Abstract
Background
We investigated the effect of prolonged inspiratory to expiratory (I/E) ratio ventilation on respiratory mechanics, gas exchange, and regional cerebral oxygen saturation (rSO2) in obese patients undergoing laparoscopic bariatric surgery in the reverse Trendelenburg position.
Methods
Twenty-eight adult patients scheduled for laparoscopic sleeve gastrectomy were enrolled in this prospective observational study. After anesthesia induction, pressure-controlled ventilation was conducted initially at a conventional I/E ratio of 1:2 and a positive end-expiratory pressure of 5 cmH2O. Twenty minutes after pneumoperitoneum, the I/E ratio was changed to 1:1 for 20 min and then to 2:1 for 20 min. Hemodynamic variables, end-tidal carbon dioxide tension, rSO2, arterial blood gas analysis results, and respiratory variables were recorded.
Results
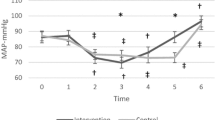
No significant changes in hemodynamic values and rSO2 were observed during the study. Peak airway pressure was significantly lower, but mean airway pressure and dynamic compliance were significantly higher at I/E ratios of 1:1 and 2:1 than during conventional I/E ratio ventilation. Arterial oxygen tension (PaO2) value was significantly higher (p = 0.009), and alveolar-arterial oxygen tension gradient was lower (p = 0.015) at an I/E ratio of 2:1 than during conventional ratio ventilation.
Conclusions
The use of prolonged I/E ratio of 2:1 significantly improved respiratory mechanics and arterial oxygenation without causing hemodynamic derangements or cerebral desaturation during laparoscopic bariatric surgery in the reverse Trendelenburg position.

Similar content being viewed by others
References
Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87(3):654–60.
García-Pérez M, Belda F, Lla J, et al. Changes in chest wall and lung compliance during laparoscopic cholecystectomy. Rev Esp Anestesiol Reanim. 2001;48(4):171–5.
Yanos J, Watling SM, Verhey J. The physiologic effects of inverse ratio ventilation. Chest. 1998;114(3):834–8.
Kim WH, Hahm TS, Kim JA, et al. Prolonged inspiratory time produces better gas exchange in patients undergoing laparoscopic surgery: a randomised trial. Acta Anaesthesiol Scand. 2013;57(5):613–22.
Kim SH, Choi YS, Lee JG, et al. Effects of a 1:1 inspiratory to expiratory ratio on respiratory mechanics and oxygenation during one-lung ventilation in the lateral decubitus position. Anaesth Intensive Care. 2012;40(6):1016–22.
Mousa WF. Equal ratio ventilation (1:1) improves arterial oxygenation during laparoscopic bariatric surgery: a crossover study. Saudi J Anaesth. 2013;7(1):9–13.
Moerman AT, De Hert SG, Jacobs TF, et al. Cerebral oxygen desaturation during beach chair position. Eur J Anaesthesiol. 2012;29(2):82–7.
Kurukahvecioglu O, Sare M, Karamercan A, et al. Intermittent pneumatic sequential compression of the lower extremities restores the cerebral oxygen saturation during laparoscopic cholecystectomy. Surg Endosc. 2008;22(4):907–11.
Lee JR, Lee PB, Do SH, et al. The effect of gynaecological laparoscopic surgery on cerebral oxygenation. J Int Med Res. 2006;34(5):531–6.
Bloomfield GL, Ridings PC, Blocher CR, et al. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit Care Med. 1997;25(3):496–503.
Hardman JG, Aitkenhead AR. Estimation of alveolar dead space fraction using arterial and end-tidal CO2: a factor analysis using a physiological simulation. Anaesth Intensive Care. 1999;27(5):452–8.
Jo YY, Lee JY, Lee MG, et al. Effects of high positive end-expiratory pressure on haemodynamics and cerebral oxygenation during pneumoperitoneum in the Trendelenburg position. Anaesthesia. 2013;68(9):938–43.
Sprung J, Whalley DG, Falcone T, et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg. 2003;97(1):268–74.
Cakar N, Tuŏrul M, Demirarslan A, et al. Time required for partial pressure of arterial oxygen equilibration during mechanical ventilation after a step change in fractional inspired oxygen concentration. Intensive Care Med. 2001;27(4):655–9.
Bardoczky GI, Yernault JC, Houben JJ, et al. Large tidal volume ventilation does not improve oxygenation in morbidly obese patients during anesthesia. Anesth Analg. 1995;81(2):385–8.
Matthay MA, Bhattacharya S, Gaver D, et al. Ventilator-induced lung injury: in vivo and in vitro mechanisms. Am J Physiol Lung Cell Mol Physiol. 2002;283(4):L678–82.
Strandberg A, Tokics L, Brismar B, et al. Constitutional factors promoting development of atelectasis during anaesthesia. Acta Anaesthesiol Scand. 1987;31(1):21–4.
Casati A, Comotti L, Tommasino C, et al. Effects of pneumoperitoneum and reverse Trendelenburg position on cardiopulmonary function in morbidly obese patients receiving laparoscopic gastric banding. Eur J Anaesthesiol. 2000;17(5):300–5.
Soeding PF, Hoy S, Hoy G, et al. Effect of phenylephrine on the haemodynamic state and cerebral oxygen saturation during anaesthesia in the upright position. Br J Anaesth. 2013;111(2):229–34.
Mirro R, Busija D, Green R, et al. Relationship between mean airway pressure, cardiac output, and organ blood flow with normal and decreased respiratory compliance. J Pediatr. 1987;111(1):101–6.
Kwak HJ, Park SK, Lee KC, et al. High positive end-expiratory pressure preserves cerebral oxygen saturation during laparoscopic cholecystectomy under propofol anesthesia. Surg Endosc. 2013;27(2):415–20.
Muench E, Bauhuf C, Roth H, et al. Effects of positive end-expiratory pressure on regional cerebral blood flow, intracranial pressure, and brain tissue oxygenation. Crit Care Med. 2005;33(10):2367–237.
Lessard MR, Guérot E, Lorino H, et al. Effects of pressure-controlled with different I:E ratios versus volume-controlled ventilation on respiratory mechanics, gas exchange, and hemodynamics in patients with adult respiratory distress syndrome. Anesthesiology. 1994;80(5):983–91.
Uttman L, Jonson B. A prolonged postinspiratory pause enhances CO2 elimination by reducing airway dead space. Clin Physiol Funct Imaging. 2003;23(5):252–6.
Koliopanos A, Zografos G, Skiathitis S, et al. Esophageal Doppler (ODM II) improves intraoperative hemodynamic monitoring during laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2005;15(6):332–8.
Conflict of Interest
All authors declare no conflict of interest.
A Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
A Statement of Human and Animal Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jo, Y.Y., Kim, J.Y., Park, C.K. et al. The Effect of Ventilation Strategy on Arterial and Cerebral Oxygenation During Laparoscopic Bariatric Surgery. OBES SURG 26, 339–344 (2016). https://doi.org/10.1007/s11695-015-1766-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1766-8