Abstract
Background
The optimal management of small (≤2 cm) pancreatic neuroendocrine tumors (PNETs) remains controversial. We evaluated these tumors in the National Cancer Data Base (NCDB) to determine if resection provides a survival advantage over observation.
Methods
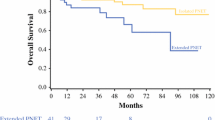
The NCDB was queried to identify patients with nonmetastatic PNETs ≤2 cm treated between 1998 and 2006. Kaplan-Meier survival estimates, stratified by grade and treatment type, evaluated the difference in 5-year overall survival (OS) between patients who underwent resection and observation. Multivariable Cox regression was used to determine the importance of resection in OS.
Results
Three hundred eighty patients met inclusion criteria. Eighty-one percent underwent resection; 19 % were observed. Five-year OS was 82.2 % for patients who underwent surgery and 34.3 % for those who were observed (p < 0.0001). When controlling for age, comorbidities, income, facility type, tumor size and location, grade, margin status, nodal status, surgical management, and nonsurgical therapy in the Cox model, observation [hazard ratio (HR) 2.80], poorly differentiated histology (HR 3.79), lymph node positivity (HR 2.01), and nonsurgical therapies (HR 2.23) were independently associated with an increase in risk of mortality (p < 0.01).
Conclusion
Patients with localized PNETs ≤2 cm had an overall survival advantage with resection compared to observation, independent of age, comorbidities, tumor grade, and treatment with nonsurgical therapies.


Similar content being viewed by others
References
Bettini R, Partelli S, Boninsegna L, Capelli P, Crippa S, Pederzoli P, Scarpa A, Falconi M. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery 2011;150:75–82.
Franko J, Feng W, Yip L, Genovese E, Moser AJ. Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. Journal of Gastrointestinal Surgery 2010;14:541–548.
Cherenfant J, Stocker SJ, Gage MK, Du H, Thurow TA, Odeleye M, Schimpke SW, Kaul KL, Hall CR, Lamzabi I, Gattuso P, Winchester DJ, Marsh RW, Roggin KK, Bentrem DJ, Baker MS, Prinz RA, Talamonti MS. Predicting aggressive behavior in nonfunctioning pancreatic neuroendocrine tumors. Surgery 2013;154:785–791.
Bilimoria KY, Talamonti MS, Tomlinson JS, Stewart AK, Winchester DP, Ko CY, Bentrem DJ. Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: Analysis of 3851 patients. Annals of Surgery 2008;247:490–500.
Haynes AB, Deshpande V, Ingkakul T, Vagefi PA, Szymonifka J, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, Fernandez-del Castillo C. Implications of incidentally discovered, nonfunctioning pancreatic endocrine tumors: Short-term and long-term patient outcomes. Archives of Surgery 2011;146:534–538.
Lee LC, Grant CS, Salomao DR, Fletcher JG, Takahashi N, Fidler JL, Levy MJ, Huebner M. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): Role for nonoperative management. Surgery 2012;152:965–974.
Gaujoux S, Partelli S, Maire F, D’Onofrio M, Larroque B, Tamburrino D, Sauvanet A, Falconi M, Ruszniewski P. Observational study of natural history of small sporadic nonfunctioning pancreatic neuroendocrine tumors. Journal of Clinical Endocrinology and Metabolism 2013;98:4784–4789.
Kooby DA, Gillespie TW, Liu Y, Byrd-Sellers J, Landry J, Bian J, Lipscomb J. Impact of adjuvant radiotherapy on survival after pancreatic cancer resection: An appraisal of data from the National Cancer Data Base. Annals of Surgical Oncology 2013;20:3634–3642.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Nabil Wasif (Scottsdale, AZ): Management of incidentally found small pancreatic neuroendocrine tumors can be clinically quite vexing, and I commend the authors for carrying out this study. The difficulty of studying this “orphan” tumor is highlighted by the fact that even in the largest cancer registry in the world, only 380 patients met inclusion criteria. I have the following questions and comments.
1. The difference in overall survival between patients undergoing surgery versus observation (82 and 34 %) is so stark that I cannot shake the possibility of selection bias explaining your findings. Patients who are judged unfit for surgery are observed and, hence, may be dying of the comorbid diseases that precluded surgical resection in the first place, and not from the neuroendocrine tumor under observation. Are you satisfied with the risk adjustment methodology, i.e., Charlson score and age, used for this study?
2. As a corollary to the first question why did you choose to use overall survival and not disease-specific survival as an endpoint? Do you agree that disease-specific survival would be a more appropriate endpoint in order to account for competing risks from comorbidity?
3. You examine the interaction between surgery and tumor grade in your manuscript. In your experience, how often do patients with a classic PNET on imaging undergo FNA? If they do, how accurate is the assessment of tumor grade based on cytology and can that be reliably used to inform decision making?
Closing Discussant
Dr. Sharpe: Thank you for your comments and questions. I agree that the overall survival difference between patients who undergo resection and those who are observed is quite impressive. There is no doubt that there is selection bias in the database. The cases within the NCDB are all malignant tumors and likely represent the more aggressive versions of pancreatic neuroendocrine tumors being seen nationally each year. There may also be reporting bias. Patients who are observed may not necessarily get captured in the NCDB. We did attempt to ensure that the survival advantage observed was related to treatment type as best as possible within the limits of the database by controlling for age and Charlson score in our multivariate model. Moreover, this is the largest series specifically addressing the effect of resection on overall survival in PNETs 2 cm or less and demonstrates a survival benefit with resection that is quite large. Given the magnitude of this difference, it would be hard to imagine that the whole difference is due to some omitted variable(s). Certainly, surgical resection has associated morbidity, but I think we should carefully consider future recommendations for observation in patients with tumors between 1 and 2 cm.
I do agree that disease-specific survival would be a more appropriate endpoint than overall survival to account for comorbidities, but at this time, the National Cancer Data Base reports only overall survival and not disease-specific survival.
In our experience, almost all patients with a classic PNET on imaging undergo FNA and many are referred to us having already had the procedure. Several papers have looked at EUS-FNA sensitivity and specificity for tumor diagnosis and in assessment of grade. For tumor diagnosis, the sensitivity and specificity is 80–95 %; for assessment of grade, it is 80 % sensitive and 100 % specific. In our institution, the EUS-FNA is about 80 % sensitive, so I think with a skilled endosonographer and cytopathologist, EUS-FNA is highly accurate. Data for the accuracy of EUS-FNA in the NCDB are not available and could not be determined for this current review.
This study was presented at the Society for Surgery of the Alimentary Tract, May 2–6, 2014, Chicago, IL, USA.
Rights and permissions
About this article
Cite this article
Sharpe, S.M., In, H., Winchester, D.J. et al. Surgical Resection Provides an Overall Survival Benefit for Patients with Small Pancreatic Neuroendocrine Tumors. J Gastrointest Surg 19, 117–123 (2015). https://doi.org/10.1007/s11605-014-2615-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2615-0