Abstract
BACKGROUND
Clinical guidelines recommend that physicians counsel patients on diet and exercise; however, physician counseling remains suboptimal.
OBJECTIVES
To determine if incorporating performance improvement (PI) methodologies into a needs assessment for an internal medicine (IM) residency curriculum on nutrition and exercise counseling was feasible and enhanced our understanding of the curricular needs.
DESIGN AND PARTICIPANTS
One hundred and fifty-eight IM residents completed a questionnaire to assess their knowledge, attitudes, and practices (KAP) about nutrition and exercise counseling for hypertensive patients. Residents’ baseline nutrition and exercise counseling rates were also obtained using chart abstraction. Fishbone diagrams were created by the residents to delineate perceived barriers to diet and exercise counseling.
MAIN MEASURES
The KAP questionnaire was analyzed using descriptive statistics. Chart abstraction data was plotted on run charts and average counseling rates were calculated. Pareto charts were developed from the fishbone diagrams depicting the number of times each barrier was reported.
KEY RESULTS
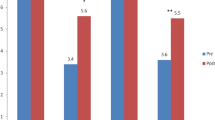
Almost 90% of the residents reported counseling their hypertensive patients about diet and exercise more than 20% of the time on the KAP questionnaire. In contrast, chart abstraction revealed average counseling rates of 3% and 4% for nutrition and exercise, respectively. The KAP questionnaire exposed a clinical knowledge deficit, lack of familiarity with the national guidelines, and low self-efficacy. In contrast, the fishbone analysis highlighted patient apathy, patient co-morbidities, and time pressure as the major perceived barriers.
CONCLUSIONS
We found that incorporating PI methods into a needs assessment for an IM residency curriculum on nutrition and exercise counseling for patients at risk of cardiovascular disease was feasible, provided additional information not obtained through other means, and provided the opportunity to pilot the use of PI techniques as an educational strategy and means of measuring outcomes. Our findings suggest that utilization of PI principles provides a useful framework for developing and implementing a medical education curriculum and measuring its effectiveness.





Similar content being viewed by others
References
Chobanian AV, Bakaris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52.
Pearson TA, Blair SN, Daniels SR, et al. AHA Guidelines for primary prevention of cardiovascular disease and stroke: 2002 Update. Consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation. 2002;106:388–91.
Redberg RF, Benjamin EJ, Bittner V, et al. ACCF/AHA 2009 performance measures for primary prevention of cardiovascular disease in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing committee to develop performance measures for primary prevention of cardiovascular disease). Developed in collaboration with the American Academy of Family Physicians; American Association of Cardiovascular and Pulmonary Rehabilitation; and Preventive Cardiovascular Nurses Association. Endorsed by the American College of Preventive Medicine, American College of Sports Medicine, and Society for Women’s Health Research. J Am Coll Cardiol. 2009;54:1364–405.
Mellen PB, Palla SL, Goff DC Jr, Bonds DE. Prevalence of nutrition and exercise counseling for patients with hypertension. United States, 1999 to 2000. J Gen Intern Med. 2004;19:917–24.
Jacobson TA, Morton F, Jacobson KL, Sharma S, Garcia DC. An assessment of obesity among African-American women in an inner city primary care clinic. J Natl Med Assoc. 2002;94:1049–57.
Tsui JI, Dodson K, Jacobson TA. Cardiovascular disease prevention counseling in residency: resident and attending physician attitudes and practices. J Natl Med Assoc. 2004;96 1080–3, 1088–91.
Kern D, Thomas P, Howard D, Bass E. Curriculum Development for Medical Education. A Six-Step Approach. Maryland: The John Hopkins University Press; 1998.
Langley G, Moen R, Nolan K, Nolan T, Norman C, Provost L. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. New York: Jossey-Bass; 2009.
Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34.
Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45.
ACGME Outcomes Project: General Competencies. Available at: http://www.acgme.org/outcome/comp/compMin.asp. Accessed May 3, 2010.
Levine MA, Grossman RS, Darden PM, et al. Dietary counseling of hypercholesterolemic patients by internal medicine residents. J Gen Intern Med. 1992;7:511–6.
Tang JW, Freed B, Baker T, et al. Internal medicine residents’ comfort with and frequency of providing dietary counseling to diabetic patients. J Gen Intern Med. 2009;24:1140–3.
Rogers LQ, Bailey JE, Gutin B, et al. Teaching resident physicians to provide exercise counseling: a needs assessment. Acad Med. 2002;77:841–4.
Mosca L, Linfante AH, Benjamin EJ, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510.
Rogers LQ, Gutin B, Humphries MC, et al. Evaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived success. Teach Learn Med. 2006;18:215–21.
Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115–21.
Acknowledgements
-
1.
We appreciate and acknowledge the support of an intramural grant for medical education innovations from Emory Healthcare.
-
2.
Prior to writing this manuscript:
-
a.
Drs. Fluker, Whalen, and Doyle presented a poster, “Assessing Residents’ Behaviors and Barriers to Counseling Hypertensive Patients on Diet Using Performance Improvement Tools” at the ACGME-ABMS Joint Conference, Physician Competence: From Deconstruction to Reconstruction, on September 15, 2007.
-
b.
Drs. Whalen and Schneider presented a workshop, “Designing and Implementing Interventions to Improve Exercise Counseling in Continuity Clinics” at the Annual American College of Sports Medicine meeting, May 28–31, 2008.
-
a.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fluker, SA., Whalen, U., Schneider, J. et al. Incorporating Performance Improvement Methods into a Needs Assessment: Experience with a Nutrition and Exercise Curriculum. J GEN INTERN MED 25 (Suppl 4), 627–633 (2010). https://doi.org/10.1007/s11606-010-1404-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1404-z