Abstract
Novel susceptibility genes related to ischemic stroke (IS) are proposed in recent literatures. Population-based replicate studies would cause false positive results due to population stratification. 229 recruit IS patients and their 229 non-IS siblings were used in this study to avoid population stratification. The family-based study was conducted in Beijing from June 2005 to June 2012. Association between SNPs and IS was found in the sibship discordant tests, and the conditional logistic regression was performed to identify effect size and explore gene–environment interactions. Significant allelic association was identified between NINJ2 gene rs11833579 (P = 0.008), protein kinase C η gene rs2230501 (P = 0.039) and IS. The AA genotype of rs11833579 increased 1.51-fold risk (95 % CI 1.04–3.46; P = 0.043) of IS, and it conferred susceptibility to IS only in a dominant model (OR 2.69; 95 % CI 1.06–6.78; P = 0.036]. Risk of IS was higher (HR 3.58; 95 % CI 1.54–8.31; P = 0.003) especially when the carriers of rs11833579 AA genotype were smokers. The present study suggests A allele of rs11833579 may play a role in mediating susceptibility to IS and it may increase the risk of IS together with smoking.
Similar content being viewed by others
Introduction
Stroke is the leading cause of neurological disability and it is one of the leading causes of death worldwide [1], and ischemic stroke (IS) is the major type of stroke in China [2]. Although genome wide association study (GWAS) and genetic studies based on candidate genes have provided numerous probable susceptibility locus, a large part of genetic risks of IS remains unexplained.
Several candidate genes were identified for IS based on genome-wide linkage search and subsequent fine-mapping in the past decades, such as PDE4D gene [3], ALOX5AP gene [4], and protein kinase C η (PRKCH) gene [5]. Besides, candidate genes were also proposed and demonstrated based on different pathways of pathogenic mechanisms, such as Selenoprotein S (SEPS1) gene which involved in the regulation of inflammatory response and protection from oxidative damage [6]. GWAS has been used in exploring genetic risk factors of IS since 2007, and has provided more replicable novel genetic markers, such as rs10757278 in 9p21 [7] and rs11833579 encoded NINJ2 [8]. Numerous replicate studies are needed to perform in various populations in order to provide more solid evidence of causality. To date, most studies aim at confirming previous susceptibility locus are population-based case control study, however, this kind of study design will cause misleading false positive results because of population stratification. Therefore, we used a random non-IS sibling of IS patients as matched control, and carried out family-based case control study to confirm the association between single nucleotide polymorphisms (SNPs) in several novel genes and IS.
As with most complex diseases, IS is likely to be influenced not only by genetic, but also by environmental components. Traditional cardiovascular disease risk factors, such as cigarette smoking and alcohol drinking, may increase the risk of IS [9, 10]. Some of these traditional risk factors may dramatically increase risk of disease together with risk alleles. Identification of interactions between genetic and environment components will help to recognize individuals with high risk in developing IS, and make cost-effective prevention strategies. Thus, the joint effects of traditional environment risk factors and genes which have main effect in IS were also investigated in the present study.
Methods
Study population and data collection
Following the protocol of Fangshan/Family-based Ischemic Stroke Study in China (FISSIC) [11], the subjects were recruited in Fangshan from June 2005 to June 2012. Fangshan located in southwest of Beijing is a district with high prevalence of cardiovascular disease including IS [12]. IS patients aged above 18 years old with computerized tomography (CT) or magnetic resonance imaging (MRI) confirmed were recruited in the First Hospital of Fangshan District. Patients are eligible for inclusion if they have at least one parents or a full sibling aged above 18 years participating in the study.
Demographic characters (age, sex, etc.), lifestyle risk factors (cigarette smoking etc.) and medical history (diagnose and treatment of stroke and other chronic disease) were collected through a face-to-face interview by trained interviewers using uniform questionnaires. Current smoker was defined as the one who smoked more than 100 cigarettes and still smoking during last 1 month, past smoker was defined as the one who had smoked that amount of cigarettes but have not smoke for at least 1 month, and non-smoker are those who has smoked <100 cigarettes accumulatively. In the analysis, current smokers and past smokers were both treated as smokers. Anthropometric measurements were obtained by trained and certified observers. Blood pressure was measured three times at the right brachial artery using a sphygmomanometer after the participant has rested in a seated position for 5 min. Concentrations of total cholesterol, triglycerides, and high-density lipoprotein cholesterol were measured with Hitachi 7180 auto-analyzer (Hitachi High-Technologies Corp., Tokyo, Japan) in central clinical laboratory, Central Hospital.
This study had been approved by the ethics committee of Peking University Health Sciences Center. Each participant had been informed about the study and they had agreed for blood sampling and physical examination in this study. All subjects had signed an informed consent prior to participating in the study. In the end, we recruited 229 unrelated Chinese patients with their 229 full sibling non-IS controls.
DNA extraction and genotyping
We selected 13 SNPs to test their association with IS. Genomic DNA was extracted from the peripheral blood with a DNA extraction kit (DP319-01; Tiangen Biotech, Beijing, China). The PCR was performed on a thermal cycler (ABI GeneAmp 9700 384 Dual; ABI, Foster City, CA, USA). Genotypes were analyzed with Typer 4.0 software (MassARRAY Compact System; Sequenom, San Diego, CA, USA). All SNPs in this report had a genotyping success rate of >98 %.
Statistical analysis
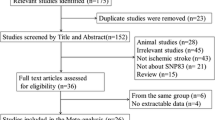
The initial data set contains singleton families and multiplex families. The 199 singleton families contain only one affected individual and at least one unaffected siblings. The 44 multiplex families comprise families with at least 2 affected siblings, and any number of unaffected siblings. After excluding 14 multiplex families which have no unaffected siblings, we recruited a total of 229 families in the association study. For this study, in affected group, one case from each family was selected. In unaffected group, one non-IS siblings of IS patient from each families was randomly selected.
During data analysis process, means and standard deviations (SDs) were reported for continuous variables, and percentages were reported for categorical variables. Paired sample t test was used to examine the difference of continuous variables, and McNemar’s Chi squared tests were used to test for the difference of categorical variables. Each SNP was tested separately for deviation from Hardy–Weinberg equilibrium (HWE) in control group using Chi squared test. We used the sibship disequilibrium test (SDT) to test association between SNPs and IS in the first step. Conditional logistic regression served as a second method to confirm the SDT results and provided estimates of relative risks. We analyzed the family-based data, by using the procedure COX regression in IBM SPSS Statistics 20.0 software, to fit the conditional logistic regression model and search for gene-environment interactions. All P values were two-tailed, with statistical significance defined as <0.05.
Results
We used 229 case-sibling pairs in this association study. Of the 229 IS patients, 157 (57.9 %) were male, which were significantly more than control group (P < 0.001, Table 1). The patients were significantly elder than controls (P = 0.002). The percent of IS cases that had ever smoked cigarettes was significantly higher than controls (58.6 vs. 41.4 %, P = 0.001). Systolic and diastolic blood pressures were significantly higher in cases than controls (P ≤ 0.001). There was no significant difference of the concentration of total cholesterol between patients and controls (P = 0.366), while the concentration of HDL-cholesterol (HDLC) was significantly higher in patients than controls (P < 0.001).
All 13 SNPs showed no significant deviation from Hardy–Weinberg equilibrium in the control group (P > 0.05). The results of SDT and allele frequencies for patients and controls were shown in Table 2. Significant associations with IS were found in NINJ2 gene rs11833579 (P = 0.008), PRKCH gene rs2230501 (P = 0.039). The A allele frequency in rs11833579 was significantly higher in stroke patients (40.0 %) than that of unaffected controls (33.6 %). The C allele of rs2230501 is significantly higher in stroke patients (22.9 %) than that of unaffected controls (19.4 %).
Conditional logistic regression validated the significant association of rs11833579 and rs2230501 with IS. Table 3 showed that, before any adjustments, the A allele of rs11833579 was the risk allele of IS in dominant model [odds ratio (OR) 2.17, 95 % CI 1.01–4.76, P = 0.049]. The AA genotype of rs11833579 increased risk of IS 3.04-fold relative to the GG genotype (95 % CI 1.14–8.16, P = 0.027). After adjusting for age, sex, hypertension, diabetes, serum lipids and smoke, the A allele of rs11833579 could increase 2.69-fold risk of IS (95 % CI 1.06–6.78; P = 0.036) in dominant model. The AA genotype of rs11833579 could increase 1.51-fold risk of IS (95 % CI 1.04–3.46, P = 0.043). For rs2230501, after multiple adjustments, the AC genotype gave a 2.93-fold increased risk of IS relative to the AA genotype (95 % CI 1.07–8.00, P = 0.036).
Smoking had significant interaction with rs111833579 in IS (Table 4). The odds ratios (OR) to IS rise continuously as the increasing number of risk allele in rs11833579 and ORs rise more distinct if risk allele carriers were also smokers. The AA genotype could increase 3.58 times of risk in smokers than GG genotype in non-smokers (95 % CI 1.54–8.31, P = 0.003), and 3.17-fold IS risk than GG/GA genotype non-smokers (95 % CI 1.46–6.88, P = 0.004). After adjusting for age and sex, the AA genotype of smokers could increase 2.72-fold risk of IS (95 % CI 1.09–6.78, P = 0.032) than the GG genotype of non-smokers, and increase 2.41-fold risk of IS than GG/GA genotype non-smokers (95 % CI 1.04–5.61, P = 0.041).
Discussion
Our study described the association between novel SNPs and IS using case-sibling matched case–control study in Chinese population. We revealed that rs11833579 near NINJ2 gene was significantly associated with IS. In addition, we also found a significant interaction of rs11833579 and smoking in IS. The strength of our study include well characteristic IS patients with imaging data, and the usage of non-IS sibling as matched control, so as to reduce false positive rate due to population stratification. Additionally, Fangshan District, where our study was conducted, was located in the “stroke belt” of China similar to the “stroke belt” in the south-eastern United States, and its population was representative of the rural northern Han Chinese. Besides, to our knowledge, it is the first study to examine the interaction of smoke and rs11833579 in IS.
Ninjurin2 (NINJ2), which is a cell surface adhesion molecule, plays a role in nerve regeneration via hemophilic interaction [13]. Rs11833579 locates on chromosome 12p13 proximity to NINJ2 gene and encode Ninjurin2. The result of our study was consistent with the previous genome-wide association study which demonstrated that rs11833579 were associated with IS in Caucasians [8]. Similarly, some replicate study in Asia also found the association between rs11833579 and IS [14, 15]. Tong et al. [15] reported that the A allele of rs11833579 was significantly associated with IS in the Han population (OR 1.27, 95 % CI 1.08–1.49), and rs11833579 conferred susceptibility to IS in recessive model (P = 0.004). On the contrary, another Chinese study showed that there was no statistically significant association between rs11833579 and IS [16]. Besides, a study included 137 IS patients and 66 controls from Nanjing China, also found no association between rs11833579 and IS [17]. The difference may be explained by the several possibilities: (1) Our study was conducted in a population with stable genetic background in North China, the studies provide different results recruited their samples in South China [16, 17], the different genetic background may confers to the difference; (2) The living habits are different between North and South of China, since IS is a complex disease affected by both genetic and environment, the complex interaction of different environmental risk factors with SNPs may explain the difference; (3) Some population based case–control studies with limited sample size may lack of power to detect associations with alleles with a small effect. Although the results remain controversial, our results provide additionally evidence for the association between rs11833579 and IS with relatively lower false positive rate.
In addition, our study demonstrated that rs2230501 in PRKCH gene had significant association with IS. Protein kinase C mediates a wide variety of signaling pathways [18] and involves in the induction of inducible nitric oxide synthase (iNOS) which lead to vascular endothelial dysfunction [19]. Moreover, it also plays an important role in the development of atherosclerotic diseases [5]. To our knowledge, this is the first study to replicate the association between rs2230501 and IS. Another SNP rs2230500, located near and almost in absolute linkage disequilibrium (LD) with rs2230501 (D′ = 0.99), is the most frequently studied SNP in PRKCH gene. A large-scale genetic epidemiological study [5] in Japanese subjects first showed that a nonsynonymous SNP rs2230500 in the PRKCH gene with cerebral infarction. Chinese researchers also demonstrated that rs2230500 was significantly associated with IS (OR 1.31; 95 % CI 1.08–1.60; P = 0.0058) in a dominant model. After age and sex adjustment, the associations remained significant (OR 1.37, 95 % CI 1.12–1.67, P = 0.0019) [20]. Our study showed the heterozygote of rs2230501, which is in absolute LD with rs2230500, could increase the risk of IS compared with wild homozygote. More studies are still need to confirm this association with larger sample size and higher statistical power in Chinese Han population.
In addition, our study found that smoking could increase the risk of IS together with rs11833579. It is known that smoking affects cell-mediated immune responses, causes oxidative damage and arterial endothelial dysfunction [21, 22]. Ninjurin2 is a hemophilic adhesion molecule, which is nerve injury-induced and expressed in many tissues including peripheral nerves [13]. Although the independent role of smoke and NINJ2 gene is relatively clear, the mechanism involved their joint effect on IS is unknown. It is possible that NINJ2 affects IS by influencing the reaction to brain cells to injury, which might be modified by the oxidative damage or inflammation due to smoke. More replicable studies based on large population are needed to confirm this result and reveal the underlying mechanism of the interaction.
There are several limitations in our study. First, the sample size is relatively small, since it is difficult to recruit IS patients together with their discordant siblings. One of the largest family-based IS studies in the western countries is siblings with ischemic stroke study (SWISS), which recruited 223 probands and 84 stroke-unaffected siblings. Although our sample size is not as large as some population-based case control studies, it is larger than most IS family-based studies. Second, associations of SNPs with subtypes of IS were not examined in the present investigation due to the limited sample size. Thus, studies are needed to examine the association of NINJ2 gene variation in different IS subtypes in the future so as to provide further evidence for the pathogenic mechanisms of IS.
In conclusion, we confirmed that NINJ2 genetic variants were related to risk of IS in the northern Chinese population, and found the interaction between rs11833579 and smoking. Further research is needed to confirm this interaction so that the pathogenic mechanisms of IS can be featured and intervened.
References
Bonita R, Mendis S, Truelsen T, Bogousslavsky J, Toole J, Yatsu F (2004) The global stroke initiative. Lancet Neurol 3(7):391–393
Wang Y, Cui L, Ji X et al (2011) The China National Stroke Registry for patients with acute cerebrovascular events: design, rationale, and baseline patient characteristics. Int J Stroke 6(4):355–361
Gretarsdottir S, Thorleifsson G, Reynisdottir ST et al (2003) The gene encoding phosphodiesterase 4D confers risk of ischemic stroke. Nat Genet 35(2):131–138
Helgadottir A, Manolescu A, Thorleifsson G et al (2004) The gene encoding 5-lipoxygenase activating protein confers risk of myocardial infarction and stroke. Nat Genet 36(3):233–239
Kubo M, Hata J, Ninomiya T et al (2007) A nonsynonymous SNP in PRKCH (protein kinase C η) increases the risk of cerebral infarction. Nat Genet 39(2):212–217
Alanne M, Kristiansson K, Auro K et al (2007) Variation in the selenoprotein S gene locus is associated with coronary heart disease and ischemic stroke in two independent Finnish cohorts. Hum Genet 122(3–4):355–365
Gschwendtner A, Bevan S, Cole JW et al (2009) Sequence variants on chromosome 9p21. 3 confer risk for atherosclerotic stroke. Ann Neurol 65(5):531–539
Ikram MA, Seshadri S, Bis JC et al (2009) Genomewide association studies of stroke. N Engl J Med 360(17):1718–1728
Iribarren C, Darbinian J, Klatsky AL, Friedman GD (2004) Cohort study of exposure to environmental tobacco smoke and risk of first ischemic stroke and transient ischemic attack. Neuroepidemiology 23(1–2):38–44
Bazzano LA, Gu D, Reynolds K et al (2007) Alcohol consumption and risk for stroke among Chinese men. Ann Neurol 62(6):569–578
Tang X, Hu Y, Chen D, Zhan S, Zhang Z, Dou H (2007) The Fangshan/family-based ischemic stroke study in China (FISSIC) protocol. BMC Med Genet 8(1):60
Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J, Zeng Z, Wu Y (2001) Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, part I: morbidity and mortality monitoring. Circulation 103(3):462–468
Araki T, Milbrandt J (2000) Ninjurin2, a novel homophilic adhesion molecule, is expressed in mature sensory and enteric neurons and promotes neurite outgrowth. J Neurosci 20(1):187–195
Matsushita T, Umeno J, Hirakawa Y et al (2010) Association study of the polymorphisms on chromosome 12p13 with atherothrombotic stroke in the Japanese population. J Hum Genet 55(7):473–476
Tong Y, Zhang Y, Zhang R et al (2011) Association between two key SNPs on chromosome 12p13 and ischemic stroke in Chinese Han population. Pharmacogenet Genomics 21(9):572–578
Ding H, Tu X, Xu Y et al (2011) No evidence for association of 12p13 SNPs rs11833579 and rs12425791 within NINJ2 gene with ischemic stroke in Chinese Han population. Atherosclerosis 216(2):381–382
Wang X, Zhang J, Liu Y, Zhang Y (2011) Relationship between nerve injury-induced protein gene 2 polymorphism and stroke in Chinese Han population. J Biomed Res 25(4):287–291
Nishizuka Y (1995) Protein kinase C and lipid signaling for sustained cellular responses. FASEB J 9(7):484–496
Pham TN, Brown BL, Dobson PR, Richardson VJ (2003) Protein kinase C-eta (PKC-η) is required for the development of inducible nitric oxide synthase (iNOS) positive phenotype in human monocytic cells. Nitric Oxide 9(3):123–134
Wu L, Shen Y, Liu X et al (2009) The 1425G/A SNP in PRKCH is associated with ischemic stroke and cerebral hemorrhage in a Chinese population. Stroke 40(9):2973–2976
Rius C, Company C, Piqueras L et al (2013) Critical role of fractalkine (CX3CL1) in cigarette smoke-induced mononuclear cell adhesion to the arterial endothelium. Thorax 68(2):177–186
Ambrose JA, Barua RS (2004) The pathophysiology of cigarette smoking and cardiovascular disease. An update. J Am Coll Cardiol 43(10):1731–1737
Acknowledgments
We thank the population and the local health and government authorities in Fangshan district for their help. This study is supported by National Natural Science Foundation of China (81230066, 30872173, 81102177, 81172744).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yanping Zhu and Kuo Liu have contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Zhu, Y., Liu, K., Tang, X. et al. Association between NINJ2 gene polymorphisms and ischemic stroke: a family-based case–control study. J Thromb Thrombolysis 38, 470–476 (2014). https://doi.org/10.1007/s11239-014-1065-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-014-1065-6