Abstract
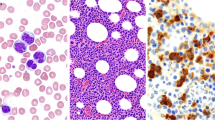
Patients with the myelodysplastic syndromes/myeloproliferative neoplasm (MDS/MPN) overlap, including chronic myelomonocytic leukemia (CMML), atypical chronic myeloid leukemia (aCML), MDS/MPN-unclassifiable (MDS/MPN-U), and refractory anemia with ring sideroblasts associated with marked thrombocytosis (RARS-T), often present with findings of both dysplasia and marrow proliferation, occupying the border region of two seemingly divergent camps. Historically, these disorders which have been lumped with either MDS or MPN have represented a minority, or been excluded all together, from the development of prognostic models and clinical trials. Therefore, Food and Drug Administration approved therapies specifically for overlap subtypes are lacking. More recently, the revolution in molecular genetics has led to discovery of mutations enacting pathways that result in the distinct biology and presentation of the overlap syndromes. Additionally, these recurrent genetic lesions have a prognostic value and are potential therapeutic targets, which might ultimately improve patient outcomes by reducing disease-related symptoms and complications and by prolonging survival.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cash J. I walk the line. With his hot and blue guitar. Nashville: Sun Records; 1955.
Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114(5):937–51.
Swerdlow S, Campo E, Harris NL, Jaffe E, Pileri S, Stein H. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: International Agency for Research on Cancer; 2008.
Strom SS, Gu Y, Gruschkus SK, Pierce SA, Estey EH. Risk factors of myelodysplastic syndromes: a case-control study. Leukemia. 2005;19(11):1912–8.
Surveillance, Epidemiology, and End Results (SEER) Program (2000–2012). In: National Cancer Institute D, Surveillance Research Program, Surveillance Systems Branch, editor. Vol. 2014; 2014.
Osca-Gelis G, Puig-Vives M, Saez M, Gallardo D, Lloveras N, Marcos-Gragera R. Population-based incidence of myeloid malignancies: fifteen years of epidemiological data in the province of Girona, Spain. Haematologica. 2013;98(8):e95–7.
Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100(7):2292–302.
Beran M, Wen S, Shen Y, et al. Prognostic factors and risk assessment in chronic myelomonocytic leukemia: validation study of the M.D. Anderson Prognostic Scoring System. Leuk Lymphoma. 2007;48(6):1150–60.
Onida F, Kantarjian HM, Smith TL, et al. Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood. 2002;99(3):840–9.
Pulliam-Leath AC, Ciccone SL, Nalepa G, et al. Genetic disruption of both Fancc and Fancg in mice recapitulates the hematopoietic manifestations of Fanconi anemia. Blood. 2010;116(16):2915–20.
Walter RB, Gyurkocza B, Storer BE, et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative allogeneic hematopoietic cell transplantation. Leukemia. 2014.
Costa R, Abdulhaq H, Haq B, et al. Activity of azacitidine in chronic myelomonocytic leukemia. Cancer. 2011;117(12):2690–6.
Wijermans PW, Ruter B, Baer MR, Slack JL, Saba HI, Lubbert M. Efficacy of decitabine in the treatment of patients with chronic myelomonocytic leukemia (CMML). Leuk Res. 2008;32(4):587–91.
Wijermans P, Lubbert M, Verhoef G, et al. Low-dose 5-aza-2′-deoxycytidine, a DNA hypomethylating agent, for the treatment of high-risk myelodysplastic syndrome: a multicenter phase II study in elderly patients. J Clin Oncol. 2000;18(5):956–62.
Aribi A, Borthakur G, Ravandi F, et al. Activity of decitabine, a hypomethylating agent, in chronic myelomonocytic leukemia. Cancer. 2007;109(4):713–7.
Braun T, Itzykson R, Renneville A, et al. Molecular predictors of response to decitabine in advanced chronic myelomonocytic leukemia: a phase 2 trial. Blood. 2011;118(14):3824–31.
Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88.
Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65.
Such E, Germing U, Malcovati L, et al. Development and validation of a prognostic scoring system for patients with chronic myelomonocytic leukemia. Blood. 2013;121(15):3005–15. This recent CMML-specific prognostic model was derived from a large and well-kept database. It includes factors readily available in most pathology labs and has been shown to have better prognostic discrimination over the MDAPS.
Calvo X, Nomdedeu M, Costa D, et al. Evaluation of two prognostic scoring systems for chronic myelomonocytic leukemia (CMML): CMML-Specific Prognostic Scoring System (CPSS) and MD Anderson Prognostic Score (MDAPS) in a series of 122 cases of de novo CMML. Blood. 2013;122(21):2810.
Patnaik MM, Padron E, LaBorde RR, et al. Mayo prognostic model for WHO-defined chronic myelomonocytic leukemia: ASXL1 and spliceosome component mutations and outcomes. Leukemia. 2013;27(7):1504–10.
Itzykson R, Kosmider O, Renneville A, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol. 2013;31(19):2428–36.
Patnaik MM, Itzykson R, Lasho TL, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014. Although not currently available in most pathology labs, testing for molecular markers will be more readily available in the near future. Not only will their prognostic information be useful in clinical decision making but may also predict response to particular treatments such as hypomethylating therapy
Eissa H, Gooley TA, Sorror ML, et al. Allogeneic hematopoietic cell transplantation for chronic myelomonocytic leukemia: relapse-free survival is determined by karyotype and comorbidities. Biol Blood Marrow Transplant. 2011;17(6):908–15.
Park S, Labopin M, Yakoub-Agha I, et al. Allogeneic stem cell transplantation for chronic myelomonocytic leukemia: a report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Eur J Haematol. 2013;90(5):355–64.
Cutler CS, Lee SJ, Greenberg P, et al. A decision analysis of allogeneic bone marrow transplantation for the myelodysplastic syndromes: delayed transplantation for low-risk myelodysplasia is associated with improved outcome. Blood. 2004;104(2):579–85.
Koreth J, Pidala J, Perez WS, et al. A decision analysis of reduced-intensity conditioning allogeneic hematopoietic stem cell transplantation for older patients with de-novo myelodysplastic syndrome (MDS): early transplantation offers survival benefit in higher-risk MDS. ASH Annu Meet Abstr. 2011;118(21):115.
Sorror ML. How I, assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121(15):2854–63.
Wardrop D, Steensma DP. Is refractory anaemia with ring sideroblasts and thrombocytosis (RARS-T) a necessary or useful diagnostic category? Br J Haematol. 2009;144(6):809–17.
Wattel E, Guerci A, Hecquet B, et al. A randomized trial of hydroxyurea versus VP16 in adult chronic myelomonocytic leukemia. Groupe Francais des Myelodysplasies and European CMML Group. Blood. 1996;88(7):2480–7.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32.
Ades L, Sekeres MA, Wolfromm A, et al. Predictive factors of response and survival among chronic myelomonocytic leukemia patients treated with azacitidine. Leuk Res. 2013;37(6):609–13.
Atypical. In: Dorland W, editor. The American pocket medical dictionary. Philadelphia: W. B. Saunders Company; 1943. p. 1037.
Hernandez JM, del Canizo MC, Cuneo A, et al. Clinical, hematological and cytogenetic characteristics of atypical chronic myeloid leukemia. Ann Oncol. 2000;11(4):441–4.
Kurzrock R, Bueso-Ramos CE, Kantarjian H, et al. BCR rearrangement-negative chronic myelogenous leukemia revisited. J Clin Oncol. 2001;19(11):2915–26.
Orazi A, Germing U. The myelodysplastic/myeloproliferative neoplasms: myeloproliferative diseases with dysplastic features. Leukemia. 2008;22(7):1308–19.
Koldehoff M, Beelen DW, Trenschel R, et al. Outcome of hematopoietic stem cell transplantation in patients with atypical chronic myeloid leukemia. Bone Marrow Transplant. 2004;34(12):1047–50.
Jabbour E, Kantarjian H, Cortes J, et al. PEG-IFN-alpha-2b therapy in BCR-ABL-negative myeloproliferative disorders: final result of a phase 2 study. Cancer. 2007;110(9):2012–8.
Mao L, You L, Yang M, Li Y, Ye X, Tong H-Y. The first case of decitabine successfully in treatment of atypical chronic myeloid leukemia with CEBPA double mutation. Chemotherapy. 2013;2(1):114.
Thepot S, Itzykson R, Seegers V, et al. Treatment of progression of Philadelphia-negative myeloproliferative neoplasms to myelodysplastic syndrome or acute myeloid leukemia by azacitidine: a report on 54 cases on the behalf of the Groupe Francophone des Myelodysplasies (GFM). Blood. 2010;116(19):3735–42.
Piazza R, Valletta S, Winkelmann N, et al. Recurrent SETBP1 mutations in atypical chronic myeloid leukemia. Nat Genet. 2013;45(1):18–24.
Maxson JE, Gotlib J, Pollyea DA, et al. Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N Engl J Med. 2013;368(19):1781–90. This paper describes a common mutation in atypical CML. This finding has the potential to improve diagnostic accuracy and provide a therapeutic target.
Schmitt-Graeff A, Thiele J, Zuk I, Kvasnicka HM. Essential thrombocythemia with ringed sideroblasts: a heterogeneous spectrum of diseases, but not a distinct entity. Haematologica. 2002;87(4):392–9.
Visconte V, Makishima H, Jankowska A, et al. SF3B1, a splicing factor is frequently mutated in refractory anemia with ring sideroblasts. Leukemia. 2012;26(3):542–5. This paper links the SF3B1 genotype with the ringed sideroblasts phenotype, eponymous to RARS and RARS-T.
Visconte V, Rogers HJ, Singh J, et al. SF3B1 haploinsufficiency leads to formation of ring sideroblasts in myelodysplastic syndromes. Blood. 2012;120(16):3173–86.
Liu Y, Tabarroki A, Visconte V, et al. A prognostic scoring system for unclassifiable MDS and MDS/MPN. ASH Annu Meet Abstr. 2012;120(21):1701.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Aaron T. Gerds received a grant from the American Society for Blood and Marrow Transplant.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gerds, A.T. I Walk the Other Line: Myelodysplastic/Myeloproliferative Neoplasm Overlap Syndromes. Curr Hematol Malig Rep 9, 400–406 (2014). https://doi.org/10.1007/s11899-014-0233-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-014-0233-2