Abstract
Patients with liver cirrhosis often exhibit sleep–wake abnormalities, which are, at least to some extent, circadian in origin. A relatively novel non-pharmacological approach to circadian disruption is appropriately timed bright light therapy. The aims of this pilot study were to investigate sleep–wake characteristics of a well-characterized population of inpatients with cirrhosis, and to evaluate the efficacy of bright light therapy in the hospital setting. Twelve consecutive inpatients with cirrhosis underwent complete sleep–wake assessment, to include qualitative and semi-quantitative (actigraphic) indices of night-time sleep quality, daytime sleepiness, diurnal preference, habitual sleep timing, quality of life, mood and circadian rhythmicity [i.e. urine collections for measurement of the melatonin metabolite 6-sulphatoxymelatonin (aMT6s)]. Patients showed extremely impaired night sleep quality (Pittsburg Sleep Quality Index global score: 16.3 ± 2.1) and daytime sleepiness was common (Epworth Sleepiness Scale: 8.3 ± 3.2). Five patients were randomly assigned to a single room in which lighting was controlled in relation to timing, spectral composition and intensity (lights on at 06:30 and off at 22:30, blue-enriched, more intense light in the morning, red-enriched, less intense light in the afternoon/evening); the others stayed in identical rooms with standard lighting. Sleep diaries revealed poor sleep quality, prolonged sleep latency (67 ± 138 min) and a reduced sleep efficiency (69 ± 21 %). These features were confirmed by actigraphy (sleep efficiency: 71 ± 13 %; fragmentation index: 55 ± 15 %). Quality of life was globally impaired, and mood moderately depressed (Beck Depression Inventory: 19.4 ± 7.9). Seven patients underwent serial urine collections: no circadian aMT6s rhythm was detected in any of them, neither at baseline, nor during the course of hospitalization in either room (n = 4). In conclusion, sleep and circadian rhythms in hospitalized, decompensated patients with cirrhosis are extremely compromised. Treatment with bright light therapy did not show obvious, beneficial effects, most likely in relation to the severity of disturbance at baseline.

Similar content being viewed by others
References
Cordoba J, Cabrera J, Lataif L, Penev P, Zee P, Blei AT (1998) High prevalence of sleep disturbance in cirrhosis. Hepatology 27(2):339–345
Hourmand-Ollivier I, Piquet MA, Toudic JP, Denise P, Dao T (2006) Actigraphy: a new diagnostic tool for hepatic encephalopathy. World J Gastroenterol 12(14):2243–2244
Cordoba J, Steindl P, Blei AT (2009) Melatonin arrhythmia is corrected after liver transplantation. Am J Gastroenterol 104(7):1862–1863. doi:10.1038/ajg.2009.171
Borbely AA (1982) A two process model of sleep regulation. Hum Neurobiol 1(3):195–204
Steindl PE, Finn B, Bendok B, Rothke S, Zee PC, Blei AT (1995) Disruption of the diurnal rhythm of plasma melatonin in cirrhosis. Ann Intern Med 123(4):274–277
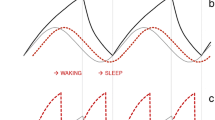
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY (2010) On the origin and the consequences of circadian abnormalities in patients with cirrhosis. Am J Gastroenterol 105(8):1773–1781. doi:10.1038/ajg.2010.86
Montagnese S, De Pittà C, De Rui M, Corrias M, Turco M, Merkel C, Amodio P, Costa R, Skene DJ, Gatta A (2014) Sleep–wake abnormalities in patients with cirrhosis. Hepatology 59(2):705–712. doi:10.1002/hep.26555
Weitzman ED, Czeisler CA, Coleman RM, Spielman AJ, Zimmerman JC, Dement W, Richardson G, Pollack CP (1981) Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia. Arch Gen Psychiatry 38(7):737–746
Thorpy MJ, Korman E, Spielman AJ, Glovinsky PB (1988) Delayed sleep phase syndrome in adolescents. J Adolesc Health Care 9(1):22–27
Ross JK, Arendt J, Horne J, Haston W (1995) Night-shift work in Antarctica: sleep characteristics and bright light treatment. Physiol Behav 57(6):1169–1174
Czeisler CA, Johnson MP, Duffy JF, Brown EN, Ronda JM, Kronauer RE (1990) Exposure to bright light and darkness to treat physiologic maladaptation to night work. N Engl J Med 322(18):1253–1259
Arendt J (2009) Managing jet lag: some of the problems and possible new solutions. Sleep Med Rev 13(4):249–256. doi:10.1016/j.smrv.2008.07.011
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY (2009) Sleep and circadian abnormalities in patients with cirrhosis: features of delayed sleep phase syndrome? Metab Brain Dis 24(3):427–439. doi:10.1007/s11011-009-9146-5
Lucas RJ, Peirson SN, Berson DM, Brown TM, Cooper HM, Czeisler CA, Figueiro MG, Gamlin PD, Lockley SW, O’Hagan JB, Price LL, Provencio I, Skene DJ, Brainard GC (2014) Measuring and using light in the melanopsin age. Trends Neurosci 37(1):1–9. doi:10.1016/j.tins.2013.10.004
Revell VL, Arendt J, Terman M, Skene DJ (2005) Short-wavelength sensitivity of the human circadian system to phase-advancing light. J Biol Rhythms 20(3):270–272
Francis G, Bishop L, Luke C, Middleton B, Williams P, Arendt J (2008) Sleep during the Antarctic winter: preliminary observations on changing the spectral composition of artificial light. J Sleep Res 17(3):354–360. doi:10.1111/j.1365-2869.2008.00664.x
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R (1973) Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 60(8):646–649
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR (2001) A model to predict survival in patients with end-stage liver disease. Hepatology 33(2):464–470
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Montagnese S, Middleton B, Skene DJ, Morgan MY (2009) Sleep–wake patterns in patients with cirrhosis: all you need to know on a single sheet. A simple sleep questionnaire for clinical use. J Hepatol 51(4):690–695. doi:10.1016/j.jhep.2009.06.006
Arendt J, Middleton B, Williams P, Francis G, Luke C (2006) Sleep and circadian phase in a ship’s crew. J Biol Rhythms 21(3):214–221
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Akerstedt T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52(1–2):29–37
Horne JA, Ostberg O (1976) A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 4(2):97–110
Lockley SW, Skene DJ, Arendt J (1999) Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res 8(3):175–183
Ware JE Jr (1992) Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Apolone G, Mosconi P, Ware JE Jr. (1997) Questionario sullo stato di salute SF-36: manuale d’uso e guida all’interpretazione dei risultati Guerini e associati
Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D (1999) Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut 45(2):295–300
Rucci P, Taliani G, Cirrincione L, Alberti A, Bartolozzi D, Caporaso N et al (2005) Validity and reliability of the Italian version of the Chronic Liver Disease Questionnaire (CLDQ-I) for the assessment of health-related quality of life. Dig Liver Dis 37(11):850–860
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
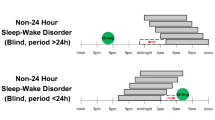
Lockley SW, Skene DJ, James K, Thapan K, Wright J, Arendt J (2000) Melatonin administration can entrain the free-running circadian system of blind subjects. J Endocrinol 164(1):R1–R6
Aldhous ME, Arendt J (1988) Radioimmunoassay for 6-sulphatoxymelatonin in urine using an iodinated tracer. Ann Clin Biochem 25(Pt 3):298–303
Minors DS, Waterhouse JM (1988) Mathematical and statistical analysis of circadian rhythms. Psychoneuroendocrinology 13(6):443–464
Lockley SW, Skene DJ, Tabandeh H, Bird AC, Defrance R, Arendt J (1997) Relationship between napping and melatonin in the blind. J Biol Rhythms 12(1):16–25
Montagnese S, Middleton B, Skene DJ, Morgan MY (2009) Night-time sleep disturbance does not correlate with neuropsychiatric impairment in patients with cirrhosis. Liver Int 29(9):1372–1382. doi:10.1111/j.1478-3231.2009.02089.x
Marchesini G, Bianchi G, Amodio P, Salerno F, Merli M, Panella C et al (2001) Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology 120(1):170–178
Samanta J, Dhiman RK, Khatri A, Thumburu KK, Grover S, Duseja A et al (2013) Correlation between degree and quality of sleep disturbance and the level of neuropsychiatric impairment in patients with liver cirrhosis. Metab Brain Dis 28(2):249–259. doi:10.1007/s11011-013-9393-3
Bianchi G, Marchesini G, Nicolino F, Graziani R, Sgarbi D, Loguercio C et al (2005) Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis 37(8):593–600
Chojnacki C, Walecka-Kapica E, Klupinska G, Wachowska-Kelly P, Zylinska K, Winczyk K et al (2012) Serotonin and melatonin secretion and metabolism in patients with liver cirrhosis. Pol Arch Med Wewn 122(9):392–397
Montagnese S, Middleton B, Mani AR, Skene DJ, Morgan MY (2011) Changes in the 24-h plasma cortisol rhythm in patients with cirrhosis. J Hepatol 54(3):588–590. doi:10.1016/j.jhep.2010.08.015
De Rui M, Gaiani S, Middleton B, Skene DJ, Schiff S, Gatta A, Merkel C, Amodio P, Montagnese S (2011) Bright times for patients with cirrhosis and delayed sleep habits: a case report on the beneficial effect of light therapy. Am J Gastroenterol 106(11):2048–2049. doi:10.1038/ajg.2011.239
Wakamura T, Tokura H (2001) Influence of bright light during daytime on sleep parameters in hospitalized elderly patients. J Physiol Anthropol Appl Human Sci 20(6):345–351
Yamadera H, Ito T, Suzuki H, Asayama K, Ito R, Endo S (2000) Effects of bright light on cognitive and sleep–wake (circadian) rhythm disturbances in Alzheimer-type dementia. Psychiatry Clin Neurosci 54(3):352–353
Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ (2008) Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 299(22):2642–2655. doi:10.1001/jama.299.22.2642
Gogenur I, Ocak U, Altunpinar O, Middleton B, Skene DJ, Rosenberg J (2007) Disturbances in melatonin, cortisol and core body temperature rhythms after major surgery. World J Surg 31(2):290–298
Acknowledgments
This work was part-funded by a grant from the Italian Ministry of Health to MS (Giovani Ricercatori 2009); Stockgrand Ltd. (UK) undertook the urinary 6-sulphatoxymelatonin assays; Derungs-Waldmann Illuminotecnica (Italy) provided the lighting equipment; DJS is a Royal Society Wolfson Research Merit Award holder.
Conflict of interest
Prof. Debra Skene and Dr. Benita Middleton are co-directors of Stockgrand Ltd.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special Issue: In Honor of Michael Norenberg.
Rights and permissions
About this article
Cite this article
De Rui, M., Middleton, B., Sticca, A. et al. Sleep and Circadian Rhythms in Hospitalized Patients with Decompensated Cirrhosis: Effect of Light Therapy. Neurochem Res 40, 284–292 (2015). https://doi.org/10.1007/s11064-014-1414-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-014-1414-z