Abstract
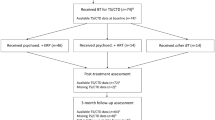
Tourette disorder is characterized by tics and is generally associated with many life impairments in childhood. International clinical guidelines recommend treatment with pharmacotherapy and behaviour therapy. The current pilot study reports a single-case design study assessing the effectiveness of an innovative cognitive-behavioural and physiological treatment for decreasing tics in children and adolescents. Fourteen participants aged 8–16 years old were recruited as consecutive referrals from the general population. Eleven cases completed a cognitive-psychophysiological treatment (CoPs) adapted for children and adolescents, and 5 children completed 6- and 12-months follow-up. The CoPs treatment lasted 14–16 sessions and covered 10 major steps principally addressing processes leading up to tics rather than the tics themselves. There was a significant decrease in tic severity as measured by the Tourette Symptom Global Scale overall children. Results showed a decrease of at least one standard deviation at follow-up time measurements and the majority of children showed a further decrease in tic severity at 12-months follow-up. In conclusion, the cognitive psychophysiological treatment reduced severity of tics in children and adolescents as well as in adults (O’Connor, 2015). These findings highlight the necessity for a therapeutic approach which focuses on the central and global processes surrounding tics to help symptom reduction in people with Tourette.

Similar content being viewed by others
Notes
Contact the authors to obtain a copy of the current version of the CoPs treatment adapted for children.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
Azrin, N. H., & Nunn, R. G. (1973). Habit-reversal: a method of eliminating nervous habits and tics. Behaviour Research and Therapy, 11(4), 619–628.
Azrin, N. H., & Peterson, A. L. (1989). Reduction of an eye tic by controlled blinking. Behavior Therapy, 20(3), 467–473.
Bellavance, J. (2010). Évaluation des effets d’un programme d’entraînement à l’autogestion des tics sur le fonctionnement social d’adolescents atteints du syndrome de Gilles de la Tourette. http://www.svs.ulaval.ca/index.php?pid=651etall=1etid=3888.
Budman, C. L., & Feirman, L. (2001). The relationship of Tourette’s syndrome with its psychiatric comorbidities: is there an overlap? Psychiatric Annals, 31, 541–548.
Carr, J. E., & Chong, I. M. (2005). Habit reversal treatment of tic disorders: a methodological critique of the literature. Behavior Modification, 29(6), 858–875.
Cavanna, A. E., David, K., Bandera, V., Termine, C., Balottin, U., Schrag, A., et al. (2013). Health-related quality of life in Gilles de la Tourette syndrome: a decade of research. Behavioural Neurology, 27(1), 83–93.
Cutler, D., Murphy, T., Gilmour, J., & Heyman, I. (2009). The quality of life of young people with Tourette syndrome. Child: Care, Health and Development, 35(4), 496–504.
Deckersbach, T., Rauch, S., Buhlmann, U., & Wilhelm, S. (2006). Habit reversal versus supportive psychotherapy in Tourette’s disorder: a randomized controlled trial and predictors of treatment response. Behaviour Research and Therapy, 44(8), 1079–1090.
Diamond, G., & Josephson, A. (2005). Family-based treatment research: a 10-year update. Journal of the American Academy of Child and Adolescent Psychiatry, 44(9), 872–887.
Dutta, N., & Cavanna, A. E. (2013). The effectiveness of habit reversal therapy in the treatment of Tourette syndrome and other chronic tic disorders: a systematic review. Functional Neurology, 28(1), 7–12.
Eddy, C. M., Rizzo, R., Gulisano, M., Agodi, A., Barchitta, M., Calì, P., et al. (2011). Quality of life in young people with Tourette syndrome: a controlled study. Journal of Neurology, 258(2), 291–301.
Freeman, R., Fast, D., Burd, L., Kerbeshian, J., Robertson, M., & Sandor, P. (2000). An international perspective on Tourette syndrome: selected findings from 3500 cases in 22 countries. Developmental Medicine and Child Neurology, 42, 436–447.
Greene, R. W., Ablon, J. S., & Goring, J. C. (2003). A transactional model of oppositional behavior: underpinnings of the collaborative problem solving approach. Journal of Psychosomatic Research, 55(1), 67–75.
Harcherik, D. F., Leckman, J. F., Detlor, J., & Cohen, D. J. (1984). A new instrument for clinical studies of Tourette’s syndrome. Journal of the American Academy of Child Psychiatry, 23(2), 153–160.
Himle, M. B., Capriotti, M. R., Hayes, L. P., Ramanujam, K., Scahill, L., Sukhodolsky, D. G., et al. (2014). Variables associated with tic exacerbation in children with chronic tic disorders. Behavior Modification, 38(2), 163–183.
Hjördis, O. A., Gyllenberg, D., Langridge, A., Sandin, S., Hansen, S. N., Leonard, H., et al. (2015). The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. European Child and Adolescent Psychiatry, 24, 173–183.
Hoogduin, K., Verdellen, C., & Cath, D. (1997). Exposure and response prevention in the treatment of Gilles de la Tourette’s syndrome: four case studies. Clinical Psychology and Psychotherapy, 4(2), 125–135.
Hwang, G. C., Tillberg, C. S., & Scahill, L. (2012). Habit reversal training for children with Tourette syndrome: update and review. Journal of Child and Adolescent Psychiatric Nursing, 25, 178–183.
Knight, T., Steeves, T., Day, L., Lowerison, M., Jette, N., & Pringsheim, T. (2012). Prevalence of tic disorders: a systematic review and meta-analysis. Pediatric Neurology, 47(2), 77–90.
Lavoie, M. E., Imbriglio, T. V., Stip, E., & O’Connor, K. P. (2011). Neurocognitive changes following cognitive-behavioral treatment in Tourette syndrome and chronic tic disorder. International Journal of Cognitive Therapy, 4(1), 34–50.
Leclerc, J., O’Connor, K., Forget, J., & Lavoie, M. (2012). Évaluation de l’effet d’un programme d’entraînement à l’autogestion des épisodes explosifs chez des enfants atteints du syndrome de Gilles de la Tourette. Pratiques Psychologiques, 18(3), 221–224.
Liu, S., Zheng, L., Zheng, X., Zhang, X., Yi, M., & Ma, X. (2014). The subjective quality of life in young people with Tourette syndrome in China. Journal of Attention Disorders. doi:10.1177/1087054713518822.
McGuire, J. F., Arnold, E., Park, J. M., Nadeau, J. M., Lewin, A. B., Murphy, T. K., et al. (2015). Living with tics: reduced impairment and improved quality of life for youth with chronic tic disorders. Psychiatry Research, 225(3), 571–579.
Morand-Beaulieu, S. M., O’Connor, K. P., Sauvé, G., Blanchet, P. J., & Lavoie, M. E. (2015). Cognitive-behavioural therapy induces sensorimotor and specific electrocortical changes in chronic tic and Tourette’s disorder. Neuropsychologia. doi:10.1016/j.neuropsychologia.2015.05.024.
Mueser, K. T., Yarnold, P. R., & Foy, D. W. (1991). Statistical analysis for single-case designs: evaluating outcome of imaginal exposure treatment of chronic PTSD. Behavior Modification, 15, 132–155.
Murphy, T. K., Lewin, A. B., Storch, E. A., Stock, S., & the American Academy of Child and Adolescent Psychiatry Committee on Quality Issues (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 52(12), 1341–1359.
O’Connor, K. (2002). A cognitive-behavioral/psychophysiological model of tic disorders. Behaviour Research and Therapy, 40(10), 1113–1142.
O’Connor, K. (2005). Cognitive-behavioral management of tic disorders. New York: John Wiley & Sons Ltd..
O’Connor, K. P., Gareau, D., & Blowers, G. (1993). Change in construals of tic producing situations following cognitive and behavioral therapy. Perceptual Motor Skills, 77, 776–778.
O’Connor, K. P., Brault, M., Robillard, S., Loiselle, J., Borgeat, F., & Stip, E. (2001). Evaluation of a cognitive-behavioural program for the management of chronic tic and habit disorders. Behaviour Research and Therapy, 39(6), 667–681.
O’Connor, K. P., Lavoie, M. E., Stip, E., Borgeat, F., & Laverdure, A. (2008). Cognitive-behaviour therapy and skilled motor performance in adults with chronic tic disorder. Neuropsychological Rehabilitation, 18(1), 45–64.
O’Connor, K. P., Laverdure, A., Taillon, A., Stip, E., Borgeat, F., & Lavoie, M. (2009). Cognitive behavioral management of Tourette’s syndrome and chronic tic disorder in medicated and unmedicated samples. Behaviour Research and Therapy, 47(12), 1090–1095.
O’Connor, K. P., St-Pierre-Delorme, M. E., Leclerc, J., Lavoie, M. E., & Blais, M. T. (2014). Meta-cognitions in Tourette, tics and body focused repetitive disorders. The Canadian Journal of Psychiatry, 59(8), 417–425.
O’Connor, K. P., Lavoie, M. E., Blanchet, P., & St-Pierre-Delorme, M.-E. (2015). Evaluation of a cognitive psychophysiological model for management of tic disorders: an open trial. The British Journal of Psychiatry (Epub ahead of print). doi:10.1192/bjp.bp.114.154518.
Ouellette, S., Leclerc, J., Bellavance, J., O’Connor, K., Bombardier, M., & Nolin, J. G. (2013). The effects of a training program for self-management of tics on the social functioning of adolescents with Tourette syndrome. Marrakech: European Association for Behavioural and Cognitive Therapies (EABCT) Congress.
Piacentini, J., Woods, D. W., Scahill, L., Wilhelm, S., Peterson, A. L., Chang, S., et al. (2010). Behavior therapy for children with Tourette disorder: a randomized controlled trial. Journal of the American Medical Association, 303(19), 1929–1937.
Pringsheim, T., Doja, A., Gorman, D., McKinlay, D., Day, L., Billinghurst, L., et al. (2012). Canadian guidelines for the evidence-based treatment of tic disorders: pharmacotherapy. Canadian Journal of Psychiatry, 57(3), 133–143.
Robertson, M. M. (2000). Tourette syndrome, associated conditions and complexities of treatment. Brain, 123, 425–462.
Scahill, L., Erenberg, G., Berlin, C. M., Budman, C., Coffey, B. J., Jankovic, J., et al. (2006). Contemporary assessment and pharmacotherapy of Tourette syndrome. NeuroRx, 3(2), 192–206.
Specht, M. W., Woods, D. W., Nicotra, C. M., Kelly, L. M., Ricketts, E. J., Conelea, C. A., et al. (2013). Effects of tic suppression: ability to suppress, rebound, negative reinforcement, and habituation to the premonitory urge. Behaviour Research and Therapy, 51, 24–30.
Steeves, T., McKinlay, B. D., Gorman, D., Billinghurst, L., Day, L., Carroll, A., et al. (2012). Canadian guidelines for the evidence-based treatment of tic disorders: behavioural therapy, deep brain stimulation, and transcranial magnetic stimulation. Canadian Journal of Psychiatry, 57(3), 144–151.
Storch, E. A., Lack, C. W., Simons, L. E., Goodman, W. K., Murphy, T. K., & Geffken, G. R. (2007a). A measure of functional impairment in youth with Tourette’s syndrome. Journal of Pediatric Psychology, 32, 950–959.
Storch, E. A., Murphy, T. K., Chase, R. M., Keeley, M., Goodman, W. K., Murray, M., et al. (2007b). Peer victimization in youth with Tourette’s syndrome and chronic tic disorder: relations with tic severity and internalizing symptoms. Journal of Psychopathology and Behavioral Assessment, 29(4), 211–219.
Storch, E. A., Hanks, C. E., Mink, J. W., McGuire, J. F., Adams, H. R., Augustine, E. F., et al. (2015). Suicidal thoughts and behaviors in children and adolescents with chronic tic disorders. Depression and Anxiety, 32(10), 744–753.
Thibault, G., O’Connor, K. P., Stip, E., & Lavoie, M. E. (2009). Electrophysiological manifestations of stimulus evaluation, response inhibition and motor processing in Tourette syndrome patients. Psychiatry Research, 167(3), 202–220.
Van de Griendt, J. M. T. M., Verdellen, C. W. J., van Dijk, M. K., & Verbraak, M. J. P. M. (2013). Behavioural treatment of tics: habit reversal and exposure with response prevention. Neuroscience and Biobehavioral Reviews, 37(6), 1172–1177.
Verdellen, C. W., Keijsers, G. P., Cath, D. C., & Hoogduin, C. A. (2004). Exposure with response prevention versus habit reversal in Tourettes’s syndrome: a controlled study. Behaviour Research and Therapy, 42(5), 501–511.
Verdellen, C., van de Griendt, J., Hartmann, A., Murphy, T., & Guidelines Group, E. S. S. T. S. (2011). European clinical guidelines for Tourette syndrome and other tic disorders. Part III: behavioural and psychosocial interventions. European Child and Adolescent Psychiatry, 20(4), 197–207.
Wadman, R., Tischler, V., & Jackson, G. M. (2013). "everybody just thinks I’m weird": a qualitative exploration of the psychosocial experiences of adolescents with Tourette syndrome. Child: Care, Health and Development, 6, 880–886.
Wolpe, J. (1958). Psychotherapy by reciprocal inhibition. Stanford: Stanford University Press.
Woods, D. W., & Miltenber, R. G. (2001). Tic disorders, trichotillomania, and other repetitive behavior disorders. Behavioral approaches to analysis and treatment. Boston: Kluwer Academic Publishers.
Woods, D. W., & Miltenberger, R. G. (1995). Habit reversal: a review of applications and variations. Journal of Behavior Therapy and Experimental Psychiatry, 26(2), 123–131.
Woods, D. W., Piacentini, J. C., Scahill, L., Peterson, A. L., Wilhelm, S., Chang, S., et al. (2011). Behavior therapy for tics in children: acute and long-term effects on psychiatric and psychosocial functioning. Journal of Child Neurology, 26(7), 858–865.
Acknowledgments
This study was funded by a research grant from the “Fonds de recherche en santé du Québec” (Research group #20573): “Regroupement multidisciplinaire de la recherche clinique sur le spectre du trouble obsessionnel compulsif; 2010-2014”. The authors would like to acknowledge the Obsessive–Compulsive Disorder and Tic Disorder Studies Centre team for their participation with assessment and treatment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethic Approval
All procedures performed in this study involving human participants were approved by the ethical committee of the “Institut universitaire en santé mentale de Montréal” in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all participants and their parents.
Conflict of Interest
Julie B. Leclerc declare that she has no conflict of interest. Philippe Valois declare that he has no conflict of interest. Gabrielle J-Nolin declare that she has no conflict of interest. Mélyane Bombardier declare that she has no conflict of interest. Stéphanie Ouellette declare that she has no conflict of interest. Kieron P. O’Connor declare that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Leclerc, J.B., Valois, P., J-Nolin, G. et al. A Therapy for Tics in Children Managing Underlying Processes: a Pilot Study. J Dev Phys Disabil 28, 581–593 (2016). https://doi.org/10.1007/s10882-016-9496-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-016-9496-y