ABSTRACT
BACKGROUND
Depression and adherence to antidepressant treatment are important clinical concerns in diabetes care. While patient–provider communication patterns have been associated with adherence for cardiometabolic medications, it is unknown whether interpersonal aspects of care impact antidepressant medication adherence.
OBJECTIVE
To determine whether shared decision-making, patient–provider trust, or communication are associated with early stage and ongoing antidepressant adherence.
DESIGN
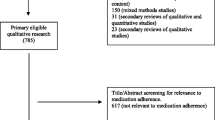
Observational new prescription cohort study.
SETTING
Kaiser Permanente Northern California.
PATIENTS
One thousand five hundred twenty-three adults with type 2 diabetes who completed a survey in 2006 and received a new antidepressant prescription during 2006–2010.
MEASUREMENTS
Exposures included items based on the Trust in Physicians and Interpersonal Processes of Care instruments and the Consumer Assessment of Healthcare Providers and Systems (CAHPS) communication scale. Measures of adherence were estimated using validated methods with physician prescribing and pharmacy dispensing data: primary non-adherence (medication never dispensed), early non-persistence (dispensed once, never refilled), and new prescription medication gap (NPMG; proportion of time without medication during 12 months after initial prescription).
RESULTS
After adjusting for potential confounders, patients’ perceived lack of shared decision-making was significantly associated with primary non-adherence (RR = 2.42, p < 0.05), early non-persistence (RR = 1.34, p < 0.01) and NPMG (estimated 5 % greater gap in medication supply, p < 0.01). Less trust in provider was significantly associated with early non-persistence (RRs 1.22–1.25, ps < 0.05) and NPMG (estimated NPMG differences 5–8 %, ps < 0.01).
LIMITATIONS
All patients were insured and had consistent access to and quality of care.
CONCLUSIONS
Patients’ perceptions of their relationships with providers, including lack of shared decision-making or trust, demonstrated strong associations with antidepressant non-adherence. Further research should explore whether interventions for healthcare providers and systems that foster shared decision-making and trust might also improve medication adherence.


Similar content being viewed by others
REFERENCES
Ratanawongsa N, Karter AJ, Parker MM, et al. Communication and medication refill adherence: the Diabetes Study of Northern California. JAMA Intern Med. 2013;173(3):210–218.
Katon WJ, Simon G, Russo J, et al. Quality of depression care in a population-based sample of patients with diabetes and major depression. Med Care. 2004;42(12):1222–1229.
Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5 Pt 1):1640–1661.
de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–630.
Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160.
Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–2672.
Katon W, Lyles CR, Parker MM, Karter AJ, Huang ES, Whitmer RA. Association of depression with increased risk of dementia in patients with type 2 diabetes: the diabetes and aging study. Arch Gen Psychiatry. 2012;69(4):410–417.
Sullivan MD, O’Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL sub study. Diabetes Care. 2012;35(8):1708–1715.
Hudson DL, Karter AJ, Fernandez A, et al. Differences in the clinical recognition of depression in diabetes patients: the diabetes study of northern California (DISTANCE). Am J Manage Care. 2013;19(5):344–352.
Lin EH, Von Korff M, Katon W, et al. The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care. 1995;33(1):67–74.
Mojtabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. J Clin Psychiatry. 2008;69(7):1064–1074.
Bauer AM, Schillinger D, Parker MM, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. 2013;28(9):1181–1187.
American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd ed. Washington DC: American Psychiatric Association; 2010.
Moffet HH, Adler N, Schillinger D, et al. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)–objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol. 2009;38(1):38–47.
Hargraves JL, Hays RD, Cleary PD. Psychometric properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 adult core survey. Health Serv Res. 2003;38(6 Pt 1):1509–1527.
Anderson LA, Dedrick RF. Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67(3 Pt 2):1091–1100.
Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the trust in physician scale. The Stanford Trust Study Physicians. Med Care. 1999;37(5):510–517.
Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339. 274.
Stewart AL, Napoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42(3 Pt 1):1235–1256.
Agency for Health Care Policy and Research. CAHPS Health Plan Survey 4.0 Supplemental Items for the Adult Questionnaires https://cahps.ahrq.gov/surveys-guidance/item-sets/HP/1157a_engadultsupp_40.pdf. Accessed October 3, 2014.
Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS(R)) clinician and group adult visit survey. Med Care. 2012;50(Suppl):S28–S34.
Raebel MA, Schmittdiel J, Karter AJ, Konieczny JL, Steiner JF. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–S21.
Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48.
Hernan MA, Hernandez-Diaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol. 2002;155(2):176–184.
Zou GY. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706.
Cheung YB. A modified least-squares regression approach to the estimation of risk difference. Am J Epidemiol. 2007;166(11):1337–1344.
Horvitz DG, Thompson DJ. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc. 1952;47(260):663–685.
Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594.
Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26(3):265–271.
Kaplan JE, Keeley RD, Engel M, Emsermann C, Brody D. Aspects of patient and clinician language predict adherence to antidepressant medication. J Am Board Fam Med. 2013;26(4):409–420.
Shin J, McCombs JS, Sanchez RJ, Udall M, Deminski MC, Cheetham TC. Primary nonadherence to medications in an integrated healthcare setting. Am J Manage Care. 2012;18(8):426–434.
Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620.
Lin EH, Von Korff M, Ciechanowski P, et al. Treatment adjustment and medication adherence for complex patients with diabetes, heart disease, and depression: a randomized controlled trial. Ann Fam Med. 2012;10(1):6–14.
DeWalt D, Callahan L, Hawk V, et al. Health literacy universal precautions toolkit (Prepared by North Carolina Network Consortium, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, under Contract No. HHSA290200710014.) AHRQ Publication No. 10-0046-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2010.
Koh HK, Brach C, Harris LM, Parchman ML. A proposed ‘health literate care model’ would constitute a systems approach to improving patients’ engagement in care. Health Aff (Millwood). 2013;32(2):357–367.
Brach C, Keller D, Hernandez L, et al. Ten Attributes of Health Literate Health Care Organizations: National Academy of Sciences; 2012: http://iom.edu/~/media/Files/Perspectives-Files/2012/Discussion-Papers/BPH_Ten_HLit_Attributes.pdf. Accessed October 3, 2014.
Acknowledgements
This research was supported by funding from the National Institutes of Health (R01-DK080726, R01-DK081796, P30-DK092924, and NCATS Grant KL2 TR000421). The research reported in this manuscript was presented at the annual meeting of the Academy of Psychosomatic Medicine in Tuscon, AZ, November 2013.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauer, A.M., Parker, M.M., Schillinger, D. et al. Associations Between Antidepressant Adherence and Shared Decision-Making, Patient–Provider Trust, and Communication Among Adults with Diabetes: Diabetes Study of Northern California (DISTANCE). J GEN INTERN MED 29, 1139–1147 (2014). https://doi.org/10.1007/s11606-014-2845-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2845-6