Abstract
BACKGROUND
Prescription medication labels contain valuable health information, and better labels may enhance patient adherence to chronic medications. A new prescription medication labeling system was implemented by Target pharmacies in May 2005 and aimed to improve readability and understanding.
OBJECTIVE
We evaluated whether the new Target label influenced patient medication adherence.
DESIGN AND PATIENTS
Using claims from two large health plans, we identified patients with one of nine chronic diseases who filled prescriptions at Target pharmacies and a matched sample who filled prescriptions at other community pharmacies.
MEASUREMENTS
We stratified our cohort into new and prevalent medication users and evaluated the impact of the Target label on medication adherence. We used linear regression and segmented linear regression to evaluate the new-user and prevalent-user analyses, respectively.
RESULTS
Our sample included 23,745 Target users and 162,368 matched non-Target pharmacy users. We found no significant change in adherence between new users of medications at Target or other community pharmacies (p = 0.644) after implementing the new label. In prevalent users, we found a 0.0069 percent reduction in level of adherence (95% CI −0.0138-0.0; p < 0.001) and a 0.0007 percent increase in the slope in Target users (the monthly rate of change of adherence) after implementation of the new label (95% CI 0.0001–0.0013; p = 0.001).
CONCLUSIONS
We found no changes in adherence of chronic medication in new users, and small and likely clinically unimportant changes in prevalent users after implementation of the new label. While adherence may not be improved with better labeling, evaluation of the effect of labeling on safety and adverse effects is needed.



Similar content being viewed by others
References
World Health Organization. Adherence to long-term therapies: Evidence for action. Geneva, Switzerland: WHO; 2003. Available at: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf Accessed 1/26/09.
Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):455–61.
Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H, LeLorier J. Persistence of use of lipid-lowering medications: a cross-national study. JAMA. 1998;279(18):1458–62.
Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–41.
National Council on Patient Information and Education. Enhancing prescription medication adherence: a national action plan. Aug. 2007. Available at: http://www.talkaboutrx.org/documents/enhancing_prescription_medicine_adherence.pdf. Accessed 6/2/2008.
Mehta S, Moore RD, Graham NM. Potential factors affecting adherence with HIV therapy. AIDS. 1997;11(14):1665–70.
Isaac LM, Tamblyn RM. Compliance and cognitive function: a methodological approach to measuring unintentional errors in medication compliance in the elderly. McGill-Calgary Drug Research Team. Gerontologist. 1993;33(6):772–81.
Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. Physician communication when prescribing new medications. Arch Intern Med. 2006;166(17):1855–62.
Svarstad BL, Bultman DC, Mount JK. Patient counseling provided in community pharmacies: effects of state regulation, pharmacist age, and busyness. J Am Pharm Assoc (Wash DC). 2004;44(1):22–9.
Fletcher SW, Fletcher RH, Thomas DC, et al. Patients’ understanding of prescribed drugs. J Community Health. 1979;4(3):183–9.
Shrank WH, Avorn J. Educating patients about their medications: the limitations and potential of written drug information. Health Affairs. 2007;26(3):731–40.
Davis TC, Wolf MS, Bass PF 3rd, Thompson JA, Tilson HH, Neuberger M, Parker RM. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145(12):887–94.
Davis TC, Wolf MS, Bass PF 3rd, Middlebrooks M, Kennen E, Baker DW, Bennett CL, Durazo-Arvizu R, Bocchini A, Savory S, Parker RM. Low literacy impairs comprehension of prescription drug warning labels. J Gen Intern Med. 2006;21(8):847–51.
Shrank WH, Agnew-Blais J, Choudhry NK, Wolf MS, Kesselheim A, Avorn J, Shekelle P. The variability and quality of medication container labels. Arch Intern Med. 2007;167(16):1760–5.
Haynes RB, McDonald H, Garg AX. Interventions for helping patients to follow prescriptions for medications. Oxford, England: Cochrane library, Update software; 2002; issue 2.
Shrank W, Avorn J, Rolón C, Shekelle P. The Effect of the Content and Format of Prescription Drug Labels on Readability, Understanding and Medication Use: a Systematic Review. Annals of Pharmacotherapy. 2007;41(5):783–801.
Bull, G. USA Today. April 28, 2005. Available at: http://www.usatoday.com/money/industries/health/drugs/2005-04-28-target-pill_x.htm?csp = 34. Accessed 01/26/09
Samet JH, Libman H, Steger KA, Dhawan RK, Chen J, Shevitz AH, Dewees-Dunk R, Levenson S, Kufe D, Craven DE. Compliance with zidovudine therapy in patients infected with human immunodeficiency virus, type 1: a cross-sectional study in a municipal hospital clinic. Am J Med. 1992;92(5):495–502.
Isaac LM, Tamblyn RM. Compliance and cognitive function: a methodological approach to measuring unintentional errors in medication compliance in the elderly. McGill-Calgary Drug Research Team. Gerontologist. 1993;33(6):772–81.
Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21(12):1215–21.
Halpern MT, Khan ZM, Schmier JK, Burnier M, Caro JJ, Cramer J, Daley WL, Gurwitz J, Hollenberg NK. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension. 2006;47(6):1039–48.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;(42):121–30.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–9.
Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167(6):540–50.
Shrank WH, Asch SM, Adams J, Setodji C, Kerr EA, Keesey J, Malik S, McGlynn EA. The Quality of Pharmacologic Care for Adults in the United States. Medical Care. 2006;44(10):936–45.
Higashi T, Shekelle PG, Solomon DH, Knight EL, Roth C, Chang JT, Kamberg CJ, MacLean CH, Young RT, Adams J, Reuben DB, Avorn J, Wenger NS. The quality of pharmacologic care for vulnerable older patients. Ann Intern Med. 2004;140(9):714–20.
Choudhry NK, Anderson G, Laupacis A, Ross-Degnan D, Normand SL, Soumerai SB. The impact of adverse events on warfarin prescribing in atrial fibrillation: a matched-pair analysis. BMJ. 2006;332:141–5.
Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50(1):105–16.
Acknowledgements
This work was supported by a Pioneer Award from the Robert Wood Johnson Foundation.
Dr. Shrank is supported by a career development award from the National Heart, Lung and Blood Institute (K23HL090505-01). Dr. Brookhart is supported by a career development award from the National Institute of Aging (AG-027400).
Drs. Shrank, Avorn, Choudhry, Schneeweiss, and Brookhart receive research funding from CVS Caremark for studies on medication adherence.
We would like to thank Joy Lee for her administrative and technical help with the project.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Pioneer Award from the Robert Wood Johnson Foundation. Dr. Shrank is supported by a career development award from the National Heart, Lung and Blood Institute (K23HL090505-01). Dr. Brookhart is supported by a career development award from the National Institute of Health (AG-027400).
Appendices
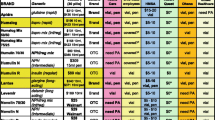
Appendix 1: Medications used to identify patients who might have one of nine chronic diseases
-
(1)
Atrial fibrillation
-
(a)
Warfarin (coumadin)
-
(b)
Beta-blockers: Acebutolol Hydrochloride, Atenolol, Betaxolol Hydrochloride, Bisoprolol Fumarate, Carteolol Hydrochloride, Esmolol Hydrochloride, Metoprolol Succinate, Metoprolol Tartrate, Nadolol, Penbutolol Sulfate, Pindolol, Propranolol Hydrochloride, Sotalol Hydrochloride, Timolol Maleate
-
(c)
Calcium channel blockers, nondihydropyridines: Diltiazem Hydrochloride, Diltiazem Malate, Mibefradil Di-Hydrochloride, Verapamil Hydrochloride
-
(a)
-
(2)
Diabetes
-
(a)
Ace inhibitors: Benazepril Hydrochloride, Captopril, Enalapril Maleate, Enalaprilat, Enalaprilat Dihydrate, Fosinopril Sodium, Lisinopril, Moexipril Hydrochloride, Perindopril Erbumine, Quinapril Hydrochloride, Ramipril, Trandolapril
-
(b)
Angiotensin receptor blocker: Candesartan, Cilexetil, Eprosartan Mesylate, Irbesartan, Losartan Potassium, Olmesartan Medoxomil, Telmisartan, Valsartan
-
(c)
Metformin
-
(d)
Sulfonureas: glipizide, glyburide, gliclazide, glimepiride,
-
(e)
Glitazones: rosiglitazone, pioglitazone
-
(f)
Insulin: insulin aspart, insulin glulisine, insulin lispro, regular, nph, lente, ultrelente, insulin detemir, insulin glargine, insulin mixtures (novolog 70/30, humalog 75/25, humulin 70/30, humulin 50/50, novolin 70/30—these are brand names)
-
(a)
-
(3)
Asthma/COPD
-
(a)
Beta agonists: albuterol, fenoterol, formoterol, fenotorol, levalbuterol, metaproteronol, pirbuterol, salmeterol, terbutaline
-
(b)
Combos: advair, combivent, duoned, symbicort (these are brand names)
-
(c)
Inhaled steroids: beclomethasone, budesonide, flunisolide, fluticasone, mometasone, triamcinolone
-
(d)
Leukotriene inhibitors: montelukast, zafirlukast, zileuton
-
(e)
Others: ipatropium, tiotropium
-
(a)
-
(4)
Hypercholesterolemia/Hyperlipidemia
-
(a)
Statins: atorvastatin, simvastatin, lovastatin, pravastatin, rosuvastatin, fluvastatin, vytorin
-
(b)
Other: niacin, ezetimibe
-
(c)
Bile acid sequestrants: cholestyramine, cholesevelam, colestipol
-
(d)
Fibrates: fenofibrate, gemfibrozil, bezafibrate
-
(a)
-
(5)
CHF (congestive heart failure)
-
(a)
Ace inhibitors: Benazepril Hydrochloride, Captopril, Enalapril Maleate, Enalaprilat, Enalaprilat Dihydrate, Fosinopril Sodium, Lisinopril, Moexipril Hydrochloride, Perindopril Erbumine, Quinapril Hydrochloride, Ramipril, Trandolapril
-
(b)
Loop diuretics: furosemide, bumetanide, torsemide
-
(c)
Angiotensin receptor blocker: Candesartan, Cilexetil, Eprosartan Mesylate, Irbesartan, Losartan Potassium, Olmesartan Medoxomil, Telmisartan, Valsartan
-
(d)
Aldosterone ant.: spironolactone, eplerenone
-
(e)
Beta-blockers: Acebutolol Hydrochloride, Atenolol, Betaxolol Hydrochloride, Bisoprolol Fumarate, Carteolol Hydrochloride, Esmolol Hydrochloride, Metoprolol Succinate, Metoprolol Tartrate, Nadolol, Penbutolol Sulfate, Pindolol, Propranolol Hydrochloride, Sotalol Hydrochloride, Timolol Maleate
-
(f)
Digoxin
-
(a)
-
(6)
Osteoporosis
-
(a)
Bisphosphonates: alendronate, clodronate, etidronate, ibandronate, pamidronate, risedronate, zoledronic acid
-
(a)
-
(7)
Hypertension
-
(a)
ACE Inhibitors: Benazepril Hydrochloride, Captopril, Enalapril Maleate, Enalaprilat, Enalaprilat Dihydrate, Fosinopril Sodium, Lisinopril, Moexipril Hydrochloride, Perindopril Erbumine, Quinapril Hydrochloride, Ramipril, Trandolapril
-
(b)
Thiazide diuretics: Bendroflumethiazide, Benzthiazide, Chlorothiazide, Chlorothiazide Sodium, Chlorthalidone, Cyclothiazide, Hydrochlorothiazide, Hydroflumethiazide, Indapamide, Methyclothiazide, Metolazone, Polythiazide, Quinethazone, Trichlormethiazide
-
(c)
Angiotensin receptor blocker: Candesartan, Cilexetil, Eprosartan Mesylate, Irbesartan, Losartan Potassium, Olmesartan Medoxomil, Telmisartan, Valsartan
-
(d)
Beta-blockers: Acebutolol Hydrochloride, Atenolol, Betaxolol Hydrochloride, Bisoprolol Fumarate, Carteolol Hydrochloride, Esmolol Hydrochloride, Metoprolol Succinate, Metoprolol Tartrate, Nadolol, Penbutolol Sulfate, Pindolol, Propranolol Hydrochloride, Sotalol Hydrochloride, Timolol Maleate
-
(e)
Calcium channel blockers:
-
Nondihydropyridines: Diltiazem Hydrochloride, Diltiazem Malate, Mibefradil Di-Hydrochloride, Verapamil Hydrochloride
-
Dihydropyridines: Amlodipine Besylate, Bepridil Hydrochloride, Felodipine, Isradipine, Nicardipine Hydrochloride, Nifedipine, Nimodipine, Nisoldipine
-
-
(f)
Potassium-Sparing Agents: Amiloride Hydrochloride, Spironolactone, Triamterene
-
(g)
Central Alpha-Antagonists: Clonidine Hydrochloride, Guanabenz Acetate, Guanfacine Hydrochloride, Methyldopa, Methyldopate Hydrochloride, Phenoxybenzamine Hydrochloride, Phentolamine Hydrochloride, Tolazoline Hydrochloride
-
(h)
Alpha Blockers: Doxazosin Mesylate, Prazosin Hydrochloride, Terazosin Hydrochloride
-
(i)
Combination Drugs
-
Beta Blockers And Diuretics
-
Bendroflumethiazide/Nadolol
-
Chlorthalidone/Atenolol
-
Hydrochlorothiazide/Bisoprolol Fumarate
-
Hydrochlorothiazide/Labetalol Hydrochloride
-
Hydrochlorothiazide/Metoprolol Tartrate
-
Hydrochlorothiazide/Propranolol
-
Hydrochlorothiazide/Propranolol Hydrochloride
-
Hydrochlorothiazide/Timolol
-
-
ACE Inhibitors And Diuretics
-
Benazepril Hydrochloride/Hydrochlorothiazide
-
Captopril/Hydrochlorothiazide
-
Enalapril Maleate/Hydrochlorothiazide
-
Fosinopril Sodium/Hydrochlorothiazide
-
Lisinopril/Hydrochlorothiazide
-
Moexipril Hydrochloride/Hydrochlorothiazide
-
Quinapril Hydrochloride/Hydrochlorothiazide
-
-
Angiotensin II Receptor Antagonists And Diuretics
-
Candesartan Cilexetil/Hydrochlorothiazide
-
Irbesartan/Hydrochlorothiazide
-
Losartan Potassium/Hydrochlorothiazide
-
Telmisartan/Hydrochlorothiazide
-
Valsartan/Hydrochlorothiazide
-
-
Calcium Antagonists And ACE Inhibitors
-
Benazepril Hydrochloride/Amlodipine Besylate
-
Enalapril Maleate/Diltazem Maleate
-
Enalapril Maleate/Felodipine
-
Trandolapril/Verapamil Hydrochloride
-
-
Other Combinations
-
Bendroflumethiazide/Potassium Chloride
-
Cryptenamine/Methylclothiazide
-
Hydrochlorothiazide/Spironolactone
-
Spironolactone/Hydrochlorothiazide
-
Hydrochlorothiazide/Triamterene
-
Hydrochlorothiazide/Amiloride Hydrochloride
-
Clonidine Hydrochloride/Chlorthalidone
-
Deserpidine/Hydrochlorothiazide
-
Deserpidine/Methyclothiazide
-
Guanethidine Sulfate/Hydrochlorothiazide
-
Methyldopa/Chlorothiazide
-
Methyldopa/Hydrochlorothiazide
-
Reserpine/Benzthiazide
-
Reserpine/Chlorothiazide
-
Reserpine/Chlorthalidone
-
Reserpine/Hydrochlorothiazide
-
Reserpine/Hydroflumethiazide
-
Reserpine/Methyclothiazide
-
Reserpine/Polythiazide
-
Reserpine/Quinethazone
-
Reserpine/Trichlormethiazide
-
Hydralazine Hydrochloride/Hydrochlorothiazide
-
Hydralazine Hydrochloride/Reserpine
-
Hydralazine Hydrochloride/Reserpine/Hydrochlorothiazide
-
Hydralaz/Reserpine/Hydrochlorothiazide
-
Hydralazine Hydrochloride/Hydrochlorothiazide
-
Prazosin Hydrochloride/Polythiazide
-
Methylclothiazide/Pargyline
-
Rauwolfia Serpentina/Bendroflumethiazide
-
Rauwolfia/Bendroflumethiazide/Potassium
-
-
Miscellaneous
-
Diazoxide
-
Metyrosine
-
Reserpine/Mannitol Hexanitrate
-
Acetazolamide
-
-
-
(a)
-
(8)
Depression
-
a)
SSRIs: citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline
-
b)
Others: buproprion, duloxetine, mirtazapine, venlafaxine
-
a)
-
(9)
Coronary Artery Disease
-
(a)
Ace inhibitors: Benazepril Hydrochloride, Captopril, Enalapril Maleate, Enalaprilat, Enalaprilat Dihydrate, Fosinopril Sodium, Lisinopril, Moexipril Hydrochloride, Perindopril Erbumine, Quinapril Hydrochloride, Ramipril, Trandolapril
-
(b)
Angiotensin receptor blocker: Candesartan, Cilexetil, Eprosartan Mesylate, Irbesartan, Losartan Potassium, Olmesartan Medoxomil, Telmisartan, Valsartan
-
c)
Beta-blockers: Acebutolol Hydrochloride, Atenolol, Betaxolol Hydrochloride, Bisoprolol Fumarate, Carteolol Hydrochloride, Esmolol Hydrochloride, Metoprolol Succinate, Metoprolol Tartrate, Nadolol, Penbutolol Sulfate, Pindolol, Propranolol Hydrochloride, Sotalol Hydrochloride, Timolol Maleate
-
d)
statins: atorvastatin, simvastatin, lovastatin, pravastatin, rosuvastatin, fluvastatin, vytorin
-
e)
anti-platelets: clopidogrel, aspirin, coumadin
-
(a)
Appendix 2: ICD-9 Diagnostic codes used to identify chronic diseases
-
(1)
Atrial Fibrillation (ICD-9 codes: 427.31)
-
(2)
Diabetes (ICD-9 codes: 250.0x–250.9x)
-
(3)
Asthma/COPD (ICD-9 codes: 494.xx, 496.xx)
-
(4)
Hypercholesterolemia/Hyperlipidemia (ICD-9 codes: 272.0, 272.2)
-
(5)
CHF (congestive heart failure) (ICD-9 codes: 428.xx)
-
(6)
Osteoporosis (ICD-9 codes: 733.0)
-
(7)
Hypertension (ICD-9 codes: 401.xx, 402.xx, 403.xx, 404.xx, 405.xx)
-
(8)
Depression (ICD-9 codes: 296.2x, 296.3x, 300.4x, 309.0x, 309.1x, or 311.xx)
-
(9)
Coronary Artery Disease (ICD-9 codes: 414.0x)
Rights and permissions
About this article
Cite this article
Shrank, W.H., Gleason, P.P., Canning, C. et al. Can Improved Prescription Medication Labeling Influence Adherence to Chronic Medications? An Evaluation of the Target Pharmacy Label. J GEN INTERN MED 24, 570–578 (2009). https://doi.org/10.1007/s11606-009-0924-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-0924-x