Abstract
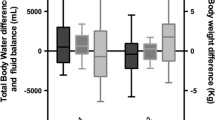
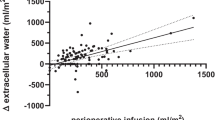
We evaluated the efficacy of bioelectrical impedance analysis (BIA) during the perioperative period by estimating the preoperative and postoperative body fluid status. After obtaining informed consent, we enrolled 100 children (3–12 years of age) scheduled for elective surgeries. All children had been fasted preoperatively. The children’s body fluid status was estimated using a BIA machine (InBody S10; Biospace, Korea) in the ward on the afternoon before surgery (baseline), just before surgery and immediately after surgery. The total administered fluid volume during the fasting period, total administered fluid volume during the operation and fasting time were recorded. Continuous data are shown as mean ± standard deviation, and Pearson’s correlation analysis was used to assess relationships between the preoperative fluid deficit and intracellular water (ICW)/extracellular water (ECW) changes. The mean fasting period was 13.3 h (range 5.8–19.7 h). A weak positive correlation was shown between the ICW and fluid deficit during the fasting period (Pearson correlation coefficient = 0.254; P = 0.010). A stronger positive correlation was shown between the ECW and fluid deficit during the fasting period (Pearson correlation coefficient = 0.359; P < 0.001). The baseline and postoperative ICW showed a strong positive correlation (Pearson correlation coefficient = 0.992, P < 0.001), as did the baseline and postoperative ECW (Pearson correlation coefficient = 0.990, P < 0.001). Also there was no dehydration and irritability on medical recording preoperatively. BIA may be an alternative method for estimating the perioperative fluid status in children and determining details of fluid administration.


Similar content being viewed by others
References
Harvey G, Meir R, Brooks L, Holloway K. The use of body mass changes as a practical measure of dehydration in team sports. J Sci Med Sport. 2008;11(6):600–3.
Armstrong LE. Hydration assessment techniques. Nutr Rev. 2005;63(6 Pt 2):S40–54.
Piccoli A. Bioelectric impedance measurement for fluid status assessment. Contrib Nephrol. 2010;164:143–52.
Grant MM, Kubo WM. Assessing a patient’s hydration status. Am J Nurs. 1975;75(8):1307–11.
Manz F, Wentz A. 24-h hydration status: parameters, epidemiology and recommendations. Eur J Clin Nutr. 2003;57(Suppl 2):S10–8.
Armstrong LE, Pumerantz AC, Fiala KA, Roti MW, Kavouras SA, Casa DJ, Maresh CM. Human hydration indices: acute and longitudinal reference values. Int J Sport Nutr Exerc Metab. 2010;20(2):145–53.
Ship JA, Fischer DJ. The relationship between dehydration and parotid salivary gland function in young and older healthy adults. J Gerontol A Biol Sci Med Sci. 1997;52(5):M310–9.
Smith I, Kranke P, Murat I, Smith A, O’Sullivan G, Soreide E, Spies C, in’t Veld B. European Society of A Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011;28(8):556–69.
Holliday MA, Segar WE, Friedman A, Chesney R, Finberg L. Intravenous fluids for seriously ill children. Lancet. 2004;363(9404):241.
Buffa R, Saragat B, Cabras S, Rinaldi AC, Marini E. Accuracy of specific BIVA for the assessment of body composition in the United States population. PLoS One. 2013;8(3):e58533.
Brooks ER, Fatallah-Shaykh SA, Langman CB, Wolf KM, Price HE. Bioelectric impedance predicts total body water, blood pressure, and heart rate during hemodialysis in children and adolescents. J Ren Nutr. 2008;18(3):304–11.
Shanholtzer BA, Patterson SM. Use of bioelectrical impedance in hydration status assessment: reliability of a new tool in psychophysiology research. Int J Psychophysiol. 2003;49(3):217–26.
Patel RV, Peterson EL, Silverman N, Zarowitz BJ. Estimation of total body and extracellular water in post-coronary artery bypass graft surgical patients using single and multiple frequency bioimpedance. Crit Care Med. 1996;24(11):1824–8.
Warner MA, Caplan RA, Epstein BS, Gibbs CP, Keller CE, Leak JA, Maltby R, Nickinovich DG, Schreiner MS, Weinlander CM. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures—a report by the American Society of Anesthesiologist Task Force on Preoperative Fasting. Anesthesiology. 1999; 90(3):896–905.
Bagci S, Muller N, Muller A, Heydweiller A, Bartmann P, Franz AR. A pilot study of the pleth variability index as an indicator of volume-responsive hypotension in newborn infants during surgery. J Anesth. 2013;27(2):192–8.
Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19(5):823–32.
Utter AC, McAnulty SR, Riha BF, Pratt BA, Grose JM. The validity of multifrequency bioelectrical impedance measures to detect changes in the hydration status of wrestlers during acute dehydration and rehydration. J Strength Cond Res. 2012;26(1):9–15.
Tam RK, Wong H, Plint A, Lepage N, Filler G. Comparison of clinical and biochemical markers of dehydration with the clinical dehydration scale in children: a case comparison trial. BMC Pediatr. 2014;14:149.
Pringle K, Shah SP, Umulisa I, Mark Munyaneza RB, Dushimiyimana JM, Stegmann K, Musavuli J, Ngabitsinze P, Stulac S, Levine AC. Comparing the accuracy of the three popular clinical dehydration scales in children with diarrhea. Int J Emerg Med. 2011;4:58.
Castillo-Zamora C, Castillo-Peralta LA, Nava-Ocampo AA. Randomized trial comparing overnight preoperative fasting period Vs oral administration of apple juice at 06:00-06:30 am in pediatric orthopedic surgical patients. Paediatr Anaesth. 2005;15(8):638–42.
Gorelick MH, Shaw KN, Murphy KO. Validity and reliability of clinical signs in the diagnosis of dehydration in children. Pediatrics. 1997;99(5):E6.
Kawana S, Uzuki M, Nakae Y, Namiki A. Preoperative anxiety and volume and acidity of gastric fluid in children. Paediatr Anaesth. 2000;10(1):17–21.
Mulasi U, Kuchnia AJ, Cole AJ, Earthman CP. Bioimpedance at the bedside: current applications, limitations, and opportunities. Nutr Clin Pract. 2015;30(2):180–93.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C. Composition of the EWG Bioelectrical impedance analysis–part I: review of principles and methods. Clin Nutr. 2004;23(5):1226–43.
Ellis KJ. Human body composition in vivo methods. Physiol Rev. 2000;80(2):649–80.
Acknowledgments
This research was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest, financial or otherwise.
Rights and permissions
About this article
Cite this article
Song, IK., Kim, DH., Kim, EH. et al. Efficacy of bioelectrical impedance analysis during the perioperative period in children. J Clin Monit Comput 31, 625–630 (2017). https://doi.org/10.1007/s10877-016-9881-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9881-1