Abstract
Purpose
Although mixed sleep apnea (MSA) is one of the three types of sleep apnea, it is not considered a separate disease entity. It is generally seen as a part of obstructive sleep apnea-hypopnea syndrome (OSAHS), but its implications are often ignored. In this study, we examined its features and the potential impact on OSAHS patients.
Methods
Subjects diagnosed with OSAHS by polysomnography (PSG) were enrolled. All participants underwent physical checkups and tests of blood biochemistry. They were anthropometrically, clinically, and polysomnographically studied.
Results
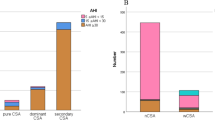
MSA events were common in patients with severe OSAHS patients. There were significant differences between the pure OSAHS group and its mixed counterpart in apnea-hypopnea indices during REM (AHIREM) and non-REM (AHINREM) and in percentages of N2 or N3 sleep. Logistic regression analysis showed that, after adjustment of other parameters, patients with MSA events were mostly male, had higher body mass index (BMI), higher scores on Epworth Sleepiness Scales (ESS), higher triglyceride (TG) levels, and higher apnea-hypopnea index (AHI). The combined predictive probability of the aforementioned variables was 0.766 (95% CI = 0.725~0.806; sensitivity 61.6%, specificity 82.1%).
Conclusions
Our study suggested that MSA was related to the stability of the ventilatory control in OSAHS patients. MSA events occur more frequently in patients with severe OSAHS, and male gender, obesity, daytime sleepiness, and elevated TG levels were risk factors for the mixed OSAHS.


Similar content being viewed by others
References
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28:499–521
Zaharna M, Rama A, Chan R, Kushida C (2013) A case of positional central sleep apnea. J Clin Sleep Med 9:265–268. https://doi.org/10.5664/jcsm.2496
Malhotra A, Owens RL (2010) What is central sleep apnea? Respir Care 55:1168–1178
Iber C, Ancoli-Israel S, Chesson AL et al (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine, Westchester
Iber C, Davies SF, Chapman RC, Mahowald MM (1986) A possible mechanism for mixed apnea in obstructive sleep apnea. Chest 89:800–805
The Report of an American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Yamauchi M, Tamaki S, Yoshikawa M, Ohnishi Y, Nakano H, Jacono FJ, Loparo KA, Strohl KP, Kimura H (2011) Differences in breathing patterning during wakefulness in patients with mixed apnea-dominant vs obstructive-dominant sleep apnea. Chest 140:54–61. https://doi.org/10.1378/chest.10-1082
Xie A, Bedekar A, Skatrud JB, Teodorescu M, Gong Y, Dempsey JA (2011) The heterogeneity of obstructive sleep apnea (predominant obstructive vs pure obstructive apnea). Sleep 34:745–750. https://doi.org/10.5665/SLEEP.1040
Lee SA, Lee GH, Chung YS, Kim WS (2015) Clinical, polysomnographic, and CPAP titration features of obstructive sleep apnea: mixed versus purely obstructive type. J Neurol Sci 355:150–154. https://doi.org/10.1016/j.jns.2015.06.005
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Chami HA, Baldwin CM, Silverman A, Zhang Y, Rapoport D, Punjabi NM, Gottlieb DJ (2010) Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. Am J Respir Crit Care Med 181:997–1002. https://doi.org/10.1164/rccm.200908-1304OC
Eckert DJ, Malhotra A, Jordan AS (2009) Mechanisms of apnea. Prog Cardiovasc Dis 51:313–323. https://doi.org/10.1016/j.pcad.2008.02.003
Younes M (2008) Role of respiratory control mechanisms in the pathogenesis of obstructive sleep disorders. J Appl Physiol (1985) 105:1389–1405. https://doi.org/10.1152/japplphysiol.90408.2008
Younes M, Ostrowski M, Thompson W et al (2001) Chemical control stability in patients with obstructive sleep apnea. Am J Respir Crit Care Med 163:1181–1190. https://doi.org/10.1164/ajrccm.163.5.2007013
Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A (2013) Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 188:996–1004. https://doi.org/10.1164/rccm.201303-0448OC
Wellman A, Edwards BA, Sands SA, Owens RL, Nemati S, Butler J, Passaglia CL, Jackson AC, Malhotra A, White DP (2013) A simplified method for determining phenotypic traits in patients with obstructive sleep apnea. J Appl Physiol (1985) 114:911–922. https://doi.org/10.1152/japplphysiol.00747.2012
Edwards BA, Eckert DJ, McSharry DG et al (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190:1293–1300. https://doi.org/10.1164/rccm.201404-0718OC
Landry SA, Andara C, Terrill PI, Joosten SA, Leong P, Mann DL, Sands SA, Hamilton GS, Edwards BA (2018) Ventilatory control sensitivity in patients with obstructive sleep apnea is sleep stage dependent. Sleep 41. https://doi.org/10.1093/sleep/zsy040
Sands SA, Owens RL, Malhotra A (2016) New approaches to diagnosing sleep-disordered breathing. Sleep Med Clin 11:143–152. https://doi.org/10.1016/j.jsmc.2016.01.005
Li Y, Ye J, Han D, Cao X, Ding X, Zhang Y, Xu W, Orr J, Jen R, Sands S, Malhotra A, Owens R (2017) Physiology-based modeling may predict surgical treatment outcome for obstructive sleep apnea. J Clin Sleep Med 13:1029–1037. https://doi.org/10.5664/jcsm.6716
Shi R, Conrad SA (2009) Correlation and regression analysis. Ann Allergy Asthma Immunol 103:S35–S41
Katsumata Y, Todoriki H, Higashiuesato Y, Yasura S, Ohya Y, Willcox DC, Dodge HH (2013) Very old adults with better memory function have higher low-density lipoprotein cholesterol levels and lower triglyceride to high-density lipoprotein cholesterol ratios: KOCOA project. J Alzheimers Dis 34:273–279. https://doi.org/10.3233/JAD-121138
Vieira JR, Elkind MS, Moon YP et al (2011) The metabolic syndrome and cognitive performance: the Northern Manhattan Study. Neuroepidemiology 37:153–159. https://doi.org/10.1159/000332208
van den Kommer TN, Dik MG, Comijs HC, Jonker C, Deeg DJH (2012) Role of lipoproteins and inflammation in cognitive decline: do they interact? Neurobiol Aging 33:191–196. https://doi.org/10.1016/j.neurobiolaging.2010.05.024
Peng Y, Zhou L, Cao Y, Chen P, Chen Y, Zong D, Ouyang R (2017) Relation between serum leptin levels, lipid profiles and neurocognitive deficits in Chinese OSAHS patients. Int J Neurosci 127:981–987. https://doi.org/10.1080/00207454.2017.1286654
Acknowledgements
We are indebted to all the subjects who took part in this study and the staff of the Sleep Center of Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
Funding
This work is supported by the National Natural Science Foundation of China (81570903).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Tongji Medical College, Huazhong University of Science and Technology and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yang, X., Xiao, Y., Han, B. et al. Implication of mixed sleep apnea events in adult patients with obstructive sleep apnea-hypopnea syndrome. Sleep Breath 23, 559–565 (2019). https://doi.org/10.1007/s11325-018-1745-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1745-0