Abstract
Decades of prostatocentric research and publications have hampered care for men with genital or pelvic pain syndromes who are often misdiagnosed with prostatitis. The prostatitis classification system as well as other misuse of terminology may have direct and indirect influence on physicians and lay persons alike. Taxonomy, medical culture, and gender issues perpetuate the substandard evaluation of men with this condition as well as the continued overuse of antibiotics. Because the vast majority of men with this condition have neither an infection nor a disease of the prostate gland, physicians must alter their approach to these patients. Thankfully, there is growing interest and evidence to show that male pelvic pain can and should be approached more broadly, even as a nonurological condition.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Krieger JN, Nyberg Jr L, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999;282(3):236–7.
Proceedings of the Giessen Consensus Panel Meeting, Giessen, Germany, September, 2002. This author was honored to be part of the consensus panel, however, very frustrated about the subsequent lack of interest or attention to the recommendations. The compilation of the entire meeting is published in European Urology supplement, 2003.
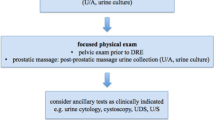
Nickel JC. The pre and post massage test (PPMT): a simple screen for prostatitis. Tech Urol. 1997;3(1):38–43.
McNaughton Collins M, Fowler Jr FJ, Elliott DB, Albertsen PC, Barry MJ. Diagnosing and treating chronic prostatitis: do urologists use the four-glass test? Urology. 2000;55:403–7.
Gerald GH, McCammon KA. Surgery for the penis and urethra in Campbell-Walsh Urology, vol. 1. 10th ed. Philadelphia: Elsevier Saunders; 2012. p. 968.
Gonder MJ. Prostatitis. Lancet. 1963;83:305–6.
Schaeffer AJ, Knauss JS, Landis JR, et al. Leukocyte and bacterial counts do not correlate with severity of symptoms in men with chronic prostatitis: the national institutes of health chronic prostatitis cohort study. J Urol. 2002;168:1048–53.
Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968;5:492–518.
Nickel JC, Downey J, Clark J, et al. Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial. Urology. 2003;62:614–7.
Alexander RB, Propert KJ, Schaeffer AJ, et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004;141:581–9.
Nickel JC, Alexander RB, Schaeffer AJ, et al. Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol. 2003;170:818–22.
Nickel JC, Downey J, Ardern D, Clark J, Nickel K. Failure of a monotherapy strategy for difficult chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004;172:551–4. As mentioned in the text, this is one of my favorite citations as it was conducted thoughtfully and methodically, and empowers us even more to abandon one dimensional thinking when it comes to CPPS in men.
Nickel JC, Stephens A, Chen J, et al. Application of state-of-the-art methods to search for microbial contributions to the etiology of urological chronic pelvic pain syndrome (UCPPS) Abstract 1147, presented at American Urologic Association Annual Meeting, 2013. This is a large, very well done study. I can’t wait for it to be published.
Strebel RT, Schmidt C, Beatrice J, Sulser T. Chronic scrotal pain syndrome (CSPS): the widespread use of antibiotics is not justified. Andrology. 2013;1(1):155–9.
Pontari MA, Krieger JN, Litwin MS, et al. Pregabalin for the treatment of men with chronic prostatitis/chronic pelvic pain syndrome: a randomized controlled trial. Arch Intern Med. 2010;170(17):1586–93.
Nickel JC, Krieger JN, McNaughton-Collins M, et al. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. NEJM. 2008;359:2663–73.
Fitzgerald M, Anderson R, Potts J, et al. UPPCRN: randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urologic chronic pelvic pain syndromes. J Urol. 2009;182:570–80. Even though this was designed and powered only as a feasibility trial, this study went on to demonstrate statistically significant improvement in CPPS when men received manual Myofascial Trigger Point Release.
Krieger JN, Ross SO, Riley DE. Chronic prostatitis: epidemiology and role of infection. Urology. 2002;60(6 Suppl):8–12. discussion 13.
Nickel JC, Alexander R, Anderson R, et al. Prostatitis unplugged? Prostatic massage revisited. Tech Urol. 1999;5:1–7.
Potts JM. Prospective identification of national institutes of health category IV prostatitis in men with elevated prostate specific antigen. J Urol. 2000;164:1550–3.
True LD, Berger RE, Rothman I, Ross SO, Krieger JN. Prostate histopathology and the chronic prostatitis/chronic pelvic pain syndrome: a prospective biopsy study. J Urol. 1999;162:2014–8.
Segura JW. Prostatosis, prostatitis or pelvic floor tension myalgia? J Urol. 1979;122:122–68.
Miller HC. Stress prostatitis. Urology. 1988;32:507–10.
Kaplan SA, Te AE, Jacobs BZ. Urodynamic evidence of vesical neck obstruction in men with misdiagnosed chronic nonbacterial prostatitis and the therapeutic role of endoscopic incision of the bladder neck. J Urol. 1994;152:2063–5.
Kaplan SA, Santarosa RP, D’Alisera PM, et al. Pseudodyssynergia (contraction of the external sphincter during voiding) misdiagnosed as chronic non-bacterial prostatitis and the role of biofeedback as a therapeutic option. J Urol. 1997;157:2234–7.
Jamzadeh AE, Xie D, Laudano M, et al. Urodynamic characterization of lower urinary tract symptoms in men less than 40 years of age. World J Urol. 2014;32(2):469–73.
Kaplan SA, Ikeguchi EF, Santarose RP, et al. Etiology of voiding dysfunction in men less than 50 years of age. Urology. 1996;47:836–9.
Anderson RU, Wise D, Sawyer T, Chan C. Integration of myofascial trigger point release and paradoxical relation training treatment of chronic pelvic pain in men. J Urol. 2005;174:155–60. Although there are some publications which precede this observational cohort study, it is among the largest series and introduces an integrative approach, using both physical therapy and psychological modalities, i.e. a unique form of relaxation techniques.
Clemens JQ, Nadler RB, Schaeffer AJ, et al. Biofeedback, pelvic floor re-education, and bladder training for male chronic pelvic pain syndrome. Urology. 2000;56(6):951–5.
Cornel EB, van Haarst EP, Browning-Groote Schaarsberg RWM, Geels J. The effect of biofeedback physical therapy in men with chronic pelvic pain syndrome type III. Eur Urol. 2005;47:607–11.
Anderson RU, Wise D, Sawyer T, et al. 6-day intensive treatment protocol for refractory chronic prostatitis/chronic pelvic pain syndrome using myofascial release and paradoxical relaxation training. J Urol. 2011;185(4):1294–9.
Khorasani B, Arab AM, Sedighi Gilani MA, et al. Transabdominal ultrasound measurement of pelvic floor muscle mobility in men with and without chronic prostatitis/chronic pelvic pain syndrome. Urology. 2012;80(3):673–7.
Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009;12(2):177–83.
Potts JM. Prostatitis—alternative approaches: biofeedback, progressive relaxation and the concept of functional somatic syndromes. Eur Urol Suppl. 2003.
Tripp DA, Nickel JC, Wang Y, et al. Catastrophizing and pain-contingent rest predict patient adjustment in men with chronic prostatitis/chronic pelvic pain syndrome. J Pain. 2006;7(10):697–708.
Anderson RU, Orenberg EK, Morey A, Chavez N, Chan CA. Stress induced hypothalamus-pituitary-adrenal axis responses and disturbances in psychological profiles in men with chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2009;182(5):2319–24.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Jeannette Potts declares that she is a paid consultant of New Pelvic Pain Technologies and her spouse is a paid board member of Allergan and Astellas.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pelvic Pain
Rights and permissions
About this article
Cite this article
Potts, J.M. Male Pelvic Pain Syndrome: Escaping the Snare of Prostatocentric Thinking. Curr Bladder Dysfunct Rep 10, 75–80 (2015). https://doi.org/10.1007/s11884-014-0286-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-014-0286-z