N1 [53]; however, there are no clinical data supporting its use.
Emergence of NAI resistance in H5N1 is a major concern. As for H1N1 (both before and after the 2009 pandemic), the H275Y mutation in the NA gene is the most common cause of NAI resistance for H5N1 [49, 53] and has been associated with fatal outcomes [49]. As observed for H1N1, the H275Y mutation in H5N1 strains confers resistance to oseltamivir but not to zanamivir [53], and limited data seem to show that zanamivir is effective in case of infection with a mutant H5N1 strain [53]. The H275Y mutation is of concern, as most seasonal A/Brisbane/59/2007(H1N1) strains acquired this mutation despite the absence of antiviral pressure, highlighting a preserved viral fitness [54]. Fortunately, viral fitness seems to be partially altered in H275Y mutant H5N1 strains [55], making the widespread emergence of H275Y H5N1 mutants without antiviral pressure less likely. Other mutations conferring resistance to a single or to multiple NAIs have been identified among H5N1 strains, although more rarely [56].
Combination Therapy
Some studies have shown that a combination of oseltamivir and amantadine with or without ribavirin provided a survival advantage in mice infected with H5N1 when compared to monotherapy [57, 58]. However, no human studies have confirmed these findings.
Recommendations
Based on the abovementioned data as well as on data extrapolated from seasonal influenza [59], the WHO strongly recommends oseltamivir as the first-line therapy in case of H5N1 infection [60, 61]. The more recent CDC guidance on novel influenza A infections also recommends NAIs to be started immediately for confirmed and probable cases, as well as for persons under investigation, even more than 48 h after symptom onset, and regardless whether patient is admitted or not [62•]. The currently recommended adult dose of oseltamivir is 75 mg twice daily for 5 days, [61, 62•] but some experts recommend to consider treating for up to 10 days with 150 mg twice daily for severely ill patients [2, 60, 62•], as human case series and animal studies have suggested that H5N1 might require higher NAI doses than other influenza strains [48, 63, 64], due to possible higher level viral replication or higher virulence. Given the lack of data about other NAIs in this context, both WHO and CDC emphasize the preference for oseltamivir compared to zanamivir [61, 62•]. The CDC also recommends maintaining a high degree of suspicion for oseltamivir resistance and considers a transition to zanamivir in case of non-response to first-line treatment [62•]. Because of widespread resistance to adamantanes, the CDC recommends against the use of adamantanes for H5N1 treatment [62•], whereas the WHO recommends using adamantanes as a first-line therapy only when neuraminidase inhibitors are not available, and especially if the virus is known or likely to be susceptible [61].
Given the lack of human data about combination therapy, the WHO weakly recommends considering a combination therapy of adamantanes and NAIs for patients with confirmed or high suspicion of H5N1, and only in the context of prospective data collection [60, 61]. Similarly, some experts consider combination therapy as a reasonable option in regions where H5N1 is likely to be susceptible to amantadine, especially in critically ill patients [2]. The CDC recommends against the combination of two NAIs [62•].
Other Agents and Emerging Therapies
Other agents with antiviral properties, such as the novel RNA polymerase inhibitor, favipiravir (T-705), sialidase fusion construct DAS181, monoclonal antibodies, convalescent plasma, interferon-gamma, and ribavirin, have been evaluated alone or in combination with NAIs for H5N1 treatment in animal or human studies [2, 65,66,67,68]. However, there is not enough data to date to firmly conclude about the usefulness of those agents. The benefit of adjunctive steroids has not yet been proven effective in animal models of H5N1 infection [69]; therefore, WHO and expert groups recommend against its routine administration and is therefore not recommended [2, 60].
Avian Influenza A(H7N9)
Adamantanes
Since the first description of human H7N9 infections in 2013, the virus harbored the S31N mutation conferring resistance to adamantanes [70, 71]. In a recent report from the WHO, the resistance to adamantanes was universal, with 100% of the 83 viruses tested carrying this mutation (WHO) [72]. For this reason, adamantanes have not been evaluated as a potential treatment for H7N9 infection.
Neuraminidase Inhibitors
Animal models suggest a benefit of oseltamivir treatment in mice infected with the H7N9 virus [73, 74]. Even if human data are scarce, it has been shown that delaying antiviral onset is associated with an increased risk of death [75], which strongly suggests a benefit of early antiviral treatment. For this reason, NAIs are the recommended first-line treatments for H7N9 infection. To date, mutations conferring resistance to NAIs seem to be relatively rare, with a rate of less than 4% according to a recent WHO report [76]. Several mutations in the H7N9 NA gene can confer resistance to one or more NAIs [77,78,79]. The R292K mutation is of particular importance because it is the most frequent mutation in group 2 NAs (including N9 but also N2), and it confers high-level resistance to oseltamivir as well as reduced sensitivity to zanamivir and peramivir [80]. Moreover, infection with the R292K mutant has been associated with worse outcome in humans [77]. Fortunately, the R292K mutant showed reduced fitness in animal and human models [14, 78, 81]. Therefore, unlike the resistance to adamantanes, it is therefore less likely to see a widespread emergence of R292K mutants in the absence of antiviral pressure.
Recommendations
The CDC recommendations for treatment of H7N9 infection are similar as those of H5N1, with oseltamivir 75 mg twice daily for 5 days as first-line therapy [62•], while further suggesting to consider treating for up to 10 days with 150 mg twice daily for severely ill patients [62•]. To date, the WHO has not issued recommendations for H7N9 treatment.
Combination Therapy, Other Agents, and Emerging Therapies
Favipiravir (T-705) seems to be effective against H7N9 in vitro and in animal models against H7N9, with some data suggesting it might have a better efficacy than NAIs [82, 83]. Other agents such as DAS181 and human or murine monoclonal antibodies have been evaluated in vitro and in animal models [84,85,86]. Moreover, a case of successful treatment of an infected human with convalescent plasma has been reported [87]. These novel treatment options as well as data about combination therapy are reviewed in more detail elsewhere [88].
Swine Influenza
Adamantanes
The 2009 A(H1N1) influenza viruses have the genetic marker (S31N in M2) for resistance to the adamantine antivirals [89]. Most variant viruses are resistant to this class [25••].
Neuraminidase Inhibitors
Variant viruses tested to date are susceptible to the neuraminidase inhibitors [25••]. A(H1N1)pdm2009 influenza viruses are sensitive to oseltamivir and zanamavir in functional assays [89]. Therefore, recommendations were made for treatment and chemoprophylaxis using oseltamivir or zanamivir [90]. Resistance to oseltamivir has been reported, as a result of the development of H275Y mutation during treatment and chemoprophylaxis [90].
Recommendations
Current CDC guidelines recommend early neuraminidase inhibitor antiviral treatment for all hospitalized patients, and for any high-risk patients with suspected or confirmed variant virus infection. Early antiviral treatment (within 48 h of illness onset) is generally most effective, though it may still be effective when administered later in patients with moderate and severe illnesses. Antivirals available include oral oseltamivir, inhaled zanamivir, and IV peramivir [25••].
Prevention Strategies
Control Within Animal Populations
Limiting the spread of zoonotic influenza viruses requires a multipronged approach to stem transmission within the zoonotic population, decrease the transmission from animals to humans, and limit transmission between humans. Limiting the spread of zoonotic influenza viruses first begins with decreasing the spread within the zoonotic population. Unfortunately, no universally effective avian or swine influenza vaccine exists, nor is there a single universal policy that would fit all situations or geographical regions [91, 92]. Ongoing surveillance and research efforts focused among countries with the highest ranking for spread and emergence of novel influenza viruses are prudent [91, 92]. Good animal health management, biosecurity, and hygiene practices are essential on farms [91]. However, efforts would also need to be implemented at other points of human-animal interface, such as live-animal markets, fairs, exhibits, and petting zoos. Therefore, eradication programs should also include increased biosecurity, extensive surveillance, and a comprehensive education program for the public [92]. Ongoing collaborations between organizations such as the World Organization for Animal Health (OIE), Food and Agriculture Organization of the United Nations (FAO), and the WHO are required to share expertise in the animal health sector with the public health sector [91].
Vaccines
Avian Influenza
The biology of avian influenza viruses presents unique challenges to the development of vaccines for human use [93]. Avian influenza viruses contain different subtypes of HA and NA glycoproteins and the genetic and antigenic diversity within each subtype resulting from various geographical lineages present innumerable potential targets for vaccine development; yet, not all strains may be of pandemic potential. In addition, the virulence of avian influenza viruses for chickens has limited the use of conventional methods for the production of vaccines from wild-type avian influenza viruses in embryonated eggs. In spite of these challenges, numerous vaccines against avian influenza viruses had been developed [2, 93]. In 2007, the US FDA approved the first H5N1 vaccine using the A/Vietnam/1203/2004 influenza strain. It was not made commercially available; however, it was reserved by the federal government for use in the event of a pandemic [90]. Subsequently, the US federal government has also maintained a stockpile of vaccines against Asian H7N9 viruses. Due to emergence of a highly pathogenic variant of H7N9 in early 2017, two additional H7N9 candidate virus vaccines were recommended for development in March, 2017 [11]. Candidate vaccine viruses continue to be made on an as-needed basis. These stockpiled vaccines could be used if similar viruses were to begin transmitting easily from person to person [94••].
Currently, the most effective way to prevent human infection with avian IAVs is to avoid sources of exposure. Bird flu viruses can enter a person’s eyes, nose, and mouth or be inhaled when the virus is in the air (in droplets or possibly dust) and the person breathes it in, or when the person touches a fomite that has the virus on it then touches their mouth, eyes, or nose. Those who work with poultry or who respond to avian influenza outbreaks are advised to follow recommended biosecurity and infection control practices. In addition to personal protective equipment and careful attention to hand hygiene, they should be monitored for illness during and after responding to avian influenza outbreaks among poultry. Though the seasonal influenza vaccination will not prevent infection with avian influenza A viruses, these people should receive a seasonal influenza vaccination every year to reduce the risk of coinfection with human and avian influenza A viruses [94••].
Swine Influenza
At the time of the 2009 pandemic, neither recent seasonal human nor swine H1N1 vaccines induced complete protection in animal models [95]. There was a lack of cross-protective immunity between the pandemic and seasonal influenza virus strains, rendering the 2009 seasonal influenza vaccine ineffective against the A(H1N1)pdm2009 virus [28]. The FDA and WHO identified A/California/07/2009 (H1N1) as the strain to be used for novel influenza A/H1N1 2009 monovalent vaccine. Manufacturers around the world developed pandemic vaccines, including inactivated whole-virion vaccines, split inactivated vaccines, subunit vaccines, and live-attenuated vaccines, including a novel type of highly attenuated influenza virus strain that is deletion of the NS1 genomic RNA segment [28]. It was shown inactivated vaccine containing 3.8 to 15 μg HA (of inactivated A(H1N1)) was able to induce potentially protective antibody levels within 2 weeks [28]. In spite of the rapid global response, it took several months to have the vaccines available. The H1N1pdm09 virus has since replaced the previously circulating human seasonal H1N1 IAV and is now the only H1N1 virus circulating in the human population. It has become the H1N1 component in the trivalent and subsequent quadrivalent human seasonal influenza vaccine since 2010 [91, 96].
Chemoprevention
Avian Influenza H5N1 Pre- and Post-Exposure Prophylaxis
As for influenza treatment, influenza chemoprevention relies mostly on NAIs. There is no data about the use of adamantanes for prophylaxis against H5N1. However, based on data extrapolated from seasonal influenza [59], adamantanes might have a clinical benefit in this setting. However, given the high rate of H5N1 resistance to adamantanes, the WHO recommends to use adamantanes for prophylaxis in high- and moderate-risk groups only when NAIs are not available and when the virus is known or likely to be susceptible [61]. The WHO does not recommend the use of adamantanes for prophylaxis in low-risk groups, regardless of viral susceptibility [61]. Interestingly, adamantanes are not mentioned in the CDC recommendations for prophylaxis [97••]. However, given the fact that CDC recommends against the use of adamantanes for H5N1 treatment because of widespread resistance [62•], one can infer that this antiviral class should not be used for prophylaxis either. Oseltamivir has been shown to be effective as a pre- and post-exposure prophylaxis against H5N1 in animal models [48, 63, 98], but human data are lacking. Data are even scarcer for zanamivir. Based on the evidence of efficacy as post-exposure prophylaxis for seasonal influenza in humans [59], the WHO recommends oseltamivir (or alternatively zanamivir) as a first-line prophylaxis; recommendations were strong in high-risk exposure groups (such as household or close family contacts of a strongly suspected or confirmed H5N1 patient), weak in moderate-risk groups (such as individuals with unprotected, inadequate, or very close contact with sick or dead H5N1-infected animals and healthcare workers in close contact with strongly suspected or confirmed H5N1 patients regardless of adequate protective personal equipment), and oseltamivir was not recommended in lower risk groups [61]. The more recent CDC guidance recommends that close contacts of patients infected with H5N1 should receive oseltamivir or zanamivir if they belong to high-risk exposure groups, whereas prophylaxis should be considered for moderate-risk groups and is not recommended for low-risk groups [97••]. In case of exposure to birds with avian influenza, the CDC recommends considering post-exposure prophylaxis in every exposed patient, based on exposure type and category risk [99]. In the historical WHO recommendations, prophylaxis dose was 75 mg once daily—half the treatment dose as soon as exposure is identified and until 7–10 days after last exposure [61]. However, the more recent CDC recommendations currently suggest using the treatment dose of 75 mg twice daily for 5 days from the last exposure in case of time-limited exposure, and 10 days in case of ongoing exposure [97••, 99].
Avian Influenza H7N9 Pre- and Post-Exposure Prophylaxis
Adamantanes should not be used as prophylaxis because of universal resistance [72]. For NAIs, data are even scarcer for prophylaxis than for treatment. Public Health England (PHE) recommends prophylaxis for close contacts of confirmed H7N9 cases [100]; whereas, the CDC advises that prophylaxis should be administered for high-risk exposure groups (household/close family member contact of a confirmed/probable case), considered for moderate-risk (healthcare personnel with unprotected close contact with a confirmed/probable case), and should not be recommended for low-risk groups [97••]. In case of exposure to infected birds, the CDC recommends considering post-exposure prophylaxis in every exposed patient, based on exposure type and category risk [99]. Interestingly, the WHO does not recommend routine post-exposure prophylaxis after exposure to a patient with confirmed H7N9 infection or infected poultry [101]. It recommends considering prophylaxis in high-risk exposures and to empirically treat if an exposed person develops respiratory symptoms, pending investigations results. Regardless of the eligibility criteria for prophylaxis, PHE, WHO, and CDC recommend that oseltamivir prophylaxis be given at a dose of 75 mg twice daily for 5 days [97••, 100, 101], although the CDC recommends a 10-day course in the case of ongoing exposure [97••].
Swine Influenza Pre-Exposure Prophylaxis
Current CDC guidelines do not recommend the use of antiviral chemoprophylaxis before or after swine exposure, including for persons who are at high risk for influenza complications. Given most cases of variant influenza are sporadic and without sustainable person-to-person spread, the use of antivirals for chemoprophylaxis follows recommendations for seasonal influenza [25••].
Infection Control for Zoonotic Influenza Infections
Avian Influenza
Current infection control recommendations for avian influenza A (H7N9), H5N1, and newly detected avian influenza H5 viruses (H5N2, H5N8, and the reassortant H5N1 virus) are encompassed in guidelines for initial infection control in healthcare settings for patients who may be infected with a novel influenza A virus associated with severe disease. Due to a lack of a widely available safe and effective vaccine and the suspected high rate of morbidity and mortality among infected patients, a higher level of infection control measures is undertaken compared to seasonal influenza. These include the addition of airborne precautions to standard and droplet/contact precautions, such as the expanded use of respirators for all patient-care activities [102, 103].
Swine Influenza
Given the assumption that swine influenza viruses can be transmitted from person-to-person and cause disease of similar severity to seasonal IAV, infection control recommendations in healthcare settings would be the same as those for seasonal influenza. These would include standard and droplet/contact precautions [25••, 104]. Additionally, for aerosol-generating procedures, the use of a fit-tested N95 respiratory or equivalent has been advocated [25••].
Summary
In summary, illness caused by zoonotic influenza viruses can range from a minor illness with primarily respiratory manifestations to severe multiorgan dysfunction resulting in death. The case fatality rates can be as high as 60%, as observed in avian influenza A (H5N1) infections. While the two classes of drugs approved for influenza infections, the adamantanes and the NAIs, are available to potentially combat these threats, several of the novel viruses may be intrinsically resistant to these drugs, especially the adamantanes. For most zoonotic influenza viruses, neuraminidase inhibitors comprise the backbone of antiviral treatment, which is complemented by supportive care. Because influenza A viruses contain different subtypes of HA and NA glycoproteins, and further possess great genetic and antigenic diversity within each subtype, they present numerous challenges for vaccine development. Recent focus has shifted to development of universal influenza vaccines, with the aim to provide protection regardless of influenza A subtype by targeting the HA stalk which is common to multiple subtypes. The most effective way to prevent human infection with zoonotic influenza viruses is the avoidance of sources of exposure. Containing the spread of these viruses requires a multipronged approach to stem the spread within the zoonotic populations, decrease the transmission from animals to humans, and limit transmission between humans. Although today we are better prepared to face a new influenza pandemic and to limit the burden of zoonotic, pandemic, and seasonal influenza than ever before, continued effort is warranted to build on this knowledge such that we can efficiently combat the constant threat these viruses pose.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kandun IN, Wibisono H, Sedyaningsih ER, Yusharmen, Hadisoedarsuno W, Purba W, et al. Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med. 2006;355(21):2186–94. https://doi.org/10.1056/NEJMoa060930.
Writing Committee of the Second World Health Organization Consultation on Clinical Aspects of Human Infection with Avian Influenza A (H5N1) Virus, Abdel-Ghafar A-N, Chotpitayasunondh T, et al. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008;358(3):261–73. https://doi.org/10.1056/NEJMra0707279.
Centers for Disease Control and Prevention (CDC). Highly pathogenic Asian avian influenza A (H5N1) in people. Avian Influenza (Flu). Available at https://www.cdc.gov/flu/avianflu/h5n1-people.htm Accessed 22 April 2018.
Liem NT, Tung CV, Hien ND, Hien TT, Chau NQ, Long HT, et al. Clinical features of human influenza A (H5N1) infection in Vietnam: 2004–2006. Clin Infect Dis. 2009;48(12):1639–46. https://doi.org/10.1086/599031.
Chotpitayasunondh T, Ungchusak K, Hanshaoworakul W, Chunsuthiwat S, Sawanpanyalert P, Kijphati R, et al. Human disease from influenza A (H5N1), Thailand, 2004. Emerg Infect Dis. 2005;11(2):201–9. https://doi.org/10.3201/eid1102.041061.
Kawachi S, Luong ST, Shigematsu M, Furuya H, Phung TTB, Phan PH, et al. Risk parameters of fulminant acute respiratory distress syndrome and avian influenza (H5N1) infection in Vietnamese children. J Infect Dis. 2009;200(4):510–5. https://doi.org/10.1086/605034.
Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353(13):1374–85. https://doi.org/10.1056/NEJMra052211.
Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet (London, England). 2004;363(9409):617–9. https://doi.org/10.1016/S0140-6736(04)15595-5.
To KF, Chan PK, Chan KF, et al. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J Med Virol. 2001;63(3):242–6. https://doi.org/10.1002/1096-9071(200103)63:3<242::AID-JMV1007>3.0.CO;2-N.
World Health Organization. Overview of the emergence and characteristics of the avian influenza A ( H7N9 ) virus. WHO Rep. 2013;(May):1–38.
World Health Organization. Human cases of influenza at the human-animal interface, January 2015 – April 2017 – Cas humains de grippe à l’interface homme-animal, janvier 2015-avril 2017. Wkly Epidemiol Rec 2017;92(33):460–475.
World Health Organization. Influenza at the human-animal interface. Available at http://www.who.int/influenza/human_animal_interface/en/ Accessed 22 April 2018.
Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet. 2013;381(9881):1916–25. https://doi.org/10.1016/S0140-6736(13)60903-4.
Yen HL, Zhou J, Choy KT, Sia SF, Teng O, Ng IH, et al. The R292K mutation that confers resistance to neuraminidase inhibitors leads to competitive fitness loss of A/Shanghai/1/2013 (H7N9) influenza virus in ferrets. J Infect Dis. 2014;210(12):1900–8. https://doi.org/10.1093/infdis/jiu353.
Gao HN, Lu HZ, Cao B, du B, Shang H, Gan JH, et al. Clinical findings in 111 cases of influenza A (H7N9) virus infection. N Engl J Med. 2013;368(24):2277–85. https://doi.org/10.1056/NEJMoa1305584.
Wang C, Yu H, Horby PW, Cao B, Wu P, Yang S, et al. Comparison of patients hospitalized with influenza a subtypes H7N9, H5N1, and 2009 pandemic H1N1. Clin Infect Dis. 2014;58(8):1095–103. https://doi.org/10.1093/cid/ciu053.
Li Q, Zhou L, Zhou M, Chen Z, Li F, Wu H, et al. Epidemiology of human infections with avian influenza A(H7N9) virus in China. N Engl J Med. 2014;370(6):520–32. https://doi.org/10.1056/NEJMoa1304617.
Centers for Disease Control and Prevention (CDC). Asian lineage avian influenza A (H7N9) virus. Avian Influenza (Flu). Available at https://www.cdc.gov/flu/avianflu/h7n9-virus.htm. Accessed 22 April 2018.
Centers for Disease Control and Prevention (CDC). Notes from the field: highly pathogenic avian influenza A (H7N3) virus infection in two poultry workers—Jalisco, Mexico, July 2012. MMWR Morb Mortal Wkly Rep. 2012;61(36):726–7.
Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet (London, England). 2004;363(9409):587–93. https://doi.org/10.1016/S0140-6736(04)15589-X.
Fouchier RA, Schneeberger PM, Rozendaal FW, et al. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci U S A. 2004;101(5):1356–61. https://doi.org/10.1073/pnas.0308352100.
Peiris M, Yuen KY, Leung CW, Chan KH, Ip PLS, Lai RWM, et al. Human infection with influenza H9N2. Lancet. 1999;354(9182):916–7. https://doi.org/10.1016/S0140-6736(99)03311-5.
•• World Health Organization. Human infection with avian influenza A(H7N4) virus—China. WHO. 2018. Available at http://www.who.int/csr/don/22-february-2018-ah7n4-china/en/. Accessed April 15, 2018. This reference describes the first case of human infection with avian influenza A(H7N4) virus detected in China.
Myers KP, Olsen CW, Gray GC. Cases of swine influenza in humans: a review of the literature. Clin Infect Dis. 2007;44(8):1084–8. https://doi.org/10.1086/512813.
•• Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Variant virus infections in people interim guidance for clinicians. Available at https://www.cdc.gov/flu/swineflu/interim-guidance-variant-flu.htm. Accessed 22 April 2018. This reference describes the clinical presentation, risk groups, diagnostic criteria, and clinical management of influenza A viruses circulating in swine that have infected humans.
Brockwell-Staats C, Webster RG, Webby RJ. Diversity of influenza viruses in swine and the emergence of a novel human pandemic influenza A (H1N1). Influenza Other Respir Viruses. 2009;3(5):207–13. https://doi.org/10.1111/j.1750-2659.2009.00096.x.
Cheng VC, To KK, Tse H, Hung IF, Yuen KY. Two years after pandemic influenza a/2009/H1N1: what have we learned? Clin Microbiol Rev. 2012;25(2):223–63. https://doi.org/10.1128/CMR.05012-11.
Girard MP, Tam JS, Assossou OM, Kieny MP. The 2009 A (H1N1) influenza virus pandemic: a review. Vaccine. 2010;28(31):4895–902. https://doi.org/10.1016/J.VACCINE.2010.05.031.
Zitterkopf NL, Leekha S, Espy MJ, Wood CM, Sampathkumar P, Smith TF. Relevance of influenza A virus detection by PCR, shell vial assay, and tube cell culture to rapid reporting procedures. J Clin Microbiol. 2006;44(9):3366–7. https://doi.org/10.1128/JCM.00314-06.
Iovine NM, Ison T, Payton T, Morris JG Jr, Rand K. High percentage of false-positive results for influenza B obtained with a rapid influenza point-of-care test. Clin Infect Dis 2014;59(4):604–605. doi:https://doi.org/10.1093/cid/ciu315.
• Hurtado JC, Mosquera MM, de Lazzari E, Martínez E, Torner N, Isanta R, et al. Evaluation of a new, rapid, simple test for the detection of influenza virus. BMC Infect Dis. 2015;15(1):44. https://doi.org/10.1186/s12879-015-0775-5. This reference describes the performance of a rapid diagnostic test for the detection of the influenza virus.
Salez N, Nougairede A, Ninove L, Zandotti C, de Lamballerie X, Charrel RN. Xpert Flu for point-of-care diagnosis of human influenza in industrialized countries. Expert Rev Mol Diagn. 2014;14(4):411–8. https://doi.org/10.1586/14737159.2014.901152.
Chan KH, To KK, Chan JF, Li CP, Chen H, Yuen KY. Analytical sensitivity of seven point-of-care influenza virus detection tests and two molecular tests for detection of avian origin H7N9 and swine origin H3N2 variant influenza a viruses. J Clin Microbiol. 2013;51(9):3160–1. https://doi.org/10.1128/JCM.01222-13.
Centers for Disease Control and Prevention (CDC). Antigenic characterization | seasonal influenza (flu). CDC. Available at https://www.cdc.gov/flu/professionals/laboratory/antigenic.htm. Accessed April 22, 2018.
Katz JM, Hancock K, Xu X. Serologic assays for influenza surveillance, diagnosis and vaccine evaluation. Expert Rev Anti-Infect Ther. 2011;9(6):669–83. https://doi.org/10.1586/eri.11.51.
Tseng CH, Tsai HJ, Chang CM. A complete molecular diagnostic procedure for applications in surveillance and subtyping of avian influenza virus. Biomed Res Int. 2014;2014:1–7. https://doi.org/10.1155/2014/653056.
Wang R, Taubenberger JK. Methods for molecular surveillance of influenza. Expert Rev Anti-Infect Ther. 2010;8(5):517–27. https://doi.org/10.1586/eri.10.24.
• Vemula S, Zhao J, Liu J, Wang X, Biswas S, Hewlett I. Current approaches for diagnosis of influenza virus infections in humans. Viruses. 2016;8(4):96. https://doi.org/10.3390/v8040096. This reference is a good resource for information regarding the current approaches for diagnosis of influenza virus infections in humans.
Wang C, Takeuchi K, Pinto LH, Lamb RA. Ion channel activity of influenza A virus M2 protein: characterization of the amantadine block. J Virol. 1993;67(9):5585–94.
Colman PM. Influenza virus neuraminidase: structure, antibodies, and inhibitors. Protein Sci. 1994;3(10):1687–96. https://doi.org/10.1002/pro.5560031007.
Cheung CL, Rayner JM, Smith GJ, et al. Distribution of amantadine-resistant H5N1 avian influenza variants in Asia. J Infect Dis. 2006;193(12):1626–9. https://doi.org/10.1086/504723.
Hill AW, Guralnick RP, Wilson MJ, Habib F, Janies D. Evolution of drug resistance in multiple distinct lineages of H5N1 avian influenza. Infect Genet Evol. 2009;9(2):169–78. https://doi.org/10.1016/j.meegid.2008.10.006.
Jacob A, Sood R, Chanu KV, Bhatia S, Khandia R, Pateriya AK, et al. Amantadine resistance among highly pathogenic avian influenza viruses (H5N1) isolated from India. Microb Pathog. 2016;91:35–40. https://doi.org/10.1016/j.micpath.2015.11.008.
Li KS, Guan Y, Wang J, Smith GJD, Xu KM, Duan L, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430(6996):209–13. https://doi.org/10.1038/nature02746.
Puthavathana P, Auewarakul P, Charoenying PC, et al. Molecular characterization of the complete genome of human influenza H5N1 virus isolates from Thailand. J Gen Virol. 2005;86(2):423–33. https://doi.org/10.1099/vir.0.80368-0.
Chen H, Smith GJ, Li KS, et al. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc Natl Acad Sci. 2006;103(8):2845–50. https://doi.org/10.1073/pnas.0511120103.
• Abdelwhab EM, Veits J, Mettenleiter TC. Biological fitness and natural selection of amantadine resistant variants of avian influenza H5N1 viruses. Virus Res. 2017;228:109–13. https://doi.org/10.1016/j.virusres.2016.11.032. This article shows that the S31N mutation conferring resistance to adamantanes does not seem to alter viral fitness in H5N1 in vitro, which likely explains why the mutant virus has become dominant despite the absence of antiviral pressure.
Govorkova EA, Ilyushina NA, Boltz DA, Douglas A, Yilmaz N, Webster RG. Efficacy of oseltamivir therapy in ferrets inoculated with different clades of H5N1 influenza virus. Antimicrob Agents Chemother. 2007;51(4):1414–24. https://doi.org/10.1128/AAC.01312-06.
de Jong MD, Tran TT, Truong HK, et al. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N Engl J Med. 2005;353(25):2667–72. https://doi.org/10.1056/NEJMoa054512.
Adisasmito W, Chan PK, Lee N, et al. Effectiveness of antiviral treatment in human influenza A(H5N1) infections: analysis of a global patient registry. J Infect Dis. 2010;202(8):1154–60. https://doi.org/10.1086/656316.
Chan PK, Lee N, Zaman M, et al. Determinants of antiviral effectiveness in influenza virus a subtype H5N1. J Infect Dis. 2012;206(9):1359–66. https://doi.org/10.1093/infdis/jis509.
Gambotto A, Barratt-Boyes SM, de Jong MD, Neumann G, Kawaoka Y. Human infection with highly pathogenic H5N1 influenza virus. Lancet. 2008;371(9622):1464–75. https://doi.org/10.1016/S0140-6736(08)60627-3.
Le QM, Kiso M, Someya K, et al. Avian flu: isolation of drug-resistant H5N1 virus. Nature. 2005;437(7062):1108. https://doi.org/10.1038/4371108a.
Moscona A. Global transmission of oseltamivir-resistant influenza. N Engl J Med. 2009;360(10):953–6. https://doi.org/10.1056/NEJMp0900648.
Govorkova EA, Ilyushina NA, Marathe BM, McClaren JL, Webster RG. Competitive fitness of oseltamivir-sensitive and -resistant highly pathogenic H5N1 influenza viruses in a ferret model. J Virol. 2010;84(16):8042–50. https://doi.org/10.1128/JVI.00689-10.
Nguyen HT, Nguyen T, Mishin VP, Sleeman K, Balish A, Jones J, et al. Antiviral susceptibility of highly pathogenic avian influenza A(H5N1) viruses isolated from poultry, Vietnam, 2009–2011. Emerg Infect Dis. 2013;19(12):1963–71. https://doi.org/10.3201/eid1912.130705.
Ilyushina NA, Hoffmann E, Salomon R, Webster RG, Govorkova EA. Amantadine-oseltamivir combination therapy for H5N1 influenza virus infection in mice. Antivir Ther. 2007;12(3):363–70.
Nguyen JT, Smee DF, Barnard DL, Julander JG, Gross M, de Jong MD, Went GT. Efficacy of combined therapy with amantadine, oseltamivir, and ribavirin in vivo against susceptible and amantadine-resistant influenza a viruses. Pekosz A, ed. PLoS One 2012;7(1): e31006. https://doi.org/10.1371/journal.pone.0031006.
Jefferson T, Demicheli V, Rivetti D, Jones M, Di Pietrantonj C, Rivetti A. Antivirals for influenza in healthy adults: systematic review. Lancet (London, England). 2006;367(9507):303–13. https://doi.org/10.1016/S0140-6736(06)67970-1.
World Health Organization. Clinical management of human infection with avian influenza A (H5N1) virus. Available at http://www.who.int/influenza/resources/documents/clinical_management_h5n1_15_08_2007/en/ Accessed April 22, 2018.
Schünemann HJ, Hill SR, Kakad M, Bellamy R, Uyeki TM, Hayden FG, et al. WHO Rapid Advice Guidelines for pharmacological management of sporadic human infection with avian influenza A (H5N1) virus. Lancet Infect Dis. 2007;7(1):21–31. https://doi.org/10.1016/S1473-3099(06)70684-3.
• Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Interim guidance on the use of antiviral medications for treatment of human infections with novel influenza A viruses associated with severe human disease. Avian Influenza (Flu). Available at https://www.cdc.gov/flu/avianflu/novel-av-treatment-guidance.htm. Accessed 22 April 2018. This reference enlists the CDC’s interim guidance on the use of antiviral medications for treatment of human infections with novel influenza A viruses associated with severe human disease.
Yen HL, Monto AS, Webster RG, Govorkova EA. Virulence may determine the necessary duration and dosage of oseltamivir treatment for highly pathogenic A/Vietnam/1203/04 influenza virus in mice. J Infect Dis. 2005;192(4):665–72. https://doi.org/10.1086/432008.
McKimm-Breschkin JL, Selleck PW, Usman TB, Johnson MA. Reduced sensitivity of influenza A to oseltamivir. Emerg Infect Dis. 2007;13(9):1354–7. https://doi.org/10.3201/eid1309.070164.
Marathe BM, Wong SS, Vogel P, Garcia-Alcalde F, Webster RG, Webby RJ, et al. Combinations of oseltamivir and T-705 extend the treatment window for highly pathogenic influenza a (H5N1) virus infection in mice. Sci Rep. 2016;6(1):26742. https://doi.org/10.1038/srep26742.
Herbreteau CH, Denizot M, Lowther S, Riddell S, Frazer L, Haining J, et al. Efficacy of a specific polyclonal equine F(ab’) 2 against avian influenza (H5N1) in ferrets: synergy with oseltamivir. Immunotherapy. 2016;8(9):1021–32. https://doi.org/10.2217/imt-2016-0062.
Bal C, Herbreteau CH, Buchy P, Rith S, Zaid M, Kristanto W, et al. Safety, potential efficacy, and pharmacokinetics of specific polyclonal immunoglobulin F(ab’)2 fragments against avian influenza A (H5N1) in healthy volunteers: a single-centre, randomised, double-blind, placebo-controlled, phase 1 study. Lancet Infect Dis. 2015;15(3):285–92. https://doi.org/10.1016/S1473-3099(14)71072-2.
Haasbach E, Droebner K, Vogel AB, Planz O. Low-dose interferon type I treatment is effective against H5N1 and swine-origin H1N1 influenza A viruses in vitro and in vivo. J Interf Cytokine Res. 2011;31(6):515–25. https://doi.org/10.1089/jir.2010.0071.
Pu L, Jiang T, Liu JY, Deng YQ, Wang P, Nian QG, et al. Methylprednisolone treatment fails to protect mice from the H5N1 influenza A virus-induced proinflammatory response and mortality. J Inf Secur. 2014;69(3):297–9. https://doi.org/10.1016/j.jinf.2014.03.014.
Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368(20):1888–97. https://doi.org/10.1056/NEJMoa1304459.
Liu Q, Lu L, Sun Z, Chen GW, Wen Y, Jiang S. Genomic signature and protein sequence analysis of a novel influenza A(H7N9) virus that causes an outbreak in humans in China. Microbes Infect. 2013;15(6–7):432–9. https://doi.org/10.1016/j.micinf.2013.04.004.
World Health Organization. Analysis of recent scientific information on avian influenza A(H7N9) virus. Available at http://www.who.int/influenza/human_animal_interface/avian_influenza/riskassessment_AH7N9_201702/en/ Accessed 22 April 2018.
Xu L, Bao L, Li F, Gu S, Lv Q, Yuan J, et al. Combinations of oseltamivir and fibrates prolong the mean survival time of mice infected with the lethal H7N9 influenza virus. J Gen Virol. 2015;96(1):46–51. https://doi.org/10.1099/vir.0.069799-0.
Baranovich T, Burnham AJ, Marathe BM, Armstrong J, Guan Y, Shu Y, et al. The neuraminidase inhibitor oseltamivir is effective against A/Anhui/1/2013 (H7N9) influenza virus in a mouse model of acute respiratory distress syndrome. J Infect Dis. 2014;209(9):1343–53. https://doi.org/10.1093/infdis/jit554.
Wang X, Jiang H, Wu P, Uyeki TM, Feng L, Lai S, et al. Epidemiology of avian influenza A H7N9 virus in human beings across five epidemics in mainland China, 2013–17: an epidemiological study of laboratory-confirmed case series. Lancet Infect Dis. 2017;17(8):822–32. https://doi.org/10.1016/S1473-3099(17)30323-7.
World Health Organization. WHO risk assessment. Human infections with avian influenza A(H7N9) virus summary of surveillance and investigation findings. 2014. Available at http://www.who.int/influenza/human_animal_interface/influenza_h7n9/riskassessment_h7n9_2Oct14.pdf Accessed April 22 2018.
Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet. 2013;381(9885):2273–9. https://doi.org/10.1016/S0140-6736(13)61125-3.
Marjuki H, Mishin VP, Chesnokov AP, Jones J, de la Cruz JA, Sleeman K, et al. Characterization of drug-resistant influenza a(H7N9) variants isolated from an oseltamivir-treated patient in Taiwan. J Infect Dis. 2015;211(2):249–57. https://doi.org/10.1093/infdis/jiu447.
Zhang X, Song Z, He J, Yen HL, Li J, Zhu Z, et al. Drug susceptibility profile and pathogenicity of H7N9 influenza virus (Anhui1 lineage) with R292K substitution. Emerg Microbes Infect. 2014;3(11):e78. https://doi.org/10.1038/emi.2014.80.
Hay AJ, Hayden FG. Oseltamivir resistance during treatment of H7N9 infection. Lancet. 2013;381(9885):2230–2. https://doi.org/10.1016/S0140-6736(13)61209-X.
Sleeman K, Guo Z, Barnes J, Shaw M, Stevens J, Gubareva LV. R292K substitution and drug susceptibility of influenza A(H7N9) viruses. Emerg Infect Dis. 2013;19(9):1521–4. https://doi.org/10.3201/eid1909.130724.
Cao RY, Xiao JH, Cao B, Li S, Kumaki Y, Zhong W. Inhibition of novel reassortant avian influenza H7N9 virus infection in vitro with three antiviral drugs, oseltamivir, peramivir and favipiravir. Antivir Chem Chemother. 2014;23(6):237–40. https://doi.org/10.3851/IMP2672.
Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, et al. Characterization of H7N9 influenza A viruses isolated from humans. Nature. 2013;501(7468):551–5. https://doi.org/10.1038/nature12392.
Marjuki H, Mishin VP, Chesnokov AP, de la Cruz JA, Fry AM, Villanueva J, et al. An investigational antiviral drug, DAS181, effectively inhibits replication of zoonotic influenza a virus subtype H7N9 and protects mice from lethality. J Infect Dis. 2014;210(3):435–40. https://doi.org/10.1093/infdis/jiu105.
Tharakaraman K, Subramanian V, Viswanathan K, Sloan S, Yen HL, Barnard DL, et al. A broadly neutralizing human monoclonal antibody is effective against H7N9. Proc Natl Acad Sci. 2015;112(35):10890–5. https://doi.org/10.1073/pnas.1502374112.
Wilson JR, Guo Z, Reber A, Kamal RP, Music N, Gansebom S, et al. An influenza A virus (H7N9) anti-neuraminidase monoclonal antibody with prophylactic and therapeutic activity in vivo. Antivir Res. 2016;135:48–55. https://doi.org/10.1016/j.antiviral.2016.10.001.
Wu XX, Gao HN, Wu HB, Peng XM, Ou HL, Li LJ. Successful treatment of avian-origin influenza A (H7N9) infection using convalescent plasma. Int J Infect Dis. 2015;41:3–5. https://doi.org/10.1016/j.ijid.2015.10.009.
Danqi B, Li Z, Liu Q, Richt JA. H7N9 avian influenza A virus in China: a short report on its circulation, drug resistant mutants and novel antiviral drugs. Expert Rev Anti-Infect Ther. 2017;15(8):723–7. https://doi.org/10.1080/14787210.2017.1353419.
Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science (80-). 2009;325(5937):197–201. https://doi.org/10.1126/science.1176225.
Sym D, Patel PN, Ei-Chaar GM, El-Chaar GM. Seasonal, avian, and novel H1N1 influenza: prevention and treatment modalities. Ann Pharmacother. 2009;43(12):2001–11. https://doi.org/10.1345/aph.1M557.
Vincent AL, Awada L, Brown I, Chen H, Claes F, Dauphin G, et al. Review of influenza A virus in swine worldwide: a call for increased surveillance and research. Zoonoses Public Health. 2014;61(1):4–17. https://doi.org/10.1111/zph.12049.
Peyre M, Fusheng G, Desvaux S, Rorger F. Avian influenza vaccines: a practical review in relation to their application in the field with a focus on the Asian experience. Epidemiol Infect. 2009;137(1):1–21. https://doi.org/10.1017/S0950268808001039.
Subbarao K, Joseph T. Scientific barriers to developing vaccines against avian influenza viruses. Nat Rev Immunol. 2007;7(4):267–78. https://doi.org/10.1038/nri2054.
•• Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Prevention and treatment of avian influenza A viruses in people | Avian Influenza (Flu). Available at https://www.cdc.gov/flu/avianflu/prevention.htm. Accessed 22 April 2018. This reference from the Centers for Disease Control and Prevention (CDC) provides recommendations for prophylaxis and treatment of avian influenza A.
Pascua PNQ, Song M-S, Lee JH, Park KJ, Kwon HI, Baek YH, Hong SP, Rho JB, Kim CJ, Poo H, Ryoo TS, Sung MH, Choi YK Evaluation of the efficacy and cross-protectivity of recent human and swine vaccines against the pandemic (H1N1) 2009 virus infection. Sommer P, ed. PLoS One. 2009;4(12): e8431. https://doi.org/10.1371/journal.pone.0008431.
Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Bresee JS, Fry AM, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices—United States, 2017–18 influenza season. MMWR Recomm Reports. 2017;66(2):1–20. https://doi.org/10.15585/mmwr.rr6602a1.
•• Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Interim guidance on follow-up of close contacts of persons infected with novel influenza A viruses associated with severe human disease and on the use of antiviral medications for chemoprophylaxis. Available at https://www.cdc.gov/flu/avianflu/novel-av-chemoprophylaxis-guidance.htm. Accessed 22 April 2018. This reference from the CDC provides chemoprophylaxis recommendations for close contact of persons infected with novel influenza A viruses.
Boltz DA, Rehg JE, McClaren J, Webster RG, Govorkova EA. Oseltamivir prophylactic regimens prevent H5N1 influenza morbidity and mortality in a ferret model. J Infect Dis. 2008;197(9):1315–23. https://doi.org/10.1086/586711.
Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Interim guidance on influenza antiviral chemoprophylaxis of persons exposed to birds with avian influenza A viruses associated with severe human disease or with the potential to cause severe human disease. Available at https://www.cdc.gov/flu/avianflu/guidance-exposed-persons.htm. Accessed 22 April 2018.
Centers for Disease Control and Prevention. Interim guidance on follow-up of close contacts of persons infected with novel influenza A viruses associated with severe human disease and on the use of antiviral medications for chemoprophylaxis. Available at https://www.cdc.gov/flu/avianflu/novel-av-chemoprophylaxis-guidance.htm. Accessed 22 April 2018.
World Health Organization. Avian influenza A(H7N9) virus: post-exposure antiviral chemoprophylaxis of close contacts of a patient with confirmed H7N9 virus infection and/or high risk poultry/environmental exposures. Available at http://www.who.int/influenza/human_animal_interface/influenza_h7n9/13_January_2013_PEP_recs.pdf. Accessed 22 April 2018.
Centers for Disease Control and Prevention (National Center for Immunization and Respiratory Diseases). Interim guidance for infection control within healthcare settings when caring for confirmed cases, probable cases, and cases under investigation for infection with novel influenza A viruses associated with severe disease. Available at https://www.cdc.gov/flu/avianflu/novel-flu-infection-control.htm. Accessed 22 April 2018.
Government of Ontario (Ministry of Health and Long-Term Care). Guidance for health workers and health sector employers - avian influenza - emergency planning and preparedness - programs and services - health care professionals - MOHLTC. Available at http://www.health.gov.on.ca/en/pro/programs/emb/avian/workers.aspx. Accessed 22 April 2018.
Ontario Agency for Health Protection and Promotion PIDAC. Annex B: best practices for prevention of transmission of acute respiratory infection disclaimer for best practice documents. Toronto, Ontario: Queen’s Printer for Ontario; 2013. Available at https://www.publichealthontario.ca/en/eRepository/PIDAC-IPC_Annex_B_Prevention_Transmission_ARI_2013.pdf. Accessed 22 April 2018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Tropical, Travel and Emerging Infections
Rights and permissions
About this article
Cite this article
Mehta, K., Goneau, L.W., Wong, J. et al. Zoonotic Influenza and Human Health—Part 2: Clinical Features, Diagnosis, Treatment, and Prevention Strategies. Curr Infect Dis Rep 20, 38 (2018). https://doi.org/10.1007/s11908-018-0643-8
Published:
DOI: https://doi.org/10.1007/s11908-018-0643-8