Abstract
Background
Bariatric surgery orientation sessions are often the first point of contact and a recommended component of pre-bariatric surgery assessment. Self-removal rates after bariatric program orientation are as high as 25 % despite the proven efficacy of this procedure. The objective of this study was to identify factors contributing to patient self-removal after orientation using a mixed method approach.
Methods
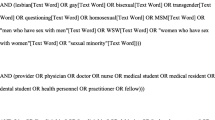
Patients who attended the Toronto Western Hospital Bariatric Surgery Program orientation between 2012 and 2013 and then self-removed from the program (N = 216) were included in the study. Subjects were interviewed via telephone using a semi-structured interview guide, generating both quantitative and qualitative data. Factors leading to discontinuation were rated on a five-point Likert scale. Qualitative data was analyzed using constant comparative methodology.
Results
The response rate was 59 % with a 40.7 % completion rate (N = 88). Concerns about potential surgical risks and complications and the ability to adapt to changes in eating and drinking post-operatively were identified as the top two factors for patients’ self-removal from the program. Thematic analysis uncovered 11 major themes related to patient self-removal. Unexpected themes include perceived personal suitability for the surgery, family impact of surgery, miscommunication with the family physician, and fears related to the orientation information.
Conclusions
This is one of the first studies examining barriers to bariatric surgery in the pre-operative setting and offers new insights into the reasons patients self-remove from bariatric surgery programs. This study may inform bariatric orientation program changes resulting in improved access to this effective surgical intervention.

Similar content being viewed by others
References
World Health Organization. Obesity and overweight fact sheet N8311. 2006. Available from: http://www.who.int/mediacentre/factsheets/fs311/en
Statistics Canada. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. 2012. Available from: http://www.statcan.gc.ca/pub/82-003-x/2012003/article/11706-eng.htm
Ludwig D, Pollack H. Obesity and the economy: from crisis to opportunity. JAMA. 2002;301(5):533–5.
Pitzul KB, Jackson T, Crawford S, et al. Understanding disposition after referral for bariatric surgery: when and why patients referred do not undergo surgery. Obes Surg. 2014;24(1):134–40.
Buchwald H, Oien D. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Canadian Institute for Health Information. Bariatric surgery in Canada. 2014. Available from: https://secure.cihi.ca/free_products/Bariatric_Surgery_in_Canada_EN.pdf
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–72.
Auspitz M, Cleghorn MC, Azin A, et al. Knowledge and perception of bariatric surgery among primary care physicians: a survey of family doctors in Ontario. Obes Surg 2016 [Epub].
Tsuda S, Barrios L, Schneider B, et al. Factors affecting rejection of bariatric patients from an academic weight loss program. Surg Obes Relat Dis. 2009;5(2):199–202.
Sockalingam S, Cassin S, Crawford A, et al. Psychiatric predictors of surgery non-completion following suitability assessment for bariatric surgery. Obes Surg. 2013;23(2):205–11.
Martin M, Beekley A, Kjorstad R, et al. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obest Relat Dis. 2010;6(1):8–15.
DeMaria E, Pate V, Warthen M, et al. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obest Relat Dis. 2010;6(4):347–55.
Afonso B, Rosenthal R, Li K, et al. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obest Relat Dis. 2010;6(1):16–21.
Perlman S, Reinhold R, Nadzam G. How do family practitioners perceive surgery for the morbidly obese? Surg Obest Relat Dis. 2007;3(4):428–33.
Gregory D, Temple JN, Twells L. Patients’ perceptions of waiting for bariatric surgery: a qualitative study. Int J Equity Health. 2013;12:86.
Keating C, Backholder K, Moodie M, et al. Differences in the rates of treatment of severe obesity using bariatric surgery across socioeconomic groups. JAMA Surg. 2015;150(4):367–8.
Stanford F, Kyle T, Claridy M, et al. The influence of an individual’s weight perception on the acceptance of bariatric surgery. Obesity (Silver Spring). 2015;23(2):277–81.
Merrell J, Ashton K, Windover A, et al. Psychological risk may influence drop-out prior to bariatric surgery. Surg Obest Relat Dis. 2012;8(4):463–9.
Lecaros-Bravo J, Cruzat-Mandich C, Diaz-Castrillon F, et al. Bariatric surgery in adults: variables that facilitate and hinder weight loss from patients perspective. Nutr Hosp. 2015;31(4):1504–12. Spanish.
Ide P, Fitzgerald-O’Shea C, Lautz D. Implementing a bariatric surgery program. AORN J. 2013;97(2):195–206.
Moffett J. Twelve tips for “flipping” the classroom. Med Teach. 2014;37:1–6.
Fortier MA, Bunzli E, Walthall J, Olshansky E, Saadat H, Santistevan R, Mayes L, Kain ZN. Web-based tailored intervention for preparation of parents and children for outpatient surgery (WebTIPS): formative evaluation and randomized controlled trial.
Parry MJ, Watt-Watson J, Hodnett E, et al. Cardiac Home Education and Support Trial (CHEST): a pilot study. Can J Cardiol. 2009;25(12):e393–8.
Acknowledgments
We would like to thank the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kai Yang, Binghao Zhang, Patti Kastanias, Wei Wang, Allan Okraniec, and Sanjeev Sockalingam declare that they have no conflict of interest related to this work.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yang, K., Zhang, B., Kastanias, P. et al. Factors Leading to Self-Removal from the Bariatric Surgery Program After Attending the Orientation Session. OBES SURG 27, 102–109 (2017). https://doi.org/10.1007/s11695-016-2250-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2250-9