Abstract
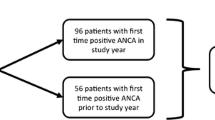
A prompt immunosuppressive treatment initiation is crucial in ANCA-associated vasculitis (AAV) to minimize organ injury. The aim of the present work was to analyze the accuracy of emergency ANCA screening to identify rapidly patients with AAV. In our Institution, emergency ANCA screening is based on a telephone call between a Clinician and a Biologist. Indirect immunofluorescence (IIF) for ANCA detection was performed using a commercial kit (Euroimmun® Granulocyte Mosaic 12). Positive serums for c- or p-ANCA at IIF are subsequently screened for antigenic specificity (MPO or PR3) by an immunodot technique (immunodot, D-Tek®.) Positive samples with atypical c- or p-ANCA pattern at IIF are subsequently screened for antigenic specificity by ELISA. Data were retrieved from patients’ medical records and confronted to emergency ANCA screening results. Between 2005 and 2012, 114 patients were screened. IIF was positive in 27.2 % of patients, but c-/p-ANCA anti-MPO/-PR3 was detected in 13.2 % of patients. The sensibility and specificity of IIF combined with immunodot for newly diagnosed AAV were 83.3 and 100 %, respectively. Ten patients were newly diagnosed with AAV. In these patients, a specific AAV treatment was initiated less than 24 h following ANCA screening. Emergency ANCA screening based on a clinical gating policy was relevant to identify patients with AAV diagnosis, and was associated with a rapid treatment initiation.

Similar content being viewed by others
References
Beauvillain C, Delneste Y, Renier G, Jeannin P, Subra JF, Chevailler A (2008) Antineutrophil cytoplasmic autoantibodies: how should the biologist manage them? Clin Rev Allergy Immunol 35(1–2):47–58. doi:10.1007/s12016-007-8071-9
Jennette JC, Falk RJ, Hu P, Xiao H (2013) Pathogenesis of antineutrophil cytoplasmic autoantibody-associated small-vessel vasculitis. Annu Rev Pathol 8:139–160. doi:10.1146/annurev-pathol-011811-132453
Tervaert JW, van der Woude FJ, Fauci AS, Ambrus JL, Velosa J, Keane WF, Meijer S, van der Giessen M, van der Hem GK, The TH et al (1989) Association between active Wegener’s granulomatosis and anticytoplasmic antibodies. Arch Intern Med 149(11):2461–2465
Subra JF, Michelet C, Laporte J, Carrere F, Reboul P, Cartier F, Saint-Andre JP, Chevailler A (1998) The presence of cytoplasmic antineutrophil cytoplasmic antibodies (C-ANCA) in the course of subacute bacterial endocarditis with glomerular involvement, coincidence or association? Clin Nephrol 49(1):15–18
Tur BS, Suldur N, Ataman S, Tutkak H, Atay MB, Duzgun N (2004) Anti-neutrophil cytoplasmic antibodies in patients with rheumatoid arthritis: clinical, biological, and radiological correlations. Jt Bone Spine : revue du rhumatisme 71(3):198–202. doi:10.1016/j.jbspin.2003.04.002
Aslam A, Newman TL, Misbah SA (2003) Audit of the clinical usefulness of a rapid qualitative ELISA screen for antimyeloperoxidase and antiproteinase 3 antibodies in the assessment of patients with suspected vasculitis. J Clin Pathol 56(10):775–777
Savige J, Gillis D, Benson E, Davies D, Esnault V, Falk RJ, Hagen EC, Jayne D, Jennette JC, Paspaliaris B, Pollock W, Pusey C, Savage CO, Silvestrini R, van der Woude F, Wieslander J, Wiik A (1999) International consensus statement on testing and reporting of antineutrophil cytoplasmic antibodies (ANCA). Am J Clin Pathol 111(4):507–513
Savige J, Dimech W, Fritzler M, Goeken J, Hagen EC, Jennette JC, McEvoy R, Pusey C, Pollock W, Trevisin M, Wiik A, Wong R, International Group for Consensus Statement on T, Reporting of Antineutrophil Cytoplasmic A (2003) Addendum to the international consensus statement on testing and reporting of antineutrophil cytoplasmic antibodies. Quality control guidelines, comments, and recommendations for testing in other autoimmune diseases. Am J Clin Pathol 120(3):312–318. doi:10.1309/WAEP-ADW0-K4LP-UHFN
Arnold DF, Timms A, Luqmani R, Misbah SA (2010) Does a gating policy for ANCA overlook patients with ANCA associated vasculitis? An audit of 263 patients. J Clin Pathol 63(8):678–680. doi:10.1136/jcp.2009.072504
Mandl LA, Solomon DH, Smith EL, Lew RA, Katz JN, Shmerling RH (2002) Using antineutrophil cytoplasmic antibody testing to diagnose vasculitis: can test-ordering guidelines improve diagnostic accuracy? Arch Intern Med 162(13):1509–1514
Sinclair D, Saas M, Stevens JM (2004) The effect of a symptom related “gating policy” on ANCA requests in routine clinical practice. J Clin Pathol 57(2):131–134
Robinson PC, Steele RH (2009) Appropriateness of antineutrophil cytoplasmic antibody testing in a tertiary hospital. J Clin Pathol 62(8):743–745. doi:10.1136/jcp.2009.064485
Russell KA, Wiegert E, Schroeder DR, Homburger HA, Specks U (2002) Detection of anti-neutrophil cytoplasmic antibodies under actual clinical testing conditions. Clin Immunol 103(2):196–203. doi:10.1006/clim.2001.5200
Tsiveriotis K, Tsirogianni A, Pipi E, Soufleros K, Papasteriades C (2011) Antineutrophil cytoplasmic antibodies testing in a large cohort of unselected greek patients. Autoimmun Dis 2011:626495. doi:10.4061/2011/626495
Moroni G, Ponticelli C (2014) Rapidly progressive crescentic glomerulonephritis: early treatment is a must. Autoimmun Rev 13(7):723–729. doi:10.1016/j.autrev.2014.02.007
Catanoso M, Pipitone N, Magnani L, Boiardi L, Salvarani C (2011) New indications for biological therapies. Intern Emerg Med 6(Suppl 1):1–9. doi:10.1007/s11739-011-0667-7
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sayegh, J., Poli, C., Chevailler, A. et al. Emergency testing for antineutrophil cytoplasmic antibodies combined with a dialog-based policy between clinician and biologist: effectiveness for the diagnosis of ANCA-associated vasculitis. Intern Emerg Med 10, 315–319 (2015). https://doi.org/10.1007/s11739-014-1141-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-014-1141-0