ABSTRACT
BACKGROUND
Warfarin is effective in preventing thromboembolic events, but concerns exist regarding its use in patients with substance abuse.
OBJECTIVE
Identify which patients with substance abuse who receive warfarin are at risk for poor outcomes.
DESIGN
Retrospective cohort study. Diagnostic codes, lab values, and other factors were examined to identify risk of adverse outcomes.
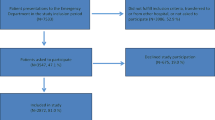
PATIENTS
Veterans AffaiRs Study to Improve Anticoagulation (VARIA) database of 103,897 patients receiving warfarin across 100 sites.
MAIN MEASURES
Outcomes included percent time in therapeutic range (TTR), a measure of anticoagulation control, and major hemorrhagic events by ICD-9 codes.
RESULTS
Nonusers had a higher mean TTR (62 %) than those abusing alcohol (53 %), drugs (50 %), or both (44 %, p < 0.001). Among alcohol abusers, an increasing ratio of the serum hepatic transaminases aspartate aminotransferase/alanine aminotransferase (AST:ALT) correlated with inferior anticoagulation control; normal AST:ALT ≤ 1.5 predicted relatively modest decline in TTR (54 %, p < 0.001), while elevated ratios (AST:ALT 1.50–2.0 and > 2.0) predicted progressively poorer anticoagulation control (49 % and 44 %, p < 0.001 compared to nonusers). Age-adjusted hazard ratio for major hemorrhage was 1.93 in drug and 1.37 in alcohol abuse (p < 0.001 compared to nonusers), and remained significant after also controlling for anticoagulation control and other bleeding risk factors (1.69 p < 0.001 and 1.22 p = 0.003). Among alcohol abusers, elevated AST:ALT >2.0 corresponded to more than three times the hemorrhages (HR 3.02, p < 0.001 compared to nonusers), while a normal ratio AST:ALT ≤ 1.5 predicted a rate similar to nonusers (HR 1.19, p < 0.05).
CONCLUSIONS
Anticoagulation control is particularly poor in patients with substance abuse. Major hemorrhages are more common in both alcohol and drug users. Among alcohol abusers, the ratio of AST/ALT holds promise for identifying those at highest risk for adverse events.

Similar content being viewed by others
REFERENCES
Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–76.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133:160S–98S.
Havrda DE, Mai T, Chonlahan J. Enhanced antithrombotic effect of warfarin associated with low-dose alcohol consumption. Pharmacotherapy. 2005;25:303–7.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 365:981–92.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–52.
Dawson DA, Saha TD, Grant BF. A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug Alcohol Depend. 2010;107:31–8.
Liangpunsakul S, Qi R, Crabb DW, Witzmann F. Relationship between alcohol drinking and aspartate aminotransferase:alanine aminotransferase (AST:ALT) ratio, mean corpuscular volume (MCV), gamma-glutamyl transpeptidase (GGT), and apolipoprotein A1 and B in the U.S. population. J Stud Alcohol Drugs. 2010;71:249–52.
Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Patient characteristics associated with oral anticoagulation control: results of the Veterans AffaiRs Study to Improve Anticoagulation (VARIA). J Thromb Haemost. 2010;8:2182–91.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–95.
Hannuksela ML, Liisanantti MK, Nissinen AE, Savolainen MJ. Biochemical markers of alcoholism. Clin Chem Lab Med. 2007;45:953–61.
Rosendaal FR, Cannegieter SC, van der Meer FJ, Briet E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69:236–9.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3:692–4.
Jasuja GK, Reisman JI, Miller DR, et al. Identifying Major Hemorrhage with Automated Data: Results of the Veterans Affairs Study to Improve Anticoagulation (VARIA). Thrombosis research. 2012.
Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol. 2011;57:173–80.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70.
Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000;160:41–6.
McCormick D, Gurwitz JH, Goldberg RJ, et al. Prevalence and quality of warfarin use for patients with atrial fibrillation in the long-term care setting. Arch Intern Med. 2001;161:2458–63.
Monette J, Gurwitz JH, Rochon PA, Avorn J. Physician attitudes concerning warfarin for stroke prevention in atrial fibrillation: results of a survey of long-term care practitioners. J Am Geriatr Soc. 1997;45:1060–5.
Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010;123:638–45 e4.
Baczek VL, Chen WT, Kluger J, Coleman CI. Predictors of warfarin use in atrial fibrillation in the United States: a systematic review and meta-analysis. BMC Fam Pract. 2012;13:5.
Chen WT, White CM, Phung OJ, et al. Are the risk factors listed in warfarin prescribing information associated with anticoagulation-related bleeding? A systematic literature review. Int J Clin Pract. 2011;65:749–63.
Schauer DP, Moomaw CJ, Wess M, Webb T, Eckman MH. Psychosocial risk factors for adverse outcomes in patients with nonvalvular atrial fibrillation receiving warfarin. J Gen Intern Med. 2005;20:1114–9.
Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118:2029–37.
van Leeuwen Y, Rosendaal FR, Cannegieter SC. Prediction of hemorrhagic and thrombotic events in patients with mechanical heart valve prostheses treated with oral anticoagulants. J Thromb Haemost. 2008;6:451–6.
Veeger NJ, Piersma-Wichers M, Tijssen JG, Hillege HL, van der Meer J. Individual time within target range in patients treated with vitamin K antagonists: main determinant of quality of anticoagulation and predictor of clinical outcome. A retrospective study of 2300 consecutive patients with venous thromboembolism. Br J Haematol. 2005;128:513–9.
Wallentin L, Yusuf S, Ezekowitz MD, et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet. 2010;376:975–83.
White HD, Gruber M, Feyzi J, et al. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007;167:239–45.
Arnason T, Wells PS, van Walraven C, Forster AJ. Accuracy of coding for possible warfarin complications in hospital discharge abstracts. Thromb Res. 2006;118:253–62.
Tamariz L, Harkins T, Nair V. A systematic review of validated methods for identifying venous thromboembolism using administrative and claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):154–62.
White RH, Garcia M, Sadeghi B, et al. Evaluation of the predictive value of ICD-9-CM coded administrative data for venous thromboembolism in the United States. Thromb Res. 2010;126:61–7.
Hastie TJ, Tibshirani RJ. Generalized additive models. New York: Chapman and Hall; 1990.
Acknowledgements
Contributors
No further contributors.
Funding
This study was supported by a grant from VA Health Services Research and Development (IIR-10-374). Dr. Rose is supported by a career development award from VA Health Services Research and Development (CDA-08-017). The sponsor had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, and approval of the manuscript.
Disclaimer
The opinions expressed in this manuscript do not necessarily represent the official views of the Department of Veterans Affairs.
Guarantor
Dr. Rose is the guarantor of the entire manuscript.
Presentations
No prior presentations.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Efird, L.M., Miller, D.R., Ash, A.S. et al. Identifying the Risks of Anticoagulation in Patients with Substance Abuse. J GEN INTERN MED 28, 1333–1339 (2013). https://doi.org/10.1007/s11606-013-2453-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2453-x