Abstract
Purpose
Data have demonstrated an association between regret and lack of fertility counseling among patients undergoing treatment for non-gynecologic cancers. We sought to determine if fertility-related regret is reduced with pre-treatment counseling or fertility-sparing surgery (FSS) in patients with gynecologic cancers.
Methods
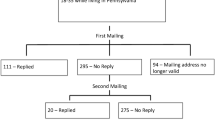
A cross-sectional survey was administered to 593 reproductive-age survivors (18–40 years old at diagnosis) of localized cervix, ovarian, or endometrial cancers that were eligible for FSS. A validated decision regret score was used to evaluate regret in patients.
Results
Four hundred seventy women completed the survey. Forty-six percent received pre-treatment counseling about treatment’s effects on fertility. Having received counseling (adjusted ß-coefficient of −1.24, 95 % CI = −2.29 to −0.18, p = 0.02), satisfactory counseling (adjusted ß-coefficient of −2.71, 95 % CI = −3.86 to −1.57, p < 0.001), and FSS (adjusted ß-coefficient of −1.26, 95 % CI = −2.39 to −0.14, p = 0.03) were associated with lower regret post-treatment, after adjusting for age. Time since diagnosis, prior parity, socioeconomic status and cancer type were not associated with regret (p > 0.05). While 50 % of women reported desiring more children after diagnosis, desire for children after treatment was associated with increased regret (adjusted ß-coefficient of 3.97, 95 % CI = 2.92–5.02, p < 0.001).
Conclusions
Though less than half of study participants received counseling about the effect of cancer treatment on future fertility, both fertility counseling and FSS were associated with decreased regret in reproductive-aged women with gynecologic cancers. The desire for more children after treatment was associated with increased regret.
Implications for cancer survivors
Inquiring about fertility desires and providing counseling regarding reproductive outcomes following cancer treatment should be implemented as part of the treatment process.
Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29. doi:10.3322/caac.21254.
Eskander RN, Randall LM, Berman ML, Tewari KS, Disaia PJ, Bristow RE. Fertility preserving options in patients with gynecologic malignancies. Am J Obstet Gynecol. 2011;205(2):103–10. doi:10.1016/j.ajog.2011.01.025.
Maltaris T, Boehm D, Dittrich R, Seufert R, Koelbl H. Reproduction beyond cancer: a message of hope for young women. Gynecol Oncol. 2006;103(3):1109–21. doi:10.1016/j.ygyno.2006.08.003.
Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009;15(5):587–97. doi:10.1093/humupd/dmp015.
Armuand GM, Wettergren L, Rodriguez-Wallberg KA, Lampic C. Women more vulnerable than men when facing risk for treatment-induced infertility: a qualitative study of young adults newly diagnosed with cancer. Acta Oncol. 2014;54(2):243–52. doi:10.3109/0284186X.2014.948573.
Noyes N, Knopman JM, Long K, Coletta JM, Abu-Rustum NR. Fertility considerations in the management of gynecologic malignancies. Gynecol Oncol. 2011;120(3):326–33. doi:10.1016/j.ygyno.2010.09.012.
Letourneau J, Chan J, Salem W, Chan SW, Shah M, Ebbel E, et al. Fertility sparing surgery for localized ovarian cancers maintains an ability to conceive, but is associated with diminished reproductive potential. J Surg Oncol. 2015;112(1):26–30. doi:10.1002/jso.23942.
Deshpande NA, Braun IM, Meyer FL. Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: a systematic review. Cancer. 2015. doi:10.1002/cncr.29637.
Wenzel L, Dogan-Ates A, Habbal R, Berkowitz R, Goldstein DP, Bernstein M, et al. Defining and measuring reproductive concerns of female cancer survivors. J Natl Cancer Inst Monogr. 2005;34:94–8. doi:10.1093/jncimonographs/lgi017.
Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281–92.
Clark JA, Inui TS, Silliman RA, Bokhour BG, Krasnow SH, Robinson RA, et al. Patients’ perceptions of quality of life after treatment for early prostate cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 2003;21(20):3777–84. doi:10.1200/JCO.2003.02.115.
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118(6):1710–7. doi:10.1002/cncr.26459.
Collingwood SA, McBride RB, Leapman M, Hobbs AR, Kwon YS, Stensland KD, et al. Decisional regret after robotic-assisted laparoscopic prostatectomy is higher in African American men. Urol Oncol. 2014;32(4):419–25. doi:10.1016/j.urolonc.2013.10.011.
Bastings L, Baysal O, Beerendonk CC, IntHout J, Traas MA, Verhaak CM, et al. Deciding about fertility preservation after specialist counselling. Hum Reprod (Oxford, Engl). 2014;29(8):1721–9. doi:10.1093/humrep/deu136.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol: Off J Am Soc Clin Oncol. 2013;31(19):2500–10. doi:10.1200/JCO.2013.49.2678.
Peate M, Meiser B, Cheah BC, Saunders C, Butow P, Thewes B, et al. Making hard choices easier: a prospective, multicentre study to assess the efficacy of a fertility-related decision aid in young women with early-stage breast cancer. Br J Cancer. 2012;106(6):1053–61. doi:10.1038/bjc.2012.61.
Gardino SL, Jeruss JS, Woodruff TK. Using decision trees to enhance interdisciplinary team work: the case of oncofertility. J Assist Reprod Genet. 2010;27(5):227–31. doi:10.1007/s10815-010-9413-8.
Huyghe E, Sui D, Odensky E, Schover LR. Needs assessment survey to justify establishing a reproductive health clinic at a comprehensive cancer center. J Sex Med. 2009;6(1):149–63. doi:10.1111/j.1743-6109.2008.01005.x.
Nakayama K, Liu P, Detry M, Schover LR, Milbourne A, Neumann J, et al. Receiving information on fertility- and menopause-related treatment effects among women who undergo hematopoietic stem cell transplantation: changes in perceived importance over time. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2009;15(11):1465–74. doi:10.1016/j.bbmt.2009.07.019.
Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol: Off J Am Soc Clin Oncol. 2002;20(7):1880–9.
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol: Off J Am Soc Clin Oncol. 2004;22(20):4174–83. doi:10.1200/JCO.2004.01.159.
Arora NK, Hamilton AS, Potosky AL, Rowland JH, Aziz NM, Bellizzi KM, et al. Population-based survivorship research using cancer registries: a study of non-Hodgkin’s lymphoma survivors. J Cancer Survivorship: Res Pract. 2007;1(1):49–63. doi:10.1007/s11764-007-0004-3.
Acknowledgments
This research was supported by the National Institutes of Health (Grant Number T32 HD007440—Dr. Chan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chan, J.L., Letourneau, J., Salem, W. et al. Regret around fertility choices is decreased with pre-treatment counseling in gynecologic cancer patients. J Cancer Surviv 11, 58–63 (2017). https://doi.org/10.1007/s11764-016-0563-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0563-2