Abstract
Objective
To introduce a new classification, aiming to correspond TMJ disc configuration with diagnosis, meanwhile reduce difficulty and subjectivity in TMJ MRI evaluation and training of TMD diagnosis for dental students.
Methods
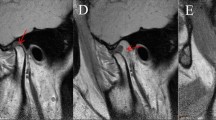
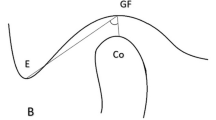
90 patients sought for TMD treatment were enrolled in the study, whose MRIs were used to establish the new classification. A total of 180 discs were evaluated using MRI for position (normal, DDWR or DDWoR) and classified by morphology according to previous (Murakami’s classification) and new classification respectively. 60 discs were selected and judged by two groups (2 TMJ specialists and 30 dental students) to assess the reliability and validity of the new classification. Questionnaires were acquired for all observers to assess the attitude toward two classification systems. Descriptive statistics, Spearman’s rank correlation coefficient, and intraclass correlation coefficient were performed. P < 0.05 was considered statistically significant.
Results
In the new classification, Class 1 disc was significantly correlated with DDWR and Class 3 disc was significantly correlated with DDWoR. Interobserver reliability/consistency for observers between TMJ specialists was 0.867 when Murakami’s classification was applied and 0.948 when the new classification was applied. Interobserver ICC value for dental students was 0.656 when using Murakami’s classification, and 0.831 when using the new classification. The difference in attitude toward different classification systems was statistically significant.
Conclusion
A new classification of TMJ disc configuration is presented. The correlation between disc morphology and position revealed helps diagnosis and management. The new classification improves TMJ MRI interpreting accuracy and provides a better learning and using experience.





Similar content being viewed by others
Change history
11 June 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11282-022-00627-w
References
Westesson PL, Rohlin M. Internal derangement related to osteoarthrosis in temporomandibular joint autopsy specimens. Oral Surg Oral Med Oral Pathol. 1984;57(1):17–22.
Arayasantiparb R, Tsuchimochi M, Mitrirattanakul S. Transformation of temporomandibular joint disc configuration in internal derangement patients using magnetic resonance imaging. Oral Sci Int. 2012;9:43–8.
Vogl TJ, Lauer HC, Lehnert T, et al. The value of MRI in patients with temporomandibular joint dysfunction: correlation of MRI and clinical findings. Eur J Radiol. 2016;85(4):714–9.
Yoshida H, Hirohata H, Onizawa K, et al. Flexure deformation of the temporomandibular joint disk in pseudodynamic magnetic resonance images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(1):104–11.
Taşkaya-Yilmaz N, Oğütcen-Toller M. Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J Oral Maxillofac Surg. 2001;59(8):860–5.
Matsubara R, Yanagi Y, Oki K, et al. Assessment of MRI findings and clinical symptoms in patients with temporomandibular joint disorders. Dentomaxillofac Radiol. 2018;47(4):20170412.
Pinto GNS, Grossmann E, Iwaki FL, et al. Correlation between joint effusion and morphology of the articular disc within the temporomandibular joint as viewed in the sagittal plane in patients with chronic disc displacement with reduction: a retrospective analytical study from magnetic resonance imaging. Cranio. 2021;39(2):119–24.
Koh KJ, Park HN, Kim KA. Relationship between anterior disc displacement with/without reduction and effusion in temporomandibular disorder patients using magnetic resonance imaging. Imaging Sci Dent. 2013;43(4):245–51.
Dias IM, Cordeiro PC, Devito KL, et al. Evaluation of temporomandibular joint disc displacement as a risk factor for osteoarthrosis. Int J Oral Maxillofac Surg. 2016;45(3):313–7.
Roh HS, Kim W, Kim YK, et al. Relationships between disk displacement, joint effusion, and degenerative changes of the TMJ in TMD patients based on MRI findings. J Craniomaxillofac Surg. 2012;40(3):283–6.
Rudisch A, Innerhofer K, Bertram S, et al. Magnetic resonance imaging findings of internal derangement and effusion in patients with unilateral temporomandibular joint pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(5):566–71.
Ottl P, Hohmann A, Piwowarczyk A, et al. Retrospective study on the evaluation of the TMJ by MRI using a newly developed standardized evaluation form. Cranio. 2008;26(1):33–43.
Murakami S, Takahashi A, Nishiyama H, et al. Magnetic resonance evaluation of the temporomandibular joint disc position and configuration. Dentomaxillofac Radiol. 1993;22(4):205–7.
Ottl P, Hohmann A, Piwowarczyk A, et al. Assessment of the temporomandibular joint using MRI and a new standardised evaluation form. Aktuelle Rheumatol. 2007;32(2):86–91.
Schmitter M, Kress B, Hähnel S, et al. The effect of quality of temporomandibular joint MR images on interrater agreement. Dentomaxillofac Radiol. 2004;33(4):253–8.
Widmalm SE, Brooks SL, Sano T, et al. Limitation of the diagnostic value of MR images for diagnosing temporomandibular joint disorders. Dentomaxillofac Radiol. 2006;35(5):334–8.
Hirata FH, Guimarães AS, Oliveira JX, et al. Evaluation of TMJ articular eminence morphology and disc patterns in patients with disc displacement in MRI. Braz Oral Res. 2007;21(3):265–71.
De Farias JF, Melo SL, Bento PM, et al. Correlation between temporomandibular joint morphology and disc displacement by MRI. Dentomaxillofac Radiol. 2015;44(7):20150023.
Serindere G, Aktuna BC. MRI investigation of TMJ disc and articular eminence morphology in patients with disc displacement. J Stomatol Oral Maxillofac Surg. 2021;122(1):3–6.
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network* and orofacial pain special interest group†. J Oral Fac Pain Headache. 2014;28(1):6–27.
Kumar R, Pallagatti S, Sheikh S, et al. Correlation between clinical findings of temporomandibular disorders and MRI characteristics of disc displacement. Open Dent J. 2015;9:273–81.
Orhan K, Nishiyama H, Tadashi S, et al. Comparison of altered signal intensity, position, and morphology of the TMJ disc in MR images corrected for variations in surface coil sensitivity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(4):515–22.
Koca CG, Gümrükçü Z, Bilgir E. Does clinical findings correlate with magnetic resonance imaging (MRI) findings in patients with temporomandibular joint (TMJ) pain? A cross sectional study. Med Oral Patol Oral Cir Bucal. 2020;25(4):e495–501.
Almăşan OC, Hedeşiu M, Băciuţ G, et al. Disk and joint morphology variations on coronal and sagittal MRI in temporomandibular joint disorders. Clin Oral Investig. 2013;17(4):1243–50.
Emshoff R, Bertram A, Hupp L, et al. Condylar erosion is predictive of painful closed lock of the temporomandibular joint: a magnetic resonance imaging study. Head Face Med. 2021;17(1):40.
Emshoff R, Bertram A, Hupp L, et al. A logistic analysis prediction model of TMJ condylar erosion in patients with TMJ arthralgia. BMC Oral Health. 2021;21(1):374.
Hegab AF, Al Hameed HI, Karam KS. Classification of temporomandibular joint internal derangement based on magnetic resonance imaging and clinical findings of 435 patients contributing to a nonsurgical treatment protocol. Sci Rep. 2021;11(1):20917.
Minston W, Benchimol D, Jacobs R, et al. Pre-surgical radiographic and clinical features as predictors for temporomandibular joint discectomy prognosis. Oral Dis. 2021. https://doi.org/10.1111/odi.13923.
Hegab AF, Youssef AH, Hameed H, et al. MRI-based determination of occlusal splint thickness for temporomandibular joint disk derangement: a randomized controlled clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(1):74–87.
Polat ME, Yanik S. Efficiency of arthrocentesis treatment for different temporomandibular joint disorders. Int J Oral Maxillofac Surg. 2020;49(5):621–7.
Xiong X, Yin X, Liu F, et al. Magnetic resonance imaging-guided disc-condyle relationship adjustment via articulation: a technical note and case series. J Int Med Res. 2020;48(8):300060520951052.
Funding
This study was funded by Chengdu Science and technology Bureau (Grant/Award Number: 2019-YF05-00508-SN); Sichuan University (Grant/Award Number: 2018SCUH0082) and West China Hospital of Stomatology (Grant/Award Number: RD-03-202005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Institution Review Board of the West China Hospital of Stomatology, Sichuan University, China) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for which identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qinlanhui Zhang and Xin Xiong contributed equally to this work
Rights and permissions
About this article
Cite this article
Zhang, Q., Xiong, X., Gong, Y. et al. Introducing a novice-friendly classification system for magnetic resonance imaging of the temporomandibular joint disc morphology. Oral Radiol 39, 143–152 (2023). https://doi.org/10.1007/s11282-022-00615-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-022-00615-0