Abstract
A leading neurological hypothesis for autism postulates amygdala dysfunction. This hypothesis has considerable support from anatomical and neuroimaging studies. Individuals with bilateral amygdala lesions show impairments in some aspects of social cognition. These impairments bear intriguing similarity to those reported in people with autism, such as impaired recognition of emotion in faces, impaired theory of mind abilities, failure to fixate eyes in faces, and difficulties in regulating personal space distance to others. Yet such neurological cases have never before been assessed directly to see if they meet criteria for autism spectrum disorders (ASD). Here we undertook such an investigation in two rare participants with developmental-onset bilateral amygdala lesions. We administered a comprehensive clinical examination, as well as the Autism Diagnostic Observation Schedule (ADOS), the Social Responsiveness Scale (SRS), together with several other standardized questionnaires. Results from the two individuals with amygdala lesions were compared with published norms from both healthy populations as well as from people with ASD. Neither participant with amygdala lesions showed any evidence of autism across the array of different measures. The findings demonstrate that amygdala lesions in isolation are not sufficient for producing autistic symptoms. We suggest instead that it may be abnormal connectivity between the amygdala and other structures that contributes to autistic symptoms at a network level.
Similar content being viewed by others
Human social behavior is distinguished from the affiliative behavior of other animals in several respects. While many animal species guide their social behavior based on perception of cues in a variety of sensory modalities (such as the detection of pheromones in mating behaviors, and the use of facial expressions and body postures to establish social hierarchies), it is our capacity for complex social cognition that stands out and likely accounts for much of what is unique about human society. Social cognition involves integrating multiple sources of sensory input, contextual cues, and memories as we generate attributions and inferences about others (Adolphs 2010a). Social neuroscience has identified a network of structures that implement human social cognition, one of which is the amygdala.
Amygdala pathology has been specifically hypothesized to account for the social impairments seen in autism spectrum disorders (ASD) (Baron-Cohen et al. 2000; Damasio and Maurer 1978), an idea that has fueled a large number of different studies ever since histological abnormalities were first reported in the amygdala in post-mortem examination (M. Bauman and Kemper 1985). For instance, abnormal cell packing density has been reported in modern stereological studies (Schumann and Amaral 2006), and morphometric studies have found an abnormal developmental trajectory of amygdala volume in autism using structural MRI (Mosconi et al. 2009; Nacewicz et al. 2006; Schumann et al. 2009; Schumann et al. 2004).
These structural findings are now complemented by a rapidly growing body of studies using functional neuroimaging. Earlier studies using positron emission tomography (PET) reported amygdala hypoactivation while making social inferences (Baron-Cohen et al. 1999), and more recent studies using fMRI have argued that abnormal amygdala activation may be related to abnormal fixations onto faces (Dalton et al. 2005) and hyperactive response to social stimuli (Kleinhans et al. 2009). A number of other neuroimaging studies have noted abnormal amygdala activation when people with ASD process faces (Pelphrey et al. 2007; Pierce et al. 2004). While the direction of the “abnormality” is inconsistent across studies (with some finding hypo- and some hyper-activation), taken collectively the findings fit broadly with an emerging literature that has identified the amygdala as a key node in a network for social information processing (Aggleton 2000; Buchanan et al. 2009), as well as with the finding that impairments on social cognition tasks constitute one of the most reliable impairments in autism (Losh et al. 2009). Dysfunction in the neural structures that mediate social cognition has thus been a recurring theme in recent studies of autism (Pelphrey et al. 2005; Schultz 2005). An important complement to that literature would be direct tests of the causal role of the putative brain structures in the social aspects of autism symptomatology, a line of investigation requiring experimental or natural neurological lesions.
Emphasis on the amygdala in social cognition originally derived from a large literature going back to Kluver and Bucy’s classical lesion studies in monkeys (Kluver and Bucy 1939), which reported abnormal emotional and social behavior following extensive bilateral temporal lesions that included the amygdala. More modern studies have produced a somewhat complex array of findings. Monkeys with amygdala lesions can exhibit reduced eye contact, avoid social encounters, have inexpressive faces, lack normal play behaviors, and show locomotor stereotypies and increases in self-directed behaviors that all bear some resemblance to autism in humans (Bachevalier et al. 2001). However, other studies have found more complex and subtle abnormalities, such as increased social approach behavior in adult animals yet reduced social approach and increased social anxiety in infant animals (Prather et al. 2001). Taken together, the pattern of results in monkeys has not provided compelling support for the idea that the amygdala is necessary for producing the full repertoire of social behaviors (Amaral et al. 2003), but suggests instead that the amygdala may play a more complex modulatory role during the inferential and interpretive process of social cognition (see “Discussion”).
Damage to the amygdala in humans arises most frequently from neurosurgical temporal lobectomy for the treatment of epilepsy. However, those lesions are unilateral and typically result in considerably milder abnormalities than seen with bilateral damage. Bilateral amygdala damage can arise from acute encephalitis, but this invariably damages several structures in the medial temporal lobe, including the hippocampus, and is typically associated with a dense amnesia and other symptoms resulting from extra-amygdala damage that make interpretations difficult. The most specific bilateral lesions of the amygdala result from very rare constellations of events (e.g., a combination of neurosurgical and/or vascular (Phelps et al. 1998; Young et al. 1996)) or from Urbach-Wiethe disease (Adolphs et al. 1999; Babinsky et al. 1993). Urbach-Wiethe disease, also called lipoid proteinosis, is an extremely rare genetic disease (Hamada and al. 2002; Hofer 1973), although a few studies with samples of 10 or more subjects have now been published (Siebert et al. 2003; Thornton et al. 2008). Bilateral amygdala damage from Urbach-Wiethe disease results in variable impairments; in some patients it impairs aspects of social cognition that bear superficial resemblance to some components of the social phenotype in autism, including impaired recognition of emotion and other social cues from faces (Adolphs et al. 1998; Adolphs et al. 1999), impaired theory-of-mind abilities (Stone et al. 2003), and impaired regulation of the social distance to others (Kennedy et al. 2009). Particularly intriguing have been close parallels between people with autism, the broad autism phenotype, and patients with bilateral amygdala lesions in a strikingly specific failure to make use of information from the eye region of faces (Adolphs et al. 2005; Adolphs et al. 2008; Spezio et al. 2007a), an impairment related to their failure to fixate normally eyes in faces (Adolphs et al. 2005; Pelphrey et al. 2002; Spezio et al. 2007b).
Despite the frequent finding of abnormal amygdala function in autism, and the several parallels in aspects of abnormal social cognition between individuals with autism and individuals with bilateral amygdala lesions, the latter have to date never been assessed directly with respect to autistic symptomatology. Do individuals with complete bilateral damage to the amygdala meet behavioral criteria for an ASD? Do they meet criteria, or show elevated scores, on instruments such as the ADOS? Answers to these questions would fill an important gap in our understanding of how directly the amygdala might contribute to impaired social behavior in autism, and we undertake such an investigation in the present study.
Methods
Participants
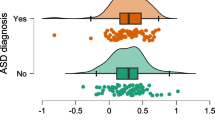
We tested two women with bilateral damage to the amygdala who have IQ, language, perceptual and motor functions all in the normal range (Buchanan et al. 2009). Both patients have bilateral developmental amygdala lesions resulting from Urbach-Wiethe disease. Subject SM is a 43-year-old woman with a high-school education (full-scale IQ = 88), whose lesions encompass the entire amygdala plus subjacent white matter and anterior entorhinal cortex. Subject AP is a 23-year-old woman with a college education (full-scale IQ = 98). Her lesions are entirely confined to the amygdala, and occupy roughly 50% of each amygdala’s volume (Fig. 1).
Subject SM has been studied in great detail previously. The completeness of her lesion to the amygdala is paralleled by her neuropsychological dissociation; while performing in the normal range on standardized tests of IQ, memory, language and perception (Buchanan et al. 2009), she is severely impaired in fear conditioning (Bechara et al. 1995), and in recognizing fear from facial expressions (Adolphs et al. 1995), which are known consequences of amygdala damage.
SM’s first MRI scan was taken during her early twenties, showing clear indications of bilateral amygdala calcifications (Tranel and Hyman 1990), and AP’s first MRI scan was taken when she was fourteen, showing partial bilateral amygdala calcification. There is evidence that the medial temporal calcifications caused by Urbach-Wiethe disease are not entirely congenital, but progressively develop over the course of childhood and adolescence (Appenzeller et al. 2006; Buchanan et al. 2009). In fact, there is a growing consensus that the intracranial calcifications typically begin to emerge sometime around 10 years of age (Appenzeller et al. 2006; Aroni et al. 1998; Claeys et al. 2007; Staut and Naidich 1998). This estimate is also consistent with what we know about the history of our two participants. Both reported occasional abnormal sensations (associated with feelings of anxiety or panic, as well as olfactory sensations) that would be expected by abnormal amygdala activity due to progressive calcification, around this age. SM’s autobiographical recollection suggests that she experienced fear prior to age 10, but not thereafter. All of these observations lead us to believe that both SM and AP acquired amygdala lesions in early adolescence, which progressed to complete lesions in the case of SM by age 20, and partial lesions in the case of AP.
Finally, it is important to note that the phenotype of Urbach-Wiethe disease is not restricted to the central nervous system, but can involve other organs. The skin shows abnormal collagen synthesis and scarring in response to injury. The vocal chords are abnormally thickened, resulting in a hoarse voice in both of our participants. SM has had a hysterectomy likely prompted in part by abnormal epithelial growth of her uterus.
Experimental protocol
Assessment involved a battery of interview- and questionnaire-based tasks which we briefly describe here. The ADOS (Lord et al. 2000), is considered the “gold standard” in the field due to its diagnostic accuracy based on validation studies. Module 4 of the ADOS was administered to both participants by one of the co-authors (C.C.), who has many years of extensive experience with the ADOS and has achieved reliability under the person who developed the instrument (Dr. Catherine Lord). The Social Responsiveness Scale (SRS) (Constantino and Gruber 2005) is a questionnaire focusing on social difficulties present in individuals with ASD consisting of 65 behaviors organized into 5 domains. The adult version of the SRS was completed as a self-rating form by our participants (pre-publication version of this measure provided by Western Psychological Services). The Empathizing Quotient (EQ) and Systemizing Quotient - Revised (SQ-R) questionnaires are self-report instruments that assess the drive to identify others’ thoughts or emotions (EQ) and the drive to understand and construct lawful systems for governing behavior (SQ-R), and higher SQ/EQ ratios are associated with autism spectrum disorders (Wheelwright et al. 2006). Both subjects also received a comprehensive diagnostic interview, including administration of the Mini International Neuropsychiatric Interview conducted by a licensed clinical psychologist (L.K.P.).
A number of supplementary questionnaires were administered; while not used to diagnose autism, these might provide additional points of similarities or differences. Social Anxiety Scale (SAS), State-Trait Anxiety Inventory -Form Y (STAI), and Social Phobia and Anxiety Inventory (SPAI) were administered because many autistic individuals also have significant comorbid anxiety. Adaptive real-life behavior was assessed with the Adaptive Behavior Assessment System II (ABAS-II), which assesses general adaptive functioning related to conceptual skills, social functioning, and practical activities. We were unfortunately unable to administer the Autism Diagnostic Interview (ADI; (Lord et al. 1994)), another well-validated instrument commonly used to diagnose autism, since no primary caregivers familiar with the childhood history of our participants were available.
All participants in this study gave informed consent under a protocol approved by the institutional review board of the California Institute of Technology.
Results
Both SM and AP were alert, fully oriented and cooperative. In clinical interviews, neither merited a psychiatric diagnosis according to DSM-IV criteria. SM’s psychosocial history is notable for social isolation and bullying by peers during school years and into adulthood and she has been unable to sustain employment but lives independently. AP is well-adjusted, college-educated, and currently holds a teaching job. Neither participant came close to meeting criteria for an ASD on clinical interview, nor did either qualify for an additional psychiatric diagnosis.
Across measures of anxiety and phobia, no abnormalities were noted (Table 1), consistent with previously documented mood and personality measures that were all in the normal range (Buchanan et al. 2009). On the ABAS-II, all of AP’s subscale scores were above average while SM scored in borderline range in social functioning, consistent with her real-life situation (Table 2). Neither AP nor SM differed from female controls on measures of systematizing or empathizing (Table 3) (SM’s est AQ = 16.65 (z = .21) and AP’s est AQ = 15.51 (z = 0)). Relative to gender-matched subjects with Asperger’s Syndrome or High-functioning Autism, both AP & SM had significantly higher empathizing scores (Wheelwright et al. 2006).
Neither participant met criteria for autism or any other ASD on the ADOS or the SRS (Table 4). On the ADOS, both participants demonstrated good nonverbal communication, using varied and appropriate facial expressions, typical eye contact as judged by the experimenter, and a range of descriptive and conventional gestures. Both participants also demonstrated understanding of social relationships and emotions, as well as awareness of responsibility for their own wellbeing. Both participants effectively engaged in conversation during the assessment. Neither participant used any stereotyped, repetitive, or pedantic speech, nor did either engage in repetitive behaviors or show evidence of restricted interests during the assessment.
Although neither participant met criteria for an autism or ASD diagnosis, they each had at least one atypical item score within the social or communication domains on the ADOS. AP, the participant who exhibits less amygdala damage, received only one atypical score, which was the result of her lack of inquiry about the examiner’s comments during conversation. In contrast, SM had several item-scores indicative of atypical communication and social interaction. SM exhibited more inquiry into the examiner’s comments than did AP, but not as much as expected. In addition, SM was socially naïve and disinhibited in her interactions with the examiner, leading to scores indicating mild impairment on four ADOS items: Emphatic or emotional gestures, Quality of social overtures, Quality of social response, and Rapport. Although SM exhibited intact basic skills in communication and social interaction such as initiating joint attention through coordination of eye gaze and language, her emotional gestures and social interactions were often poorly integrated, somewhat exaggerated, impulsive, and inappropriate. She often touched the examiner and joked with her in an overly familiar manner (this was the first time she had met the experimenter). Despite these atypical social behaviors, neither participant met diagnostic criteria for ASD in either the Communication or Reciprocal Social Interaction domains of the ADOS.
Discussion
We assessed two rare individuals with developmental bilateral amygdala lesions using a comprehensive battery of interviews, behavioral observations, and questionnaires widely used to diagnose ASD. Across all tasks, our two participants exhibited no distinctively autistic symptomatology. Although participant SM, with complete amygdala lesions, did exhibit some atypical social behaviors during testing and reported social difficulties in daily life, her social impairments were not consistent with those seen in autism. Participant AP, who retained approximately 50% of her amygdala volume, did not exhibit any abnormalities in social behavior. Taken together, the results argue that the amygdala is not essential for the aspects of social behavior that are diagnostically characteristic of autism. On the other hand, the results do not argue against some role for the amygdala in autism, a more complex issue we take up next.
We believe that these results support an alternative emerging view: that the amygdala functions together with other structures in a system for social cognition (Adolphs 2010b). An emphasis on connectivity, rather than on overt pathology intrinsic to the amygdala, could incorporate a role for the amygdala in aspects of the social phenotype of autism while respecting the negative findings of the present study. Abnormal connectivity has been reported in a number of studies of ASD (Alexander et al. 2007; Belmonte et al. 2004; Belmonte and Baron-Cohen 2005; Cascio et al. 2006; Geschwind and Levitt 2007; Vidal et al. 2006). Some specific functional consequences of such abnormal connectivity are now being reported as well, using coherence between the BOLD signal measured in the amygdala and other regions with which it is connected (e.g., Kleinhans et al. 2008). Such abnormal connectivity of the amygdala with other brain structures could be consistent with abnormal BOLD signal within the amygdala, since BOLD-fMRI reflects primarily synaptic metabolic activity and could thus differ with different strengths of input to the amygdala. An emphasis on abnormal connectivity could also be reconciled with the several studies that have noted enlarged amygdalae in autism early in life (Mosconi et al. 2009; Schumann et al. 2009, 2004), since neuropil density, and hence overall volume, could reflect the development of such abnormal connectivity.
Which connections might be most important to consider? Of particular interest is amygdala connectivity with other structures that collaborate in motivation and reward learning, such as medial prefrontal cortex, ventral striatum, and nucleus accumbens. For instance, in animal studies, disconnection of the amygdala and orbitofrontal cortex results in deficits on reward learning tasks that are as severe as those caused by lesions to either structure in isolation (Baxter et al. 2000). Similarly, disconnection of the amygdala from the nucleus accumbens in rats disrupts instrumental behavior towards rewards (Ambroggi et al. 2008). In humans, the connections between amygdala and the prefrontal cortex in particular have been highlighted in regard to genetic polymorphisms and susceptibility to psychiatric illness (Mayberg et al. 1999). Of great interest has been a polymorphism in the promotor region of the serotonin reuptake transporter (5HTTLPR), which some studies have associated with risk of psychiatric illness, as well as with changes in BOLD signal within the amygdala while processing emotional facial expressions (Munafo et al. 2008); it has also been reported to be associated with individual differences in anxious temperament and scanpaths to faces in monkeys (Gibboni et al. 2009). More recently, a number of studies have found that the polymorphism is associated also with systematic changes in the strength of both structural and functional connectivity between amygdala and medial parts of the prefrontal cortex (Heinz et al. 2005; Pezawas et al. 2005; Pacheco et al. 2009), with consequences for psychopathology (Pezawas et al. 2005), trait anxiety (Kim and Whalen 2009), as well as for aspects of decision-making (Roiser et al. 2009). It thus remains quite possible that dysfunction of the amygdala will constitute a useful marker of the impaired social cognition that underlies autism, even if it is not the primary causal factor of autistic behavior.
This more nuanced interpretation of the role of the amygdala in social behavior, and its possible contribution to social dysfunction in autism, fits with the literature on amygdala lesions in monkeys. In monkeys, earlier lesions that were nonselective resulted in severe impairments in social behavior with the result that the monkeys lost their social status (Rosvold et al. 1954) and were ostracized by the group, resulting in death in the wild (Kling and Brothers 1992). Selective neurotoxic lesions resulted in more subtle impairments that were quite complex and depended on other factors. One study found that the amygdalectomized monkeys showed more prosocial cues and less avoidance behaviors towards other (healthy) monkeys when in dyadic interactions, with the result that they were actually approached more and groomed more by other monkeys (Emery et al. 2001). They also showed more approach behavior towards unfamiliar humans, consistent with their increase in prosocial behaviors. However, in more complex groups (the lesioned monkey together with three healthy monkeys in a tetrad) these effects were not seen, and instead a quite subtle increase in avoidance and stress behaviors was shown by other monkeys towards the amygdalectomized monkey (Machado and Bachevalier 2006). Further complexities arise if the lesions are made neonatally: for instance, exaggerated social fear (yet with the typically diminished fear of novel objects) has been reported in such lesioned monkeys (Bauman et al. 2004), although this profile appears to change as the monkeys age (Toscano et al. 2009).
Two important take-home messages from the monkey lesion studies are that the amygdala’s effect on social behavior is not rigid and universal, but context dependent and susceptible to individual differences; and that even complete lesions of the amygdala appear to leave the repertoire of social behaviors as such largely intact—they just are not elicited in a context-appropriate way (Amaral et al. 2003). For instance, monkeys with amygdala lesions can still respond normally to social stimuli such as a human stare, even though they show blunted avoidance responses to potential predators such as a snake (Machado et al. 2009). While the socioemotional changes in monkeys with amygdala lesions appear to constitute a stable behavioral change that can be thought of as a trait change in personality (Mason et al. 2006), it is neither a change in the ability to show the full repertoire of social behaviors (Amaral et al. 2003) nor a change in mood as such (Kalin et al. 2001). Rather, it is probably best thought of as a consistent change in the way that context-dependent situations (stimuli in the context of an emotionally significant or socially significant setting) modulate motivated behavior. Such context-dependency highlights the flexible nature of social cognition, and emphasizes a role for the amygdala beyond social perception and sensory processing.
There are several possible alternative explanations for why amygdala lesions failed to reproduce autistic symptoms in our study. One plausible differentiating factor is age of lesion-onset. Although both autism and Urbach-Wiethe disease are developmental conditions, Urbach-Wiethe disease may impact amygdala development at a later stage than does autism. While unusual social behaviors are apparent in the first three years of life in autism, the amygdala lesions in Urbach-Wiethe disease are believed to begin around age 10 (although this is not known with certainty and may well vary considerably between individuals). Unfortunately, we were unable to obtain data from the ADI (Lord et al. 1994) in our study, which would have provided a window into the early behavioral development of our two participants. However, in light of the negative findings we report here from them as adults, it is unlikely that they showed any autistic symptomatology earlier in life. This may be a key difference as very early amygdala damage could lead to unique and substantial reorganization of the social cognition network in which the amygdala participates, and thus produce specific social aspects of the autism phenotype. This remains an important possibility to consider, especially in light of the above noted differences in monkeys depending on whether they had adult-onset or neonatal amygdala lesions. It is plausible that earlier lesion onset may impede development of meta-cognitive processes that facilitate regulation of actual social behavior, either via alterations in connectivity as described above or simply by biasing an individual toward different life experiences. To address this would require an examination of the behavioral outcome following truly neonatal (or prenatal) lesions of the amygdala in humans.
Finally, it is important to consider the possibility that the behavioral consequences of amygdala lesions show large individual differences, and that a sample of two participants could by chance result in a false negative finding. It could be that a sample of 100 subjects with bilateral amygdala lesions would show a strikingly high incidence of autistic symptoms, yet that two randomly chosen individuals may well not show any. It is worth emphasizing that one of our two patients, AP, only had incomplete damage to the amygdala, and that complete lesions are a pre-requisite for any social impairments resembling autism. Relatedly, it is possible that our instruments simply were insufficiently sensitive to show parallels between our two participants and autism, and that more sensitive behavioral measures would have revealed similarities after all. On this note, it is relevant to keep in mind that the ADOS and SRS were designed to capture the behavioral impairments seen in autism, not social impairments following amygdala lesions or subtle features of social cognition. It is conceivable that broader, or different, assessments of social behavior could reveal some overlap between autism and amygdala lesions after all. A challenging but theoretically interesting future direction would be to conduct the present investigation, as it were, in reverse: to develop behavioral and questionnaire-based measures that capture what is abnormal about social behavior in patients with bilateral amygdala lesions, and apply these tools to people with autism. It is possible that such an approach could uncover subtypes of autism and help to define the boundaries of this heterogeneous disorder as well.
References
Adolphs R. Conceptual challenges and directions for social neuroscience. Neuron. 2010a;65:752–67.
Adolphs R. What does the amygdala contribute to social cognition? Ann NY Acad Sci. 2010b;1191:42–61.
Adolphs R, Tranel D, Damasio H, Damasio AR. Fear and the human amygdala. J Neurosci. 1995;15:5879–92.
Adolphs R, Tranel D, Damasio AR. The human amygdala in social judgment. Nature. 1998;393:470–4.
Adolphs R, Tranel D, Hamann S, Young A, Calder A, Anderson A, et al. Recognition of facial emotion in nine subjects with bilateral amygdala damage. Neuropsychologia. 1999;37:1111–7.
Adolphs R, Gosselin F, Buchanan TW, Tranel D, Schyns PG, Damasio A. A mechanism for impaired fear recognition after amygdala damage. Nature. 2005;433:68–72.
Adolphs R, Spezio ML, Parlier M, Piven J. Distinct face-processing strategies in parents of autistic children. Curr Biol. 2008;18:1090–3.
Aggleton J, editor. The amygdala. A functional analysis. New York: Oxford University Press; 2000.
Alexander AL, Lee JE, Lazar M, Boudos R, DuBray MB, Oakes TR, et al. Diffusion tensor imaging of the corpus callosum in autism. Neuroimage. 2007;34:61–73.
Amaral DG, Capitanio JP, Jourdain M, Mason WA, Mendoza SP, Prather M. The amygdala: is it an essential component of the neural network for social cognition? Neuropsychologia. 2003;41:235–40.
Ambroggi F, Ishikawa A, Fields HL, Nicola SM. Basolateral amygdala neurons facilitate reward-seeking behavior by exciting nucleus accumbens neurons. Neuron. 2008;59:648–61.
Appenzeller S, Chaloult E, Velho P, de Souza EM, Araujo VZ, Cendes F, et al. Amygdalae calcifications associated with disease duration in lipoid proteinosis. J Neuroimaging. 2006;16:154–6.
Aroni K, Lazaris AC, Papadimitriou K, Paraskevakou H, Davaris PS. Lipoid proteinosis of the oral mucosa: a case report and review of the literature. Pathol Res Pract. 1998;194:855–9.
Babinsky R, Calabrese P, Durwen HF, Markowitsch HJ, Brechtelsbauer D, Heuser L, et al. The possible contribution of the amygdala to memory. Behav Neurol. 1993;6:167–70.
Bachevalier J, Malkova L, Mishkin M. Effects of selective neonatal temporal lobe lesions on socioemotional behavior in infant rhesus monkeys. Behav Neurosci. 2001;115:545–59.
Baron-Cohen S, Ring HA, Wheelwright S, Bullmore ET, Brammer MJ, Simmons A, et al. Social intelligence in the normal and autistic brain: an fMRI study. Eur J Neurosci. 1999;11(6):1891–8.
Baron-Cohen S, Ring HA, Bullmore ET, Wheelwright S, Ashwin C, Williams SC. The amygdala theory of autism. Neurosci Biobehav Rev. 2000;24(3):355–64.
Bauman M, Kemper TL. Histoanatomic observations of the brain in early infantile autism. Neurology. 1985;35:866–74.
Bauman MD, Lavenex P, Mason WA, Capitanio JP, Amaral DG. The development of social behavior following neonatal amygdala lesions in rhesus monkeys. J Cogn Neurosci. 2004;16:1388–411.
Baxter MG, Parker A, Lindner CCC, Izquierdo AD, Murray EA. Control of response selection by reinforcer value requires interaction of amygdala and orbital prefrontal cortex. J Neurosci. 2000;20:4311–9.
Bechara A, Tranel D, Damasio H, Adolphs R, Rockland C, Damasio AR. Double dissociation of conditioning and declarative knowledge relative to the amygdala and hippocampus in humans. Science. 1995;269:1115–8.
Belmonte MK, Baron-Cohen S. Autism: a window onto the development of the social and the analytic brain. Annu Rev Neurosci. 2005;28:109–26.
Belmonte MK, Allen G, Beckel-Mitchener A, Boulanger LM, Carper RA, Webb SJ. Autism and abnormal development of brain connectivity. J Neurosci. 2004;24(42):9228–31.
Buchanan TW, Tranel D, Adolphs R. The human amygdala in social function. In: Whalen PW, Phelps L, editors. The human amygdala. New York: Oxford University Press; 2009. p. 289–320.
Cascio C, Styner M, Smith RG, Poe MD, Gerig G, Hazlett HC, et al. Reduced relationship to cortical white matter volume revealed by tractography-based segmentation of the corpus callosum in young children with developmental delay. Am J Psychiatry. 2006;163:2157–63.
Claeys KG, Claes LRF, Van Gothem JWM, Sercu S, Merregaert J, Lambert J, et al. Epilepsy and migraine in a patient with Urbach-Wiethe disease. Seizure. 2007;16:465–8.
Constantino J, Gruber C. The social responsiveness scale: Western Psychological Services. 2005.
Dalton KM, Nacewicz BM, Johnstone T, Schaefer HS, Gernsbacher MA, Goldsmith HH, et al. Gaze fixation and the neural circuitry of face processing in autism. Nat Neurosci. 2005;8:519–26.
Damasio AR, Maurer RG. A neurological model for childhood autism. Arch Neurol. 1978;35:777–86.
Emery NJ, Capitanio JP, Mason WA, Machado CJ, Mendoza SP, Amaral DG. The effects of bilateral lesions of the amygdala on dyadic social interactions in rhesus monkeys. Behav Neurosci. 2001;115:515–44.
Geschwind DH, Levitt P. Autism spectrum disorders: developmental disconnection syndromes. Curr Opin Neurobiol. 2007;17:103–11.
Gibboni RR, Zimmerman PE, Gothard KM. Individual differences in scanpaths correspond with serotonin transporter genotype and behavioral phenotypes in rhesus monkeys (Macaca mulatta). Front Behav Neurosci. 2009;3, article 50.
Hamada T, al. e. Lipoid proteinosis maps to 1q21 and is caused by mutations in the extracellular matrix protein 1 gene (ECM1). Hum Mol Gen. 2002;11:833–40.
Heinz A, Braus DF, Smolka MN, Wrase J, Puls I, Hermann D, et al. Amygdala-prefrontal coupling depends on a genetic variation of the serotonin transporter. Nat Neurosci. 2005;8:20–1.
Hofer P-A. Urbach-Wiethe disease: a review. Acta Derm Venerol. 1973;53:5–52.
Kalin NH, Shelton SE, Davidson RJ, Kelley AE. The primate amygdala mediates acute fear but not the behavioral and physiological components of anxious temperament. J Neurosci. 2001;21:2067–74.
Kennedy DP, Gläscher J, Tyszka JM, Adolphs R. Personal space regulation by the human amygdala. Nat Neurosci. 2009;12:1226–7.
Kim MJ, Whalen PJ. The structural integrity of an amygdala-prefrontal pathway predicts trait anxiety. J Neurosci. 2009;29:11614–8.
Kleinhans NM, Richards T, Sterling L, Stegbauer KC, Mahurin R, Johnson LC, et al. Abnormal functional connectivity in autism spectrum disorders during face processing. Brain. 2008;131:1000–12.
Kleinhans NM, Johnson LC, Richards T, Mahurin R, Greenson J, Dawson G, et al. Reduced neural habituation in the amygdala and social impairments in autism spectrum disorders. Am J Psychiatry. 2009;166:467–75.
Kling AS, Brothers LA. The amygdala and social behavior. In: Aggleton JP, editor. The amygdala: neurobiological aspects of emotion, memory, and mental dysfunction. New York: Wiley-Liss; 1992.
Kluver H, Bucy PC. Preliminary analysis of functions of the temporal lobes in monkeys. Arch Neurol Psychiatry. 1939;42:979–97.
Lord C, Rutter M, Le Couteur A. Autism diagnostic interview- revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24:659–85.
Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–23.
Losh M, Adolphs R, Poe M, Couture S, Penn D, Baranek G, et al. Neuropsychological profile of autism and broad autism phenotype. Arch Gen Psychiatry. 2009;66:518–26.
Machado CJ, Bachevalier J. The impact of selective amygdala, orbital frontal cortex, or hippocampal formation lesions on established social relationships in rhesus monkeys. Behav Neurosci. 2006;120:761–86.
Machado CJ, Kazama AM, Bachevalier J. Impact of amygdala, orbital frontal, or hippocampal lesions on threat avoidance and emotional reactivity in nonhuman primates. Emotion. 2009;9:147–63.
Mason WA, Capitanio JP, Machado CJ, Mendoza SP, Amaral DG. Amygdalectomy and responsiveness to novelty in rhesus monkeys: generality and individual consistency of effects. Emotion. 2006;6:73–81.
Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, et al. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry. 1999;156:675–82.
Mosconi MW, Cody-Hazlett H, Poe M, Gerig G, Gimpel-Smith R, Piven J. Longitudinal study of amygdala volume and joint attention in 2- to 4-year-old children with autism. Arch Gen Psychiatry. 2009;66:509–16.
Munafo MR, Brown SM, Hariri AR. Serotonin transporter (5-HTTLPR) genotype and amygdala activation: a meta-analysis. Biol Psychiatry. 2008;63:852–7.
Nacewicz BM, Dalton KM, Johnstone T, Long MT, McAuliff EM, Oakes TR, et al. Amygdala volume and nonverbal social impairment in adolescent and adult males with autism. Arch Gen Psychiatry. 2006;63:1417–28.
Pacheco J, Beevers CG, Benavides C, McGeary J, Stice E, Schnyer DM. Frontal-limbic white matter pathway associations with the serotonin transporter gene promoter region (5-HTTLPR) polymorphism. J Neurosci. 2009;29:6229–33.
Pelphrey KA, Sasson NJ, Reznick JS, Paul G, Goldman BD, Piven J. Visual scanning of faces in autism. J Autism Dev Disord. 2002;32:249–61.
Pelphrey KA, Adolphs R, Morris JP. Neuroanatomical substrates of social cognition dysfunction in autism. Ment Retard Dev Disabil Res Rev. 2005;10:259–71.
Pelphrey KA, Morris JP, McCarthy G, LaBar KS. Perception of dynamic changes in facial affect and identity in autism. SCAN. 2007;2:140–50.
Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, et al. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. 2005;8:828–34.
Phelps EA, LaBar K, Anderson AK, O’Connor KJ, Fulbright RK, Spencer D. Specifying the contributions of the human amygdala to emotional memory: a case study. Neurocase. 1998;4:527–40.
Pierce K, Haist F, Sedaghat F, Courchesne E. The brain response to personally familiar faces in autism: Findings of fusiform activity and beyond. Brain. 2004;127:2703–16.
Prather MD, Lavenex P, Mauldin-Jourdain ML, Mason WA, Capitanio JP, Mendoza SP, et al. Increased social fear and decreased fear of objects in monkeys with neonatal amygdala lesions. Neuroscience. 2001;106:653–8.
Roiser JP, deMartino B, Tan GCY, Kumaran D, Seymour B, Wood NW, et al. A genetically mediated bias in decision making driven by failure of amygdala control. J Neurosci. 2009;29:5985–91.
Rosvold HE, Mirsky AF, Pribram K. Influence of amygdalectomy on social behavior in monkeys. J Comp Physiol Psychol. 1954;47:173–8.
Schultz RT. Developmental deficits in social perception in autism: the role of the amygdala and fusiform face area. Int J Dev Neurosci. 2005;23:125–41.
Schumann CM, Amaral DG. Stereological analysis of amygdala neuron number in autism. J Neurosci. 2006;26:7674–9.
Schumann CM, Hamstra J, Goodlin-Jones BL, Lotspeich L, Kwon H, Buonocore MH, et al. The amygdala is enlarged in children but not adolescents with autism; the hippocampus is enlarged at all ages. J Neurosci. 2004;24:6392–401.
Schumann CM, Barnes CC, Lord C, Courchesne E. Amygdala enlargement in toddlers with autism related to severity of social and communication impairments. Biol Psychiatry. 2009;66:942–9.
Siebert M, Markowitsch HJ, Bartel P. Amygdala, affect and cognition: evidence from 10 patients with Urbach-Wiethe disease. Brain. 2003;126:2627–37.
Spezio ML, Adolphs R, Hurley RS, Piven J. Abnormal use of facial information in high-functioning autism. J Autism Dev Disord. 2007a;37(5):929–39.
Spezio ML, Adolphs R, Hurley RSE, Piven J. Analysis of face gaze in autism using “bubbles”. Neuropsychologia. 2007b;45:144–51.
Staut CCV, Naidich TP. Urbach-Wiethe disease (lipoid proteinosis). Pediatr Neurosurg. 1998;28:212–4.
Stone VE, Baron-Cohen S, Young AW, Calder AJ, Keane J. Acquired theory of mind impairments in patients with bilateral amygdala lesions. Neuropsychologia. 2003;41:209–20.
Thornton HB, Nel D, Thornton D, van Honk J, Baker GA, Stein DJ. The neuropsychiatry and neuropsychology of lipoid proteinosis. J Neuropsychiatry Clin Neurosci. 2008;20:86–92.
Toscano JE, Bauman MD, Mason WA, Amaral DG. Interest in infants by female rhesus monkeys with neonatal lesions of the amygdala or hippocampus. Neuroscience. 2009;162:881–91.
Tranel D, Hyman BT. Neuropsychological correlates of bilateral amygdala damage. Arch Neurol. 1990;47:349–55.
Vidal CN, Nicolson R, DeVito TJ, Hayashi KM, Geaga JA, Drost DJ, et al. Mapping corpus callosum deficits in autism: an index of aberrant cortical connectivity. Biol Psychiatry. 2006;60(3):218–25.
Wheelwright N, Baron-Cohen S, al. e. Predicting autism spectrum quotient from the systematizing quotient-revised (SQ-R) and empathy quotient (EQ). Brain Res. 2006; 47–56.
Young AW, Hellawell DJ, Van de Wal C, Johnson M. Facial expression processing after amygdalotomy. Neuropsychologia. 1996;34:31–9.
Acknowledgments
The study was funded through grants from the Simons Foundation Autism Research Initiative, and grant R01MH080721 from the National Institute of Mental Health. We thank Joe Piven for helpful comments on the manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Paul, L.K., Corsello, C., Tranel, D. et al. Does bilateral damage to the human amygdala produce autistic symptoms?. J Neurodevelop Disord 2, 165–173 (2010). https://doi.org/10.1007/s11689-010-9056-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11689-010-9056-1