Abstract
Purpose
We investigated how treatment-induced neuropathic symptoms are associated with patients’ quality of life (QOL) and clinician-reported difficulty in caring for patients.
Methods
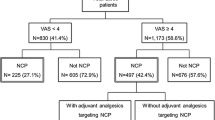
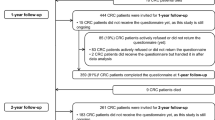
Data were obtained from 3,106 outpatients with colorectal, breast, lung, or prostate cancer on numbness/tingling (N/T), neuropathic pain, and QOL. Clinicians reported the degree of difficulty in caring for patients’ physical and psychological symptoms.
Results
For all patients, moderate to severe N/T was associated with poor QOL (OR = 1.82, 95 % CI = 1.47–2.26, P < 0.001) but neuropathic pain was not (OR = 1.31, 95 % CI = 0.94–1.83, P = 0.114). Moderate to severe N/T and neuropathic pain were associated with increased care difficulty (OR = 1.49, 95 % CI = 1.27–1.74, P < 0.001 for N/T, and OR = 1.46, 95 % CI = 1.15–1.84, P = 0.002 for neuropathic pain). The association of neuropathic pain with care difficulty was most significant in patients with colorectal cancer (CRC) (OR = 2.32, 95 % CI = 1.41–3.83, P = 0.001). Baseline neuropathic pain was associated with declining QOL in CRC patients (OR = 2.08, 95 % CI = 1.21–3.58, P = 0.008).
Conclusions
Clinicians may experience increased care difficulty for patients of all cancer types with moderate to severe N/T or neuropathic pain; care difficulty due to neuropathic pain may be higher for CRC patients. Nearly half the patients of all cancer types with moderate to severe N/T may expect poor short-term QOL; CRC—but not other—patients with baseline neuropathic pain are likely to experience declining QOL.
Implications for Cancer Survivors
About half of patients with moderate to severe N/T (any cancer type) may expect poor QOL in the short term; CRC patients with baseline neuropathic pain in particular may experience declining QOL.


Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA: Cancer J Clin. 2013;63(1):11–30. doi:10.3322/caac.21166.
André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004;350(23):2343–51. doi:10.1056/NEJMoa032709.
André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol: Off J Am Soc Clin Oncol. 2009;27(19):3109–16. doi:10.1200/jco.2008.20.6771.
Krishnan AV, Goldstein D, Friedlander M, Kiernan MC. Oxaliplatin-induced neurotoxicity and the development of neuropathy. Muscle Nerve. 2005;32(1):51–60. doi:10.1002/mus.20340.
Tofthagen C. Surviving chemotherapy for colon cancer and living with the consequences. J Palliat Med. 2010;13(11):1389–91. doi:10.1089/jpm.2010.0124.
Weickhardt A, Wells K, Messersmith W. Oxaliplatin-induced neuropathy in colorectal cancer. J Oncol. 2011;2011:201593. doi:10.1155/2011/201593.
Argyriou AA, Cavaletti G, Briani C, Velasco R, Bruna J, Campagnolo M, et al. Clinical pattern and associations of oxaliplatin acute neurotoxicity: a prospective study in 170 patients with colorectal cancer. Cancer. 2013;119(2):438–44. doi:10.1002/cncr.27732.
Bennett BK, Park SB, Lin CS, Friedlander ML, Kiernan MC, Goldstein D. Impact of oxaliplatin-induced neuropathy: a patient perspective. Support Care Cancer: Off J Multinational Assoc Support Care Cancer. 2012;20(11):2959–67. doi:10.1007/s00520-012-1428-5.
Tofthagen C, Donovan KA, Morgan MA, Shibata D, Yeh Y. Oxaliplatin-induced peripheral neuropathy’s effects on health-related quality of life of colorectal cancer survivors. Support Care Cancer: Off J Multinational Assoc Support Care Cancer. 2013;21(12):3307–13. doi:10.1007/s00520-013-1905-5.
Mols F, Beijers T, Lemmens V, van den Hurk CJ, Vreugdenhil G, van de Poll-Franse LV. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol: Off J Am Soc Clin Oncol. 2013;31(21):2699–707. doi:10.1200/jco.2013.49.1514.
Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, Kamal A, et al. Further data supporting that paclitaxel-associated acute pain syndrome is associated with development of peripheral neuropathy: North Central Cancer Treatment Group trial N08C1. Cancer. 2012;118(20):5171–8. doi:10.1002/cncr.27489.
Loprinzi CL, Reeves BN, Dakhil SR, Sloan JA, Wolf SL, Burger KN, et al. Natural history of paclitaxel-associated acute pain syndrome: prospective cohort study NCCTG N08C1. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(11):1472–8. doi:10.1200/jco.2010.33.0308.
Speck RM, Sammel MD, Farrar JT, Hennessy S, Mao JJ, Stineman MG, et al. Impact of chemotherapy-induced peripheral neuropathy on treatment delivery in nonmetastatic breast cancer. J Oncol Pract. 2013. doi:10.1200/jop.2012.000863.
Lewis MA, Zhao F, Jones D, Loprinzi C, Brell JM, Weiss M, Fisch MJ (2014) Neuropathic symptoms and their risk factors in medical oncology outpatients with colorectal versus breast, lung or prostate cancer—results from a prospective mulitcenter study. Support Care Cancer, Under review
Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer. 2000;89(7):1634–46.
Fainsinger RL, Nekolaichuk CL, Lawlor PG, Neumann CM, Hanson J, Vigano A. A multicenter study of the revised Edmonton Staging System for classifying cancer pain in advanced cancer patients. J Pain Symptom Manag. 2005;29(3):224–37. doi:10.1016/j.jpainsymman.2004.05.008.
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61(2):277–84.
StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. 2009.
Loprinzi CL, Maddocks-Christianson K, Wolf SL, Rao RD, Dyck PJ, Mantyh P, et al. The Paclitaxel acute pain syndrome: sensitization of nociceptors as the putative mechanism. Cancer J (Sudbury, Mass). 2007;13(6):399–403. doi:10.1097/PPO.0b013e31815a999b.
Lesser H, Sharma U, LaMoreaux L, Poole RM. Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trial. Neurology. 2004;63(11):2104–10.
Smith EM, Pang H, Cirrincione C, Fleishman S, Paskett ED, Ahles T, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA: J Am Med Assoc. 2013;309(13):1359–67. doi:10.1001/jama.2013.2813.
Schloss JM, Colosimo M, Airey C, Masci PP, Linnane AW, Vitetta L. Nutraceuticals and chemotherapy induced peripheral neuropathy (CIPN): a systematic review. Clin Nutrition (Edinburgh, Scotland). 2013;32(6):888–93. doi:10.1016/j.clnu.2013.04.007.
Loprinzi CL, Qin R, Dakhil SR, Fehrenbacher L, Flynn KA, Atherton P, et al. Phase III randomized, placebo-controlled, double-blind study of intravenous calcium and magnesium to prevent oxaliplatin-induced sensory neurotoxicity (N08CB/alliance). J Clin Oncol: Off J Am Soc Clin Oncol. 2013. doi:10.1200/jco.2013.52.0536.
Beijers AJ, Jongen JL, Vreugdenhil G. Chemotherapy-induced neurotoxicity: the value of neuroprotective strategies. Netherlands J Med. 2012;70(1):18–25.
Schroder S, Beckmann K, Franconi G, Meyer-Hamme G, Friedemann T, Greten HJ, et al. Can medical herbs stimulate regeneration or neuroprotection and treat neuropathic pain in chemotherapy-induced peripheral neuropathy? Evidence-based Complement Alternat Med: eCAM. 2013;2013:423713. doi:10.1155/2013/423713.
Seretny M, Colvin L, Fallon M. Therapy for chemotherapy-induced peripheral neuropathy. JAMA: J Am Med Assoc. 2013;310(5):537–8. doi:10.1001/jama.2013.7902.
Smith EM, Pang H. Therapy for chemotherapy-induced peripheral neuropathy—in reply. JAMA: J Am Med Assoc. 2013;310(5):538. doi:10.1001/jama.2013.7905.
Postma TJ, Reijneveld JC, Heimans JJ. Prevention of chemotherapy-induced peripheral neuropathy: a matter of personalized treatment? Ann Oncol: Off J Eur Soc Med Oncol/ESMO. 2013;24(6):1424–6. doi:10.1093/annonc/mdt173.
Schroeder S, Meyer-Hamme G, Epplée S. Acupuncture for chemotherapy-induced peripheral neuropathy (CIPN): a pilot study using neurography. Acupunct Med. 2012;30(1):4–7. doi:10.1136/acupmed-2011-010034.
Guo Y, Jones D, Palmer JL, Forman A, Dakhil SR, Velasco MR, et al. Oral alpha-lipoic acid to prevent chemotherapy-induced peripheral neuropathy: a randomized, double-blind, placebo-controlled trial. Support Care Cancer: Off J Multinational Assoc Support Care Cancer. 2013. doi:10.1007/s00520-013-2075-1.
Acknowledgments
This study was supported in part by Public Health Service Grants CA37604, CA17145, and grants from the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Drs. Fisch and Zhao had full access to the data.
Conflict of interest
The authors reported no disclosures or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, D., Zhao, F., Brell, J. et al. Neuropathic symptoms, quality of life, and clinician perception of patient care in medical oncology outpatients with colorectal, breast, lung, and prostate cancer. J Cancer Surviv 9, 1–10 (2015). https://doi.org/10.1007/s11764-014-0379-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0379-x