Abstract
Purpose
Our goal in this study is to determine the prevalence and associated factors of obstructive sleep apnea (OSA) in morbidly obese patients undergoing bariatric surgery.
Methods
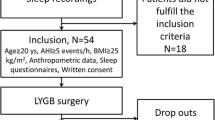
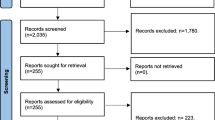
This descriptive study was conducted at King Chulalongkorn Memorial Hospital from 2007 to 2015. Data of morbidly obese patients who underwent bariatric surgery were included using ICD-10 code for principle diagnosis “morbid obesity” (E668) and ICD-9 code for “bariatric surgery” (4389, 4438, 4439).
Results
Baseline characteristics of 238 patients who met the inclusion criteria demonstrated 49.2% male, mean age of 33.9 ± 10.8 years, and mean BMI of 52.6 ± 11.6. Sleeve gastrectomy and Roux-en Y gastric bypass surgery were performed in 51.5 and 48.5%; respectively. High risk for OSA using STOP-Bang as a screening questionnaire (≥3 points) was 92.7%. The prevalence of OSA using respiratory disturbance index (RDI) ≥ 5 was demonstrated at 85.7%. Mild, moderate, and severe OSA was observed in 8.8, 15.3, and 75.9%, respectively. Snoring, STOP-Bang score ≥ 3, fatty liver, and BMI were significantly correlated with OSA compared to the group without OSA with the odds ratio of 17.04 (p = <0.0001, 95% CI = 6.67–43.49), 16 (p = 0.01, 95% CI = 1.95–131.11), 4.75 (p = 0.001, 95% CI = 1.82–12.37), and 1.04 (p = 0.045, 95% CI = 1.0009–1.09), respectively. Comparison between non-severe and severe OSA groups demonstrated dyslipidemia and BMI to be correlated with OSA severity (odds ratio = 3.06, 95% CI 1.36–6.89, p = 0.007 and odds ratio = 1.07, 95% CI 1.03–1.13, p = 0.001, respectively).
Conclusions
Obstructive sleep apnea is frequently observed in morbidly obese patients undergoing bariatric surgery and the severity tends to be severe. Snoring, STOP-Bang score ≥ 3, fatty liver, and BMI were significantly correlated with OSA. Dyslipidemia and BMI were demonstrated to be associated factors for severity of OSA in this population.

Similar content being viewed by others
References
World Health Organization (2014) Obesity and overweight fact sheet. Publishing WHO, Charlotte http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 10 October 2014
Department of health (2013) Database of nutritional status in Thai people older than 15 years in 2009 and 2013. Publishing anamai, Thailand http://www.anamai.moph.go.th/main.php?filename =Statistics. Accessed 10 October 2014
Vasu TS, Grewal R, Doghramji K (2012) Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. J Clin Sleep Med 8(2):199–207. doi:10.5664/jcsm.1784
Lee YH, Johan A, Huat Wong KK, Edwards N, Sullivan C (2009) Prevalence and risk factors for obstructive sleep apnea in a multiethnic population of patients presenting for bariatric surgery in Singapore. Sleep Med 10:226–232. doi:10.1016/j.sleep.2008.01.005
Lopez PP, Stefan B, Schulman CL, Byers PM (2008) Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg 74:834–838
Khan A, King WC, Patterson EJ, Laut J, Raum W, Courcoulas AP et al (2013) Assessment of obstructive sleep apnea in adults undergoing bariatric surgery in the longitudinal assessment of bariatric surgery-2 (LABS-2) study. J Clin Sleep Med 9:21–29. doi:10.5664/jcsm.2332
Yeh PS, Lee YC, Lee WJ, Chen SB, Ho SJ, Peng WB et al (2010) Clinical predictors of obstructive sleep apnea in Asian bariatric patients. Obes Surg 20:30–35. doi:10.1007/s11695-009-9854-2
Daltro C, Gregorio PB, Alves E, Abreu M, Bomfim D, Chicourel MH et al (2007) Prevalence and severity of sleep apnea in a group of morbidly obese patients. Obes Surg 17:809–814. doi:10.1007/s11695-007-9147-6
Serafini FM, Anderson WM, Rosemurgy AS, Strait T, Murr MM (2000) Clinical predictors of sleep apnea in patients undergoing bariatric surgery. Obes Surg 11:28–31
World Health Organisation (1999) 10 facts on obesity. Publishing WHO, Charlotte http://www.who.int/features/factfiles/obesity/facts/en/. Accessed 10 October 2014
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108(5):812–821. doi:10.1097/ALN.0b013e31816d83e4
Banhiran W, Durongphan A, Saleesing C, Chongkolwatana C (2014) Diagnostic properties of the STOP-Bang and its modified version in screening for obstructive sleep apnea in Thai patients. J Med Assoc Thai 2014 97(6):644–654
Johns MW (1991) A new method for measuring daytime sleeping: the Epworth sleepiness scale. Sleep 14:540–545
Banhiran W, Assanasen P, Nopmaneejumruslers C, Metheetrairut C (2011) Epworth sleepiness scale in obstructive sleep disordered breathing: the reliability and validity of the Thai version. Sleep Breath 15(3):571–577. doi:10.1007/s11325-010-0405-9
Darien IL (2014) International classification of sleep disorders, 3nd edn. American Academy of Sleep Medicine, Westchester
Iber C, Ancoli-Israel S, Chesson A, Quan SF (2015) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. American Academy of Sleep Medicine Version 2, Darien, IL
Chirakalwasan N, Teerapraipruk B, Simon R, Hirunwiwatkul P, Jaimchariyatam N, Desudchit T et al (2013) Comparison of polysomnographic and clinical presentations and predictors for cardiovascular-related diseases between non-obese and obese obstructive sleep apnea among Asians. J Clin Sleep Med 9(6):553–555. doi:10.5664/jcsm.2748
Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S et al (2015) Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One 10(12):1–21. doi:10.1371/journal.pone.0143697
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kositanurit, W., Muntham, D., Udomsawaengsup, S. et al. Prevalence and associated factors of obstructive sleep apnea in morbidly obese patients undergoing bariatric surgery. Sleep Breath 22, 251–256 (2018). https://doi.org/10.1007/s11325-017-1500-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1500-y