Abstract
Background
Thanks to technical advancement in surgery for hepatocellular carcinoma (HCC), hepatic resection (HR) for elderly HCC patients has become safer. However, elderly patients may have shorter long-term survival after surgery if compared with younger patients because of their expected life span. The aim of the present study was to evaluate clinical outcomes and safety after HR in HCC patients aged >75 years (older) compared with HCC patients aged <75 years (younger).
Method
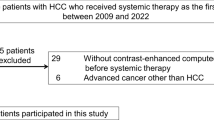
One hundred sixty-eight patients who underwent HR for HCC from 1998 to 2015 in our Center were analyzed using a prospective database. Complications, disease-free survival rates, and cumulative survival rates were compared between the two groups.
Results
During the immediate postoperative period, no differences were found about liver-related complications, hospital stay and 90-day mortality. However, older patients had more complications in class II or higher (Clavien classification) (p = 0.017). Although disease-free survival in both groups was similar (p = 0.099), overall survival was worse in the elderly group (p = 0.024). On multivariate analysis, only age ≥75 years was significantly related to overall survival.
Conclusion
If elderly patients with liver cirrhosis and HCC are appropriately selected and evaluated, they might have favorable prognoses after HR.


Similar content being viewed by others
References
El-Serag HB, Kramer J, Duan Z, Kanwal F. Epidemiology and outcomes of hepatitis C infection in elderly US Veterans. J Viral Hepat 2016; 23:687–96
Borzio M, Dionigi E, Parisi GC, Raguzzi I, Sacco R. Management of hepatocellular carcinoma in the elderly. World J Hepatol 2015; 7: 1521–29
Spolverato G, Vitale A, Ejaz A, et al. The relative net health benefit of liver resection, ablation, and transplantation for early hepatocellular carcinoma. World J Surg 2015; 39: 1474–84
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693– 699.
Clinical Practice Guidelines for Hepatocellular Carcinoma—The Japan Society of Hepatology 2009 update. Hepatol Res 2010; 40 Suppl 1: 2–144
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012; 379: 1245–55
Donadon M, Procopio F, Torzilli G. Tailoring the area of heaptic resection using inflow and outflow modulation World J Gastroenterol 2013; 19: 1049–55
Cucchetti A, Sposito C, Pinna AD et al. Effect of age on survival in patients undergoing resection of hepatocellular carcinoma. BJS 2016; 103: e93-e99
Kinoshita A, Koike K, Nishino H Clinical features and prognosis of elderly patients with hepatocellular carcinoma not indicated for surgical resection. Geriatr Gerontol Int 2016 Feb 5. doi: 10.1111/ggi.12747. [Epub ahead of print]
Santambrogio R, Bianchi P, Pasta A, Palmisano A, Montorsi M. (2002) Ultrasound-guided interventional procedures of the liver during laparoscopy: technical considerations. Surg Endosc 16:349–354
Bruix J and Sherman M. Management of hepatocellular carcinoma: an update. Hepatology 2011; 53: 1020–22
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol 2001; 35: 421–30
Santambrogio R, Kluger MD, Costa M et al. Hepatic resection for hepatocellular carcinoma in patients with Child-Pugh’s A cirrhosis: is clinical evidence of portal hypertension a contraindication? HPB 2013; 15: 78–84
Pugh RNH, Murray-Lyon M, Dawson JL, Pietroni MC, Williams R. Transection of the esophagus for bleeding esophageal varices. Br J Surg 1973; 60: 646–649
Marrero JA, Fontana RJ, Barrat A, Askari F, Conjeevaram HS, Su GL et al. Prognosis of hepatocellular carcinoma: Comparison of seven staging systems in an American cohort. Hepatology 2005; 41:707–716
Simons JP, Chau S, Hill JS, et al. In-hospital mortality from liver resection for hepatocellular carcinoma. Cancer 2010; 116: 1733–8
Yamashita Y, Tsuijita E, Takeishi K, Fujiwara M, Kira S, Mori M, Aishima S, Taketomi A, Shirabe K, Ishida T, Maehara Y (2012) Predictors for microinvasion of small hepatocellular carcinoma ≤2 cm. Ann Surg Oncol 19: 2027–34
Santambrogio R, Costa M, Strada D, et al. Intraoperative ultrasound score to predict recurrent hepatocellular carcinoma after radical treatments. Ultrasound Med Biol 2011; 37: 7–15
Santambrogio R, Bruno S, Kluger MD et al. Laparoscopic ablation therapies or hepatic resection in cirrhotic patients with small hepatocellular carcinoma. Dig Liver Dis 2016; 48: 189–196
Santambrogio R, Aldrighetti L, Barabino M, Pulitanò C, Costa M, Montorsi M et al. Laparoscopic liver resections for hepatocellular carcinoma. Is it a feasible option for patients with liver cirrhosis? Langenbecks Arch Surg 2009; 394: 255–64
Cherqui D, Laurent A, Tayar A, Chang S, Van Nhieu JT, Lotiau J et al. Laparoscopic Liver Resection for Peripheral Hepatocellular Carcinoma in Patients With Chronic Liver Disease Midterm Results and Perspectives. Ann Surg 2006; 243: 499–506
Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 1954; 7:462–503.
Wayne JD, Lauwers GY, Ikai I, Doherty DA, Belghiti J, Yamaoka Y et al. Preoperative predictors of survival after resection of small hepatocellular carcinomas. Ann Surg 2002; 5: 722–31
Dindo D, Demartines N, Clavien PA. Classification of surgical complications. A new proposal with evaluation in a cohort of 633 patients and results of a survey. Ann Surg 2004; 240: 205–13
Rahbari NN, Garden J, Padbury R et al. Posthepatectomy liver failure: a definition and grading by the international Study Group of Liver Surgery (ISGLS). Surgery 2011; 149: 713–24
Ide T, Miyoshi A, Kitahara K, Noshiro H. Prediction of postoperative complications in elderly patients with hepatocellular carcinoma. J Surg Res 2013; 185: 614–619
Nishikawa H, Kimura T, Kita R, Osaki Y. Treatment for hepatocellular carcinoma in elderly patients: a literature review. J Cancer 2013; 4: 635–43
Molinari M, Helton S. Hepatic resection versus radiofrequency ablation for hepatocellular carcinoma in cirrhotic individuals not candidates for liver transplantation: a Markov model decision analysis. Am J Surg 2009; 198: 396–406
Yazici P, Akyuz M, Yigitbas H et al. A comparison of perioperative outcomes in elderly patients with malignant liver tumors undergoing laparoscopic liver resection versus radiofrequency ablation. Surg Endosc 2016; July 21 DOI: 10.1007/s00464-016-5105-5 [Epub ahead of print]
Kishida N, Hibi T, Itano O, et al. Validation of hepatectomy for elderly patients with hepatocellular carcinoma. Ann Surg Oncol 2015; 22: 3094–3101
Andert A, Lodewick T, Ulmer TF et al. Liver resection in the elderly: a retrospective cohort study of 460 patients—Feasible and safe. Int J Surg 2016; 28:126–130
Chan ACY, Poon RTP, Cheung TT, et al. Laparoscopic versus open liver resection for elderly patients with malignant liver tumors: a single-center experience. J Gastroenterol Hepatol 2014; 29: 1279–83
Shi B, Zhang K, Zhang J, Chen J, Zhang N, Xu Z. Relationship between patient age and superficial transitional cell carcinoma characteristics. Urology. 2008; 71:1186–90
Ito Y, Kudo T, Takamura Y, Kobayashi K, Miya A, Miyauchi A. Prognostic factors of papillary thyroid carcinoma vary according to sex and patient age. World J Surg. 2011; 35:2684–90.
Goldvaser H, Purim O, Kundel Y, et al. Colorectal cancer in young patients: is it a distinct clinical entity? Int J Clin Oncol. 2016; 21:684–95.
Smith BR, Stabile BE. Extreme aggressiveness and lethality of gastric adenocarcinoma in the very young. Arch Surg. 2009;144:506–10
Partridge AH, Hughes ME, Warner ET et al. Subtype-Dependent Relationship Between Young Age at Diagnosis and Breast Cancer Survival. J Clin Oncol. 2016; 34:3308–14
Oishi K, Itamoto T, Konayashi T. Hepatectomy for hepatocellular carcinoma in elderly patients aged 75 years or more. J Gastrointest Surg 2009; 13: 695–701
Nishikawa H, Arimoto A, Wakasa T, Kita R, Kimura T, Osaka Y. Surgical resection for hepatocellular carcinoma: clinical outcomes and safety in elderly patients. Eur J Gastroenterol Hepatol 2013; 25: 912–19
Taniai N, Yoshida H, Yoshioka M, Kawano Y, Uchida E. Surgical outcomes and prognostic factors in elderly patients (75 years or older) with hepatocellular carcinoma who underwent hepatectomy. J Nippon Med Sch 2013; 80: 426–32
Liu P-H, Hsu C-Y, Lee Y-H et al. Uncompromised treatment efficacy in elderly patients with hepatocellular carcinoma: a propensity score analysis. Medicine 2014; 93; e264
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roberto Santambrogio, Matteo Barabino, Giovanna Scifo, Mara Costa, Marco Giovenzana, and Enrico Opocher have no conflicts of interest or financial ties to disclose and all authors must meet all of the criteria according the guidelines of the International Committee of Medical Journal Editors (ICMJE).
Rights and permissions
About this article
Cite this article
Santambrogio, R., Barabino, M., Scifo, G. et al. Effect of Age (over 75 Years) on Postoperative Complications and Survival in Patients Undergoing Hepatic Resection for Hepatocellular Carcinoma. J Gastrointest Surg 21, 657–665 (2017). https://doi.org/10.1007/s11605-016-3354-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3354-1