Abstract
Purpose
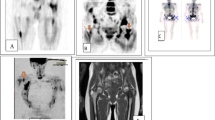
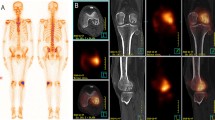
This study was done to determine the diagnostic value of whole-body magnetic resonance using diffusion-weighted imaging with background suppression (WB-DWIBS) for detecting bone metastases compared with whole-body bone scintigraphy (WB-BS).
Materials and methods
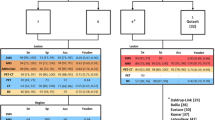
Twenty-three patients with solid tumours underwent both WB-DWIBS imaging and WBBS. A nuclear medicine specialist interpreted WB-BS images and two blinded radiologists, first independently and then jointly, interpreted the WB-DWIBS images by completing a reading grid categorising the skeletal segments. Cohen’s k statistic was used to determine interobserver agreement in reading the WB-DWIBS images and the agreement between WB-BS and WB-DWIBS. Sensitivity and specificity were calculated per patient and per lesion.
Results
Interobserver agreement in reading the WBDWIBS images was substantial or good, with κ=0.68. Analysis of agreement between the nuclear physician’s and the radiologists’ readings provided κ=0.87 [95% confidence interval (CI)=0.76–0.98)] Per-lesion analysis gave a sensitivity of 80% (95% CI=75–85) and a specificity of 98.2% (95% CI=96.5–99.8).
Conclusions
We found a good level of interobserver agreement for the WB-DWIBS images and an excellent level of agreement in the subjective judgement of presence or absence of disease between WB-BS and WB-DWIBS after consensual double reading. WB-DWIBS has the same specificity as WB-BS in detecting bone metastases. The anatomical sites exhibiting the highest level of disagreement between WB-DWIBS and WB-BS are the pelvis, the coccyx, and the sternum, all sites at which detection with WB-BS has the greatest limitations.
Riassunto
Obiettivo
Scopo del presente lavoro è stato confrontare il valore diagnostico della risonanza magnetica (RM) whole body con tecnica diffusion weighted imaging with background body signal suppression (WB-DWIBS), nella identificazione delle metastasi ossee rispetto alla scintigrafia ossea total-body (SOTB), metodica di riferimento.
Materiali e metodi
Ventitré pazienti affetti da patologia tumorale solida sono stati sottoposti sia a esame WBDWIBS che SOTB. Un medico nucleare ha interpretato le immagini della SOTB e due medici radiologi prima individualmente rispettivamente in cieco e poi esprimendo un parere congiunto hanno letto e interpretato le immagini di WB-DWIBS, compilando una scheda di lettura predefinita con una categorizzazione dei segmenti scheletrici. è stata calcolata la concordanza interosservatore per la lettura delle immagini WB-DWIBS e anche la concordanza tra le due tecniche (WB-DWIBS e SOTB) con il test k di Cohen. è stata calcolata la sensibilità e la specificità della metodica sia per paziente, che per lesione.
Risultati
La concordanza inter-osservatore nella lettura delle immagini WB-DWIBS è risultata sostanziale o buona con k=0,68. L’analisi dell’accordo tra la lettura del medico nucleare e del radiologo, calcolata mediante il k statistico di Cohen, ha fornito un valore di k=0,87 [95% intervallo di confidenza (CI)=0,76–0,98]. Nell’analisi per lesione il calcolo della sensibilità ha fornito un valore dell’80% (95% CI=75%–85%) e un valore di specificità pari al 98,2% (95% CI=96,5%-99,8%).
Conclusioni
Dall’analisi dei risultati si osservano una buona corrispondenza delle letture radiologiche della WB-DWIBS e un ottimo accordo nel giudizio soggettivo di presenza o assenza di lesioni tra la SOTB e la WB-DWIBS effettuata in doppia lettura in consensus. La WB-DWIBS mostra una specificità pari a quella della SOTB nella identificazione delle localizzazioni ossee di malattia. Le sedi anatomiche di maggiore discordanza tra DWIBS e SOTB sono rappresentate dal bacino, coccige e sterno, sedi nelle quali la SOTB trova i suoi principali limiti di detezione
Similar content being viewed by others
References/Bibliografia
Balliu E, Boada M, Peláez I et al (2010) Comparative study of wholebody MRI and bone scintigraphy for the detection of bone metastases. Clin Radiol 65:989–996
Keenan WF Jr, Fedullo LM, Robb ME, Plotkin GR (1992) The bone scan in primary care: diagnostic pitfalls. J Am Board Fam Pract 5:63–67
Wüppenhorst N, Maier C, Frettlöh J at al (2010) Sensitivity and specificity of 3-phase bone scintigraphy in the diagnosis of complex regional pain syndrome of the upper extremity. Clin J Pain 3:182–189
Cascini G, Falcone F, Greco C et al (2008) Whole-body magnetic resonance imaging for detecting bone metastases: comparison with bone scintigraphy. Radiol Med 113:1157–1170
Thomas C, Kwee TC, Takahara T et al (2008) Diffusion weighted whole-body imaging with background body signal suppression (DWIBS): features and potential applications in oncology. Eur Radiol 18:1937–1952
Nakanishi K, Kobayashi M, Takahoshi S et al (2005) Whole body MRI for detecting metastatic bone tumor: comparison with bone scintigrams. Magn Reson Med Sci 4(1):11–17
Lauenstein TC, Goehde SC, Herborn CU et al (2004) Whole-body MR imaging: evaluation of patients for metastases. Radiology 233:139–148
Cohen J (1968) Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 70:213–220
Nakanishi K, Kobayashi M, Nakaguchi K et al (2007) Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images Magn Reson Med Sci 6:147–155
Wu LM, Gu HY, Zheng J at al (2011) Diagnostic value of whole-body magnetic resonance imaging for bone metastases: a systematic review and meta-analysis. J Magn Reson Imaging 34:128–135
Barceló J, Vilanova JC, Riera E et al (2007) Diffusion-weighted wholebody MRI (virtual PET) in screening for osseous metastases. Radiology 49:407–415
Takenaka D, Ohno Y, Matsumoto K et al (2009) Detection of bone metastases in non-small cell lung cancer patients: comparison of whole-body diffusion-weighted imaging (DWI), whole-body MR imaging without and with DWI. Whole-body FDG-PET/CT, and bone scintigraphy. J Magn Reson Imaging 30:298–308
Stecco A, Romano G, Negru M at al (2009) Whole-body diffusion-weighted magnetic resonance imaging in staging of oncological patients: comparison with positron emission tomography computed tomography (PET-CT) in a pilot study. Radiol Med 114:1–17
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stecco, A., Lombardi, M., Leva, L. et al. Diagnostic accuracy and agreement between whole-body diffusion MRI and bone scintigraphy in detecting bone metastases. Radiol med 118, 465–475 (2013). https://doi.org/10.1007/s11547-012-0870-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-012-0870-2