Abstract
Background
The relationship between obstructive sleep apnea (OSA) and the risk of nocturia remains unclear. Therefore, we sought to identify whether or not OSA affects the incidence of nocturia.
Methods
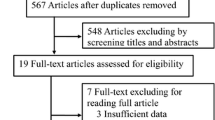
A thorough literature search was executed in September 1st 2018 from PubMed, Web of Science database, and Embase. We used DerSimonian and Laird random-effects to calculate the pooled relative ratio (RR).
Results
Total of 13 studies met inclusion criteria and in total comprised, 406 patients and 9518 controls. There was a significant association between OSA and the risk of nocturia (RR = 1.41, 95% CI 1.26–1.59). Through subgroup analysis by different severity of OSA, we found patients who had severe OSA were at high risk of nocturia. Through another subgroup analysis, we found a statistically significant association between OSA and risk of nocturia in the men (RR = 1.487, 95% CI 1.087–2.034, P = 0.013). However, there was no significant relationship between OSA and nocturia in the women (RR = 1.537, 95% CI 0.831–2.842, P > 0.05). Subgroup analysis of different diagnostic methods indicated that OSA was significantly associated with the risk of nocturia regardless what method was used to diagnose OSA (P < 0.05).
Conclusion
The findings suggest that men with OSA have a high incidence of nocturia. A large multicenter study may be useful to explore the relationship between OSA and nocturia, in order to elucidate its causes.





Similar content being viewed by others
References
Peppard PE et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014
St-Onge MP, Grandner MA, Brown D et al (2016) Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association[J]. Circulation:CIR.0000000000000444
.Redline S . Screening for obstructive sleep apnea: implications for the sleep health of the population[J]. Jama, 2017, 317(4):368, 370
Budhiraja R, Budhiraja P, Quan SF (2010) Sleep-disordered breathing and cardiovascular disorders[J]. Respir Care 55(10):1322–1332 discussion 1330-2
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O'Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study[J]. PLoS Med 6(8):e1000132
Aurora RN, Punjabi NM (2013) Obstructive sleep apnoea and type 2 diabetes mellitus: a bidirectional association[J]. Lancet Respir Med 1(4):329–338
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O'Connor GT, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM (2010) Obstructive sleep apnea-hypopnea and incident stroke the sleep heart health study[J]. Am J Respir Crit Care Med 182(2):269–277
Kramer NR, Bonitati AE, Millman RP (1998) Enuresis and obstructive sleep apnea in adults[J]. Chest 114(2):634–637
Ayik S, Bal K, Akhan G (2014) The association of nocturia with sleep disorders and metabolic and chronic pulmonary conditions: data derived from the polysomnographic evaluations of 730 patients. Turkish J Med Sci 44:249–254
Kaynak H, Kaynak D, Oztura I (2004) Does frequency of nocturnal urination reflect the severity of sleep-disordered breathing? J Sleep Res 13(2):173–176
Wang T, Huang W, Zong H, Zhang Y (2015) The efficacy of continuous positive airway pressure therapy on nocturia in patients with obstructive sleep apnea: a systematic review and meta-analysis. Int Neurourol J 19(3):178–184
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Bax L, Ikeda N, Fukui N, Yaju Y, Tsuruta H, Moons KG (2008) More than numbers: the power of graphs in meta-analysis. Am J Epidemiol 169(2):249–255
Dersimonian R, Nan L (1986) Meta-analysis in clinical trials ☆. Control Clin Trials
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309
Stuck AE, Rubenstein LZ, Wieland D, Egger M, Davey Smith G, Schneider M et al (1998) Bias in meta-analysis detected by a simple, graphical test. 316
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Bing MH et al Obstructive sleep apnea in a Danish population of men and women aged 60-80 years with nocturia. J Clin Sleep Med
Kang S et al (2012) The impact of sleep apnoea syndrome on nocturia according to age in men. BJU Int 110(11c):E851–E856
Zebede S, Lovatsis D, Alarab M, Drutz H (2015) Prevalence of obstructive sleep apnea detected by the Berlin Questionnaire in patients with nocturia attending a urogynecology unit. Int Urogynecol J 26(6):881–885
Martin SA, Appleton SL, Adams RJ, Taylor AW, Catcheside PG, Vakulin A, McEvoy R, Antic NA, Wittert GA (2016) Nocturia, other lower urinary tract symptoms (LUTS) and sleep dysfunction in a community-dwelling cohort of men. Urology 97:219–226
Lowenstein L et al (2008) The relationship between obstructive sleep apnea, nocturia, and daytime overactive bladder syndrome in women. Am J Obstet Gynecol 198(5):598.e1–598.e5
Chung S, Hung SH, Lin HC, Tsai MC, Kao LT (2016) Obstructive sleep apnea and urological comorbidities in males: a population-based study. Sleep Breathing 20(4):1203–1208
Adams RJ, Appleton SL, Vakulin A, Lang C, Martin SA, Taylor AW, McEvoy R, Antic NA, Catcheside PG, Wittert GA (2016) Association of daytime sleepiness with obstructive sleep apnoea and comorbidities varies by sleepiness definition in a population cohort of men. Respirology 21(7):1314–1321
Yoshimura K, Oka Y, Kamoto T, Yoshimura K, Ogawa O (2010) Differences and associations between nocturnal voiding/nocturia and sleep disorders. BJU Int 106(2):232–237
Chen C, Hsu CC, Pei YC, Yu CC, Chen YS, Chen CL (2011) Nocturia is an independent predictor of severe obstructive sleep apnea in patients with ischemic stroke. J Neurol 258(2):189–194
Tuncer M, Yazici O, Kafkasli A, Sabuncu K, Salepci B, Narter F, Gungor GA, Yucetas U (2017) Critical evaluation of the overactive bladder and urgency urinary incontinence association with obstructive sleep apnea syndrome in a relatively young adult male population. Neurourol Urodyn 36(7):1804–1808
Miyazaki T, Kojima S, Yamamuro M, Sakamoto K, Izumiya Y, Tsujita K, Yamamoto E, Tanaka T, Kaikita K, Hokimoto S, Ogawa H (2015) Nocturia in patients with sleep-disordered breathing and cardiovascular disease. Circ J 79(12):2632–2640
Rai A, Nimeh T, Sood A, Thirumavalavan N, Thurmond PE, Azadzoi KM, Lerner LB (2015) Could nocturia be an indicator of an undiagnosed sleep disorder in male veterans? Urology 85(3):641–647
FitzGerald MP, Mulligan M, Parthasarathy S (2006) Nocturic frequency is related to severity of obstructive sleep apnea, improves with continuous positive airways treatment. Am J Obstet Gynecol 194(5):1399–1403
Listed N (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Middelkoop HA et al (1996) Subjective sleep characteristics of 1,485 males and females aged 50-93: effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol A Biol Sci Med Sci 51(3):M108–M115
Umlauf MG, Chasens ER, Greevy RA, Arnold J, Burgio KL, Pillion DJ (2004) Obstructive sleep apnea, nocturia and polyuria in older adults. Sleep 27(1):139–144
Endeshaw YW, Johnson TM, Kutner MH, Ouslander JG, Bliwise DL (2004) Sleep-disordered breathing and nocturia in older adults. J Am Geriatr Soc 52(6):957–960
Nigro CA, Dibur E, Borsini E, Malnis S, Ernst G, Bledel I, González S, Arce A, Nogueira F (2018) The influence of gender on symptoms associated with obstructive sleep apnea. Sleep Breathing 22(3):683–693
Ono J, Chishaki A, Ohkusa T, Sawatari H, Nishizaka M, Ando S (2015) Obstructive sleep apnea-related symptoms in Japanese people with Down syndrome. Nurs Health Sci 17(4):420–425
Goyal A, Pakhare A, Chaudhary P (2019) Nocturic obstructive sleep apnea as a clinical phenotype of severe disease. Lung India 36(1):20–27
Author information
Authors and Affiliations
Contributions
Liu: project development, data collection, and manuscript writing. Zhou: data collection and manuscript editing. Xia: manuscript editing and critical revisions. Li: manuscript editing and critical revisions.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All processes conducted in studies were in accordance with the ethical standards of the institutional. Due to this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, J., Xia, S., Li, T. et al. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath 24, 1293–1298 (2020). https://doi.org/10.1007/s11325-019-01981-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01981-6