Abstract
Background
The purpose of this study is to determine the effects of posture and drink volume on gastric/pouch emptying (G/PE), intestinal transit, hormones, absorption, glycaemia, blood pressure and gastrointestinal (GI) symptoms after gastric bypass (Roux-en-Y gastric bypass (RYGB)).
Methods
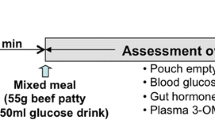
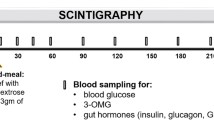
Ten RYGB subjects were studied on four occasions in randomized order (sitting vs. supine posture; 50 vs. 150 ml of labelled water mixed with 3 g 3-O-methyl-d-glucose (3-OMG) and 50 g glucose). G/PE, caecal arrival time (CAT), blood glucose, plasma insulin, glucagon-like peptide-1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), peptide YY (PYY), 3-OMG, blood pressure, heart rate and GI symptoms were assessed over 240 min. Controls were ten volunteers with no medical condition or previous abdominal surgery, who were studied with the 150-ml drink in the sitting position.
Results
Compared to controls, PE (P < 0.001) and CAT (P < 0.001) were substantially more rapid in RYGB subjects. In RYGB, PE was more rapid in the sitting position (2.5 ± 0.7 vs. 16.6 ± 5.3 min, P = 0.02) and tends to be faster after 150 ml than the 50-ml drinks (9.5 ± 2.9 vs. 14.0 ± 3.5 min, P = 0.16). The sitting position and larger volume drinks were associated with greater releases of insulin, GLP-1 and PYY, as well as more hypotension (P < 0.01), tachycardia (P < 0.01) and postprandial symptoms (P < 0.001).
Conclusions
Pouch emptying, blood pressure and GI symptoms after RYGB are dependent on both posture and meal volume.





Similar content being viewed by others
References
Anvari M, Horowitz M, Fraser R, Maddox A, Myers J, Dent J, et al. Effects of posture on gastric emptying of nonnutrient liquids and antropyloroduodenal motility. Am J Physiol. 1995;268:G868–71.
Jones KL, O’Donovan D, Horowitz M, Russo A, Lei Y, Hausken T. Effects of posture on gastric emptying, transpyloric flow, and hunger after a glucose drink in healthy humans. Dig Dis Sci. 2006;51:1331–8.
Horowitz M, Jones K, Edelbroek MA, Smout AJ, Read NW. The effect of posture on gastric emptying and intragastric distribution of oil and aqueous meal components and appetite. Gastroenterology. 1993;105:382–90.
Doran S, Jones KL, Andrews JM, Horowitz M. Effects of meal volume and posture on gastric emptying of solids and appetite. Am J Physiol. 1998;275:R1712–8.
Hellstrom PM, Gryback P, Jacobsson H. The physiology of gastric emptying. Best Pract Res Clin Anaesthesiol. 2006;20:397–407.
Jones KL, O’Donovan D, Russo A, Meyer JH, Stevens JE, Lei Y, et al. Effects of drink volume and glucose load on gastric emptying and postprandial blood pressure in healthy older subjects. Am J Physiol Gastrointest Liver Physiol. 2005;289:G240–8.
Asmar M. New physiological effects of the incretin hormones GLP-1 and GIP. Dan Med Bull. 2011;58:B4248.
Lin HC, Elashoff JD, Gu YG, Meyer JH. Nutrient feedback inhibition of gastric emptying plays a larger role than osmotically dependent duodenal resistance. Am J Physiol. 1993;265:G672–6.
Lin HC, Doty JE, Reedy TJ, Meyer JH. Inhibition of gastric emptying by sodium oleate depends on length of intestine exposed to nutrient. Am J Physiol. 1990;259:G1031–6.
Yamamoto H, Mori T, Tsuchihashi H, Akabori H, Naito H, Tani T. A possible role of GLP-1 in the pathophysiology of early dumping syndrome. Dig Dis Sci. 2005;50:2263–7.
Gebhard B, Holst JJ, Biegelmayer C, Miholic J. Postprandial GLP-1, norepinephrine, and reactive hypoglycemia in dumping syndrome. Dig Dis Sci. 2001;46:1915–23.
Tice JA, Karliner L, Walsh J, Petersen AJ, Feldman MD. Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med. 2008;121:885–93.
Nguyen NQ, Game P, Bessell J, Debreceni TL, Neo M, Burgstad CM, et al. Outcomes of Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding. World J Gastroenterol. 2013;19:6035–43.
Dirksen C, Damgaard M, Bojsen-Moller KN et al. Fast pouch emptying, delayed small intestinal transit, and exaggerated gut hormone responses after Roux-en-Y gastric bypass. Neurogastroenterol Motil. 2013;25:346–e255. doi:10.1111/nmo.12087
Laurenius A, Olbers T, Naslund I, Karlsson J. Dumping syndrome following gastric bypass: validation of the dumping symptom rating scale. Obes Surg. 2013;23:740–55.
Nguyen NQ, Debreceni TL, Bambrick JE et al. Rapid gastric and intestinal transit is a major determinant of changes in blood glucose, intestinal hormones, glucose absorption, and postprandial symptoms after gastric bypass. Obesity (Silver Spring). 2014;22:2003–9. doi:10.1002/oby.20791
Pilichiewicz AN, Little TJ, Brennan IM, Meyer JH, Wishart JM, Otto B, et al. Effects of load, and duration, of duodenal lipid on antropyloroduodenal motility, plasma CCK and PYY, and energy intake in healthy men. Am J Physiol Regul Integr Comp Physiol. 2006;290:R668–77.
Gentilcore D, Doran S, Meyer JH, Horowitz M, Jones KL. Effects of intraduodenal glucose concentration on blood pressure and heart rate in healthy older subjects. Dig Dis Sci. 2006;51:652–6.
Dirksen C, Damgaard M, Bojsen-Moller KN, Jorgensen NB, Kielgast U, Jacobsen SH, et al. Fast pouch emptying, delayed small intestinal transit, and exaggerated gut hormone responses after Roux-en-Y gastric bypass. Neurogastroenterol Motil. 2013;25:346–e255.
Pellegrini CA, Deveney CW, Patti MG, Lewin M, Way LW. Intestinal transit of food after total gastrectomy and Roux-Y esophagojejunostomy. Am J Surg. 1986;151:117–25.
Anderwald CH, Tura A, Promintzer-Schifferl M, Prager G, Stadler M, Ludvik B, et al. Alterations in gastrointestinal, endocrine, and metabolic processes after bariatric Roux-en-Y gastric bypass surgery. Diabetes Care. 2012;35:2580–7.
Bennink R, Peeters M, Van den Maegdenbergh V, Geypens B, Rutgeerts P, De Roo M, et al. Evaluation of small-bowel transit for solid and liquid test meal in healthy men and women. Eur J Nucl Med. 1999;26:1560–6.
Vanis L, Gentilcore D, Rayner CK, Wishart JM, Horowitz M, Feinle-Bisset C, et al. Effects of small intestinal glucose load on blood pressure, splanchnic blood flow, glycemia, and GLP-1 release in healthy older subjects. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1524–31.
Carswell KA, Vincent RP, Belgaumkar AP et al. The effect of bariatric surgery on intestinal absorption and transit time. Obes Surg. 2014;24:796–805. doi:10.1007/s11695-013-1166-x.
Lawaetz O, Blackburn AM, Bloom SR, Aritas Y, Ralphs DN. Gut hormone profile and gastric emptying in the dumping syndrome. A hypothesis concerning the pathogenesis. Scand J Gastroenterol. 1983;18:73–80.
Author Contribution
NN, CR, GW and MH designed the research. TD and CB conducted the research. MB provided the essential material. JW and NN analyzed the data. NN wrote the paper and has the primary responsibility for the final content. All authors read and approved the final manuscript.
Funding
This study was supported by funding from a National Health and Medical Research Council grant.
Conflict of Interest
No authors have any conflict of interest to declare
Author information
Authors and Affiliations
Corresponding author
Additional information
What is already known about the subject?
• In health, posture and meal volume exert little effect on gastric emptying (GE) of either solids or high-nutrient liquids.
• Roux-en-Y gastric bypass (RYGB) allows rapid transit of nutrients into the small intestine which may account for changes in gut hormone secretion and, potentially, “dumping syndrome”.
• The impact of posture and meal volume on GI transit, absorption and symptoms in these patients has not been investigated.
What does this research add?
• In RYGB subjects, the sitting posture was associated with more rapid pouch emptying, increased hypotension and postprandial symptoms.
• Compared to the effects of posture, those of drink volume were relatively minor.
• In RYGB subjects with “problematic dumping syndrome”, ingestion of small-volume meals in the supine or semi-supine posture may potentially minimize adverse haemodynamic changes and GI symptoms.
Rights and permissions
About this article
Cite this article
Nguyen, N.Q., Debreceni, T.L., Burgstad, C.M. et al. Effects of Posture and Meal Volume on Gastric Emptying, Intestinal Transit, Oral Glucose Tolerance, Blood Pressure and Gastrointestinal Symptoms After Roux-en-Y Gastric Bypass. OBES SURG 25, 1392–1400 (2015). https://doi.org/10.1007/s11695-014-1531-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1531-4