Abstract
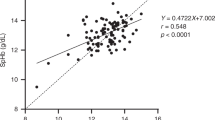
Objective Iron deficiency is the most prevalent micronutrient deficiency worldwide and a common medical condition in the United States. The American Academy of Pediatrics has recommended universal screening for iron deficiency anemia in infants at approximately 1 year of age. This screening involves invasive venous blood sampling which increases the clinic visit time and may cause significant stress to the patient and family members. The purpose of this study was to assess the accuracy and utility of a non-invasive hemoglobin measurement device compared to standard laboratory hemoglobin measurement from venipuncture. Methods One hundred ten children were enrolled in the study following a well-child examination at San Antonio Military Medical Center from June 2012 to June 2014. Each child had a hemoglobin measurement obtained with the Masimo Pronto with Rainbow® R20L disposable sensor followed by venipuncture that was sent to the clinical laboratory for hemoglobin measurement. Paired hemoglobin results from the non-invasive device and the clinical laboratory were compared. Results Ninety-seven children successfully had hemoglobin measured by the Masimo Pronto device. Hemoglobin values obtained with the Masimo Pronto were significantly correlated with venous hemoglobin levels, with a correlation coefficient of 0.48. A hemoglobin level less than 11.5 gm/dL on the Masimo Pronto had a sensitivity of 82 % and a negative predictive value of 95 % when compared to venous hemoglobin level less than 11 gm/dL. Conclusions for Practice Non-invasive hemoglobin testing with the Masimo Pronto device may be a useful screening tool for anemia in infants that avoids invasive testing.

Similar content being viewed by others
References
Baker, R. D., Greer, F. R., & Committee on Nutrition American Academy of Pediatrics. (2010). Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics, 126(5), 1040–1050.
Eden, A. N., & Sandoval, C. (2012). Iron deficiency in infants and toddlers in the United States. Pediatric Hematology and Oncology, 29(8), 704–709.
de Benoist, B., McLean, E., Egli, I. et al. (2008). Worldwide prevalence of anaemia 1993–2005 WHO Global Database on Anaemia. http://www.who.int/vmnis/publications/anaemia_prevalence/en/. Accessed July 29 2014.
Lozoff, B., Beard, J., Connor, J., et al. (2006). Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutrition Reviews, 64(5 Pt 2), S34–S43.
Carter, R. C., Jacobson, J. L., Burden, M. J., et al. (2010). Iron deficiency anemia and cognitive function in infancy. Pediatrics, 126(2), e427–e434.
Congdon, E. L., Westerlund, A., Algarin, C. R., et al. (2012). Iron deficiency in infancy is associated with altered neural correlates of recognition memory at 10 years. Journal of Pediatrics, 160(6), 1027–1033.
Shah, N., Osea, E. A., & Martinez, G. J. (2014). Accuracy of noninvasive hemoglobin and invasive point-of-care hemoglobin testing compared with a laboratory analyzer. The International Journal of Laboratory Hematology, 36(1), 56–61.
Gehring, H., Hornberger, C., Dibbelt, L., et al. (2002). Accuracy of point-of-care-testing (POCT) for determining hemoglobin concentrations. Acta Anaesthesiologica Scandinavica, 46(8), 980–986.
Jung, Y. H., Lee, J., Kim, H. S., et al. (2013). The efficacy of noninvasive hemoglobin measurement by pulse CO-oximetry in neonates. Pediatric Critical Care Medicine, 14(1), 70–73.
Lian, Q., Li, H., Zeng, R., et al. (2005). The use of a noninvasive hemoglobin monitor for determining fluid distribution and elimination in pediatric patients undergoing minor surgery [published online ahead of print February 19, 2014]. The Journal of Clinical Monitoring and Computing. doi:10.1007/s10877-014-9566-6.
Park, Y. H., Lee, J. H., Song, H. G., et al. (2012). The accuracy of noninvasive hemoglobin monitoring using the radical-7 pulse CO-Oximeter in children undergoing neurosurgery. Anesthesia and Analgesia, 115(6), 1302–1307.
Amano, I., & Murakami, A. (2013). Use of non-invasive total hemoglobin measurement as a screening tool for anemia in children. Pediatrics International, 55(6), 803–805.
Stavinoha, A., Modem, V., & Quigley, R. (2013). Using noninvasive hemoglobin measurements to estimate measured hemoglobin in a pediatric hemodialysis unit. Hemodialysis International, 17(suppl 1), S7–S10.
Spielmann, N., Mauch, J., Madjdpour, C., et al. (2012). Accuracy and precision of hemoglobin point-of-care testing during major pediatric surgery. International Journal of Laboratory Hematology, 34(1), 86–90.
Kim, S. H., Lilot, M., Murphy, L. S., et al. (2014). Accuracy of continuous noninvasive hemoglobin monitoring: A systematic review and meta-analysis. Anesthesia and Analgesia, 119(2), 332–346.
Knutson, T., Della-Giustina, D., Tomich, E., et al. (2013). Evaluation of a new nonnvasive device in determining hemoglobin levels in emergency department patients. The Western Journal of Emergency Medicine, 14(3), 283–286.
Vidyarthi, A.R., Hamill, T., Green, A.L., et al. (2014). Changing resident test ordering behavior: A multilevel intervention to decrease laboratory utilization at an academic medical center [published online ahead of print January 17, 2014]. American Journal of Medical Quality. doi:10.1177/1062860613517502.
Biondich, P. G., Downs, S. M., Carroll, A. E., et al. (2006). Shortcomings in infant iron deficiency screening methods. Pediatrics, 117(2), 290–294.
Funding
Internal funding through Department of Clinical Investigation, Wilford Hall Ambulatory Surgical Center. The funding source purchased equipment utilized in the study. The funding source had no role in the study design, in the collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Disclosures
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army and Department of Defense or the U.S. Government.
Rights and permissions
About this article
Cite this article
Hsu, D.P., French, A.J., Madson, S.L. et al. Evaluation of a Noninvasive Hemoglobin Measurement Device to Screen for Anemia in Infancy. Matern Child Health J 20, 827–832 (2016). https://doi.org/10.1007/s10995-015-1913-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1913-9