Abstract
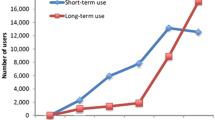
Direct oral anticoagulants (DOACs) have been introduced within the last years as alternative to vitamin K antagonists (VKAs) as oral anticoagulant drugs (OAC). The mean/median age of the patients included in DOAC-investigating trials was 70–72 years. The age-pattern of patients to whom DOAC are prescribed in clinical settings is largely unknown. Thus, aim of the study was to assess the age-pattern of patients who received OAC in the years 2011–2014 in Austria. The data analysis refers to the accounting data of the 13 major health insurance funds, covering >97 % of the Austrian population. The number of patients who received OAC in 2011–2014 increased by 43 % (182,464–261,347). Patients who received DOACs increased nearly fivefold (20,927–96,247), whereas patients who received VKAs increased by only 2 % (161,537–165,100). In 2011, the age of patients receiving VKAs was higher than DOACs (72 vs. 68 years), whereas in 2014, the age of the patients receiving VKAs was lower than DOACs (73 vs. 74 years). The proportion of patients ≥80 years receiving VKAs declined from 26 to 21 % of all OAC, receiving DOACs increased from 1 to 12 %. Among nonagenarians, the proportion of patients receiving VKAs remained 2 % (3316–5858), whereas the proportion of patients receiving DOACs increased 40-fold (91–4296). DOACs are prescribed to patients ≥80 years, although there are is a lack of data about efficacy and safety. There is an urgent need for data about this patient group. Since a randomized trial is rather unlikely in this specific age group we suggest subgroup analyses about octo-and nonagenarians, in case they have been included in previously completed or still ongoing trials or registries for OAC.



Similar content being viewed by others
References
Caldeira D, Rodrigues FB, Barra M, Santos AT, de Abreu D, Gonçalves N, Pinto FJ, Ferreira JJ, Costa J (2015) Non-vitamin K antagonist oral anticoagulants and major bleeding-related fatality in patients with atrial fibrillation and venous thromboembolism: a systematic review and meta-analysis. Heart 101:1204–1211. doi:10.1136/heartjnl-2015-307489
Camm AJ, Lip GY, De Caterina R et al (2012) 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 33:2719–2747. doi:10.1093/eurheartj/ehs253
Konstantinides SV, Torbicki A, Agnelli G et al (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35(43):3033–3069. doi:10.1093/eurheartj/ehu283
Hägg L, Johansson C, Jansson JH, Johansson L (2014) External validity of the ARISTOTLE trial in real-life atrial fibrillation patients. Cardiovasc Ther 32:214–218. doi:10.1111/1755-5922.12087
Ruff CT, Giugliano RP, Braunwald E et al (2014) New oral anticoagulants in patients with atrial fibrillation—authors’ reply. Lancet 384:25–26. doi:10.1016/S0140-6736(14)61106-5
Xu Y, Holbrook AM, Simpson CS, Dowlatshahi D, Johnson AP (2013) Prescribing patterns of novel oral anticoagulants following regulatory approval for atrial fibrillation in Ontario, Canada: a population-based descriptive analysis. CMAJ Open 16:E115–E119. doi:10.9778/cmajo.20130032
Olesen JB, Sørensen R, Hansen ML, Lamberts M, Weeke P, Mikkelsen AP, Køber L, Gislason GH, Torp-Pedersen C, Fosbøl EL (2015) Non-vitamin K antagonist oral anticoagulation agents in anticoagulant naïve atrial fibrillation patients: Danish nationwide descriptive data 2011–2013. Europace 17:187–193. doi:10.1093/europace/euu225
Metcalfe S, Moodie P (2012) National prescribing data for dabigatran. N Z Med J 125:97–105
Steinberg BA, Holmes DN, Piccini JP, Ansell J, Chang P, Fonarow GC, Gersh B, Mahaffey KW, Kowey PR, Ezekowitz MD, Singer DE, Thomas L, Peterson ED, Hylek EM, Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) Investigators and Patients (2013) Early adoption of dabigatran and its dosing in US patients with atrial fibrillation: results from the outcomes registry for better informed treatment of atrial fibrillation. J Am Heart Assoc 2:e000535. doi:10.1161/JAHA.113.000535
Pratt NL, Ramsay EN, Caughey GE, Shakib S, Roughead EE (2016) Uptake of novel oral anticoagulants in Australia. Med J Aust 204:104–105
Dreischulte T, Barnett K, Madhok V, Guthrie B (2014) Use of oral anticoagulants in atrial fibrillation is highly variable and only weakly associated with estimated stroke risk: cross-sectional population database study. Eur J Gen Pract 20:181–189. doi:10.3109/13814788.2013.852535
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 383:955–962. doi:10.1016/S0140-6736(13)62343-0
Chatterjee S, Sardar P, Biondi-Zoccai G, Kumbhani DJ (2013) New oral anticoagulants and the risk of intracranial hemorrhage: traditional and Bayesian meta-analysis and mixed treatment comparison of randomized trials of new oral anticoagulants in atrial fibrillation. JAMA Neurol 70:1486–1490. doi:10.1001/jamaneurol.2013.4021
Stöllberger C, Finsterer J (2013) Concerns about the use of new oral anticoagulants for stroke prevention in elderly patients with atrial fibrillation. Drugs Aging 30:949–958. doi:10.1007/s40266-013-0119-3
Pottegård A, Poulsen BK, Larsen MD, Hallas J (2014) Dynamics of vitamin K antagonist and new oral anticoagulants use in atrial fibrillation: a Danish drug utilization study. J Thromb Haemost 12:1413–1418. doi:10.1111/jth.12662
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schuh, T., Reichardt, B., Finsterer, J. et al. Age-dependency of prescribing patterns of oral anticoagulant drugs in Austria during 2011–2014. J Thromb Thrombolysis 42, 447–451 (2016). https://doi.org/10.1007/s11239-016-1380-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1380-1