Abstract
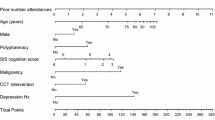
Estimation of the risk of revisit to the emergency department (ED) soon after discharge in the older population may assist discharge planning and targeting of post discharge intervention in high risk patients. In this study we sought to derive a risk prediction calculator for this purpose. In a prospective observational study in two tertiary ED, we conducted a comprehensive assessment of people aged 65 and over, and followed them for a minimum of 28 days post discharge. Cox proportional hazard models relating any unplanned ED revisit in the follow up period to observed risk factors were used to compute a probability nomogram. From 1,439 patients, 189 (13.1 %) had at least one unplanned revisit within 28 days. Revisit probability was weighted towards chronic and difficult to modify risk factors such as depression, malignancy and cognitive impairment. We conclude that the risk of revisit post discharge is calculable using a probability nomogram. However, revisit is largely related to immutable factors reflecting chronic illness burden, and does not necessarily reflect poor ED care during the initial index presentation.


Similar content being viewed by others
References
McCusker J, Roberge D, Vadeboncoeur A, Verdon J (2009) Safety of discharge of seniors from the emergency department to the community. Healthc Q, 12 Spec No Patient: 24–32
Hughes G (2012) A&E quality indicators. Emerg Med J 29(2):90
McCusker J, Cardin S, Bellavance F, Belzile E (2000) Return to the emergency department among elders: patterns and predictors. Acad Emerg Med 7(3):249–259
Hastings SN, Heflin MT (2005) A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med 12(10):978–986
Xu KT, Nelson BK, Berk S (2009) The changing profile of patients who used emergency department services in the United States: 1996 to 2005. Ann Emerg Med 54(6):805–810.e801-807
McCusker J, Verdon J (2006) Do geriatric interventions reduce emergency department visits? A systematic review. J Gerontol A Biol Sci Med Sci 61(1):53–62
Schumacher JG (2005) Emergency medicine and older adults: continuing challenges and opportunities. Am J Emerg Med 23(4):556–560
Wilber ST, Gerson LW, Terrell KM, Carpenter CR, Shah MN, Heard K, Hwang U (2006) Geriatric emergency medicine and the 2006 Institute of Medicine reports from the Committee on the Future of Emergency Care in the U.S. Health System. Acad Emerg Med 13(12):1345–1351
Hwang U, Morrison RS (2007) The geriatric emergency department. J Am Geriatr Soc 55(11):1873–1876
Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, Burant CJ, Landefeld CS (2003) Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 51(4):451–458
Wu AW, Yasui Y, Alzola C, Galanos AN, Tsevat J, Phillips RS, Connors AF Jr, Teno JM, Wenger NS, Lynn J et al (2000) Predicting functional status outcomes in hospitalized patients aged 80 years and older. J Am Geriatr Soc 48(5 Suppl):S6–S15
Hastings SN, Oddone EZ, Fillenbaum G, Sloane RJ, Schmader KE (2008) Frequency and predictors of adverse health outcomes in older medicare beneficiaries discharged from the emergency department. Med Care 46(8):771–777
Caplan GA, Brown A, Croker WD, Doolan J (1998) Risk of admission within 4 weeks of discharge of elderly patients from the emergency department–the DEED study. Discharge of elderly from emergency department. Age Ageing 27(6):697–702
Moons P, De Ridder K, Geyskens K, Sabbe M, Braes T, Flamaing J, Milisen K (2007) Screening for risk of readmission of patients aged 65 years and above after discharge from the emergency department: predictive value of four instruments. Eur J Emerg Med 14(6):315–323
Arendts G, Fitzhardinghe S, Pronk K, Donaldson M, Hutton M, Nagree Y (2012) The impact of early emergency department allied health intervention on admission rates in older people: a non-randomized clinical study. BMC Geriatrics 12:8
Moss JE, Flower CL, Houghton LM, Moss DL, Nielsen DA, Taylor DM (2002) A multidisciplinary care coordination team improves emergency department discharge planning practice. Med J Aust 177(8):435–439
Holman CDAJ, Bass AJ, Rosman DL, Smith MB, Semmens JB, Glasson EJ, Brook EL, Trutwein B, Rouse IL, Watson CR et al (2008) A decade of data linkage in western Australia: strategic design, applications and benefits of the WA data linkage system. Aust Health Rev 32(4):766–777
Harrell FE Jr, Lee KL, Mark DB et al (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387
Beland F, Bergman H, Lebel P, Clarfield AM, Tousignant P, Contandriopoulos A-P, Dallaire L (2006) A system of integrated care for older persons with disabilities in Canada: results from a randomized controlled trial. J Gerontol A Biol Sci Med Sci 61(4):367–373
Ballabio C, Bergamaschini L, Mauri S, Baroni E, Ferretti M, Bilotta C, Vergani C (2008) A comprehensive evaluation of elderly people discharged from an Emergency Department. Intern Emerg Med 3(3):245–249
Mion LC, Palmer RM, Meldon SW, Bass DM, Singer ME, Payne SMC, Lewicki LJ, Drew BL, Connor JT, Campbell JW et al (2003) Case finding and referral model for emergency department elders: a randomized clinical trial. Ann Emerg Med 41(1):57–68
Meldon SW, Mion LC, Palmer RM, Drew BL, Connor JT, Lewicki LJ, Bass DM, Emerman CL (2003) A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department. Acad Emerg Med 10(3):224–232
McCusker J, Bellavance F, Cardin S, Trepanier S, Verdon J, Ardman O (1999) Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc 47(10):1229–1237
Meldon SW, Emerman CL, Schubert DS, Moffa DA, Etheart RG (1997) Depression in geriatric ED patients: prevalence and recognition. Ann Emerg Med 30(2):141–145
Bula CJ, Wietlisbach V, Burnand B, Yersin B (2001) Depressive symptoms as a predictor of 6-month outcomes and services utilization in elderly medical inpatients. Arch Intern Med 161(21):2609–2615
Acknowledgments
CCT members at each site provided invaluable assistance with the study. Mr Michael Phillips and Ms Sally Burrows assisted with statistical analysis. The research was funded by a grant from the State Health Research Advisory Council of Western Australia.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arendts, G., Fitzhardinge, S., Pronk, K. et al. Derivation of a nomogram to estimate probability of revisit in at-risk older adults discharged from the emergency department. Intern Emerg Med 8, 249–254 (2013). https://doi.org/10.1007/s11739-012-0895-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-012-0895-5