Abstract
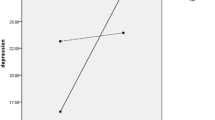
The incidence of stroke among younger adults in the United States is increasing. Few studies have investigated the prevalence of depressive symptoms after stroke among different age groups or the extent to which subjective stress at the time of stroke interacts with age to contribute to post-stroke depression. The present study examined whether there exists an age gradient in survivors’ level of depressive symptoms and explored the extent to which financial, family, and health-related stress may also impact on depression. Bivariate analyses (N = 322) indicated significant differences in depression and stress by age group, as well as differences in age and stress by 3-month depression status. Linear regression analyses indicated that survivors between the ages of 25–54 and 55–64 years old had, on average, significantly higher depressive symptom scores. Those with financial, family, and health-related stress at the time of stroke, irrespective of age, also had significantly higher scores.

Similar content being viewed by others
References
Aikens, J. E., Fischer, J. S., Namey, M., & Rudick, R. A. (1997). A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. Journal of Behavioral Medicine, 20, 433–445. doi:10.1023/A:1025547431847.
Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10, 77–84.
Aström, M., Adolfsson, R., & Asplund, K. (1993). Major depression in stroke patients. A 3-year longitudinal study. Stroke; a Journal of Cerebral Circulation, 24, 976–982. doi:10.1161/01.STR.24.7.976.
Ayerbe, L., Ayis, S., Wolfe, C., & Rudd, A. (2013). Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. British Journal of Psychiatry, 202, 14–21.
Banks, P., & Pearson, C. (2004). Parallel lives: Younger stroke survivors and their partners coping with crisis. Sexual and Relationship Therapy, 19, 413–429. doi:10.1080/14681990412331298009.
Bartoli, F., Lillia, N., Lax, A., Crocamo, C., Mantero, V., Carrà, G., & Clerici, M. (2013). Depression after stroke and risk of mortality: A systematic review and meta-analysis. Stroke Research and Treatment, 2013, 862978. doi:10.1155/2013/862978.
Berg, A., Palomäki, H., Lehtihalmes, M., Lönnqvist, J., & Kaste, M. (2003). Poststroke depression: An 18-month follow-up. Stroke, 34, 138–143. doi:10.1161/01.STR.0000048149.84268.07.
Berndt, E. R., Koran, L. M., Finkelstein, S. N., Gelenberg, A. J., & Keller, M. B. (2000). Lost human capital from early-onset chronic depression. The American Journal of Psychiatry, 157, 940–947.
Brott, T., Hertzberg, V., Adams, J., Olinger, C. P., Marler, J. R., Barsan, W. G., & Eberle, R. (1989). Measurements of acute cerebral infarction: A clinical examination scale. Stroke, 20, 864–870. doi:10.1161/01.STR.20.7.864.
Bury, M. (1982). Chronic illness as biographical disruption. Sociology of Health & Illness, 4, 167–182. doi:10.1111/1467-9566.ep11339939.
Carandang, R., Seshadri, S., Beiser, A., Kelly-Hayes, M., et al. (2006). Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. Journal of the American Medical Association, 296, 2939–2946.
Carlson, D. L. (2011). Explaining the curvilinear relationship between age at first birth and depression among women. Social Science and Medicine, 72, 494–503. doi:10.1016/j.socscimed.2010.12.001.
Chollet, F., Niclot, P., Guillon, B., Moulin, T., Marque, P., Pariente, J., & Jaillard, A. (2011). Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): A randomised placebo-controlled trial. Lancet Neurology, 10, 123–130. doi:10.1016/S1474-4422(10)70314-8.
de Haan, R., Limburg, M., Bossuyt, P., van der Meulen, J., & Aaronson, N. (1995). The clinical meaning of rankin ‘handicap’ grades after stroke. Stroke, 26, 2027–2030. doi:10.1161/01.STR.26.11.2027.
Fang, J., & Cheng, Q. (2009). Etiological mechanisms of post-stroke depression: A review. Neurological Research, 31, 904–909. doi:10.1179/174313209X385752.
Fure, B., Wyller, T. B., Engedal, K., & Thommessen, B. (2006). Emotional symptoms in acute ischemic stroke. International Journal of Geriatric Psychiatry, 21, 382–387.
Goetzel, R. Z., Hawkins, K., Ozminkowski, R. J., & Wang, S. (2003). The health and productivity cost burden of the “Top 10” physical and mental health conditions affecting six large U.S. employers in 1999. Journal of Occupational and Environmental Medicine, 45, 5–14. doi:10.1097/00043764-200301000-00007.
Goldberg, J. H., Breckenridge, J. N., & Sheikh, J. I. (2003). Age differences in symptoms of depression and anxiety: Examining behavioral medicine outpatients. Journal of Behavioral Medicine, 26, 119–132. doi:10.1023/A:1023030605390.
Hackett, M. L., & Anderson, C. S. (2005). Predictors of depression after stroke: A systematic review of observational studies. Stroke, 36, 2296–2301. doi:10.1161/01.STR.0000183622.75135.a4.
Hammen, C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293–319. doi:10.1146/annurev.clinpsy.1.102803.143938.
Irwin, M., Artin, K. H., & Oxman, M. N. (1999). Screening for depression in the older adult: Criterion validity of the 10-item center for epidemiological studies depression scale (CES-D). Archives of Internal Medicine, 159, 1701–1704. doi:10.1001/archinte.159.15.1701.
Kessler, R. C. (1997). The effects of stressful life events on depression. Annual Review of Psychology, 48, 191–214.
Kessler, R. C., Birnbaum, H., Bromet, E., Hwang, I., Sampson, N., & Shahly, V. (2010). Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R). Psychological Medicine, 40, 225–237.
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 617–627. doi:10.1001/archpsyc.62.6.617.
Kissela, B. M., Khoury, J. C., Alwell, K., Moomaw, C. J., Woo, D., Adeoye, O., & Kleindorfer, D. O. (2012). Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology, 79, 1781–1787. doi:10.1212/WNL.0b013e318270401d.
Kleindorfer, D. O., Khoury, J., Moomaw, C. J., Alwell, K., Woo, D., Flaherty, M. L., & Kissela, B. M. (2010). Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study. Stroke; a Journal of Cerebral Circulation, 41, 1326–1331. doi:10.1161/STROKEAHA.109.575043.
Kouwenhoven, S. E., Kirkevold, M., Engedal, K., & Kim, H. S. (2011). Depression in acute stroke: Prevalence, dominant symptoms and associated factors. A systematic literature review. Disability and Rehabilitation, 33, 539–556.
Lackland, D. T., Roccella, E. J., Deutsch, A. F., Fornage, M., George, M. G., Howard, G., & Towfighi, A. (2014). Factors influencing the decline in stroke mortality: A statement from the American heart association/american stroke association. Stroke, 45, 315–353. doi:10.1161/01.str.0000437068.30550.cf.
Laures-Gore, J. S., & DeFife, L. C. (2013). Perceived stress and depression in left and right hemisphere post-stroke patients. Neuropsychological Rehabilitation, 23, 783–797. doi:10.1080/09602011.2013.811087.
Lawrence, M. (2010). Young adults’ experience of stroke: A qualitative review of the literature. British Journal of Nursing (Mark Allen Publishing), 19, 241–248.
Lawrence, M., & Kinn, S. (2012). Determining the needs, priorities, and desired rehabilitation outcomes of young adults who have had a stroke. Rehabilitation Research and Practice. doi:10.1155/2012/963978.
Low, J. T. S., Kersten, P., Ashburn, A., George, S., & McLellan, D. L. (2003). A study to evaluate the met and unmet needs of members belonging to young stroke groups affiliated with the Stroke Association. Disability and Rehabilitation, 25, 1052–1056.
Mazure, C. M. (1998). Life stressors as risk factors in depression. Clinical Psychology: Science and Practice, 5, 291–313.
McCarthy, M. J., & Bauer, E. A. (2015). In sickness and in health: Couples coping with stroke across the lifespan. Health and Social Work, 40(3). Retrieved from http://hsw.oxfordjournals.org/content/early/2015/06/07/hsw.hlv043.full.
Mirowsky, J. & Kim, J. (2004). Age trajectories of depression: Growth-curve vectors, synthetic cohorts, and cross-sectional profiles. Paper presented at the annual meeting of the American Sociological Association, 08-14-2004, San Francisco, CA.
Morris, P. L., Robinson, R. G., Andrzejewski, P., Samuels, J., & Price, T. R. (1993). Association of depression with 10-year poststroke mortality. The American Journal of Psychiatry, 150, 124–129.
Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., & Turner, M. B. (2015). Heart disease and stroke statistics—2015 Update: A report from the American Heart Association. Circulation. doi:10.1161/CIR.0000000000000152.
Naess, H., Lunde, L., Brogger, J., & Waje-Andreassen, U. (2010). Depression predicts unfavourable functional outcome and higher mortality in stroke patients: The Bergen stroke study: Depression and stroke. Acta Neurologica Scandinavica, 122, 34–38. doi:10.1111/j.1600-0404.2010.01373.x.
Niedermaier, N., Bohrer, E., Schulte, K., Schlattmann, P., & Heuser, I. (2004). Prevention and treatment of poststroke depression with mirtazapine in patients with acute stroke. The Journal of Clinical Psychiatry, 65, 1619–1623. doi:10.4088/JCP.v65n1206.
Ouimet, M. A., Primeau, F., & Cole, M. G. (2001). Psychosocial risk factors in poststroke depression: A systematic review. Canadian Journal of Psychiatry, 46, 819–828.
Pan, A., Okereke, O. I., Sun, Q., Logroscino, G., Manson, J. E., Willett, W. C., & Rexrode, K. M. (2011). Depression and incident stroke in women. Stroke, 42, 2770–2775. doi:10.1161/STROKEAHA.111.617043.
Paradiso, S., & Robinson, R. (1998). Gender differences in poststroke depression. The Journal of Neuropsychiatry and Clinical Neurosciences, 10, 41–47.
Pohjasvaara, T., Leppävuori, A., Siira, I., Vataja, R., Kaste, M., & Erkinjuntti, T. (1998). Frequency and clinical determinants of poststroke depression. Stroke, 29, 2311–2317. doi:10.1161/01.STR.29.11.2311.
Robinson, R. G., Starr, L. B., Kubos, K. L., & Price, T. R. (1983). A two-year longitudinal study of post-stroke mood disorders: Findings during the initial evaluation. Stroke, 14, 736–741. doi:10.1161/01.STR.14.5.736.
Roding, J., Lindstrom, B., Malm, J., & Ohman, A. (2003). Frustrated and invisible: Young stroke patients’ experiences of the rehabilitation process. Disability and Rehabilitation, 25, 867–874.
Ronnlund, M., Sundstrom, A., Sorman, D. E., & Nilsson, L. (2013). Effects of perceived long-term stress on subjective and objective aspects of memory and cognitive functioning in a middle-aged population-based sample. Journal of Genetic Psychology, 174, 25–41.
Rook, K. S., Catalano, R., & Dooley, D. (1989). The timing of major life events: Effects of departing from the social clock. American Journal of Community Psychology, 17, 233–258.
Rush, A. J., Trivedi, M. H., Ibrahim, H. M., Carmody, T. J., Arnow, B., Klein, D. N., & Keller, M. B. (2003). The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54, 573–583. doi:10.1016/S0006-3223(02)01866-8.
Shrout, P. E., & Yager, T. J. (1989). Reliability and validity of screening scales: Effect of reducing scale length. Journal of Clinical Epidemiology, 42, 69–78. doi:10.1016/0895-4356(89)90027-9.
Taylor-Piliae, R. E., Hepworth, J. T., & Coull, B. M. (2013). Predictors of depressive symptoms among community-dwelling stroke survivors. Journal of Cardiovascular Nursing, 28, 460–467.
Tuohy, A., Knussen, C., & Wrennall, M. J. (2005). Effects of age on symptoms of anxiety and depression in a sample of retired police officers. Psychology and Aging, 20, 202–210. doi:10.1037/0882-7974.20.2.202.
Turner-Stokes, L., & Hassan, N. (2002). Depression after stroke: A review of the evidence base to inform the development of an integrated care pathway. Part 1: Diagnosis, frequency and impact. Clinical Rehabilitation, 16, 231–247. doi:10.1191/0269215502cr487oa.
West, R., Hill, K., Hewison, J., Knapp, P., & House, A. (2010). Psychological disorders after stroke are an important influence on functional outcomes: A prospective cohort study. Stroke, 41, 1723–1727. doi:10.1161/STROKEAHA.110.583351.
Whooley, M. A., Avins, A. L., Miranda, J., & Browner, W. S. (1997). Case-finding instruments for depression: Two questions are as good as many. Journal of General Internal Medicine, 12, 439–445. doi:10.1046/j.1525-1497.1997.00076.x.
Williams, L. S., Yilmaz, E. Y., & Lopez-Yunez, A. M. (2000). Retrospective assessment of initial stroke severity with the NIH stroke scale. Stroke, 31, 858–862. doi:10.1161/01.STR.31.4.858.
Wittayanukorn, S., Qian, J., & Hansen, R. A. (2014). Prevalence of depressive symptoms and predictors of treatment among US adults from 2005 to 2010. General Hospital Psychiatry, 36, 330–336. doi:10.1016/j.genhosppsych.2013.12.009.
Wulsin, L., Alwell, K., Moomaw, C. J., Lindsell, C. J., Kleindorfer, D. O., Woo, D., & Kissela, B. M. (2012). Comparison of two depression measures for predicting stroke outcomes. Journal of Psychosomatic Research, 72, 175–179. doi:10.1016/j.jpsychores.2011.11.015.
Zisook, S., Lesser, I., Stewart, J. W., Wisniewski, S. R., et al. (2007). Effect of age at onset on the course of major depressive disorder. The American Journal of Psychiatry, 164, 1539–1546.
Acknowledgments
This research was supported by funding from the National Institute on Neurological Disorders and Stroke [PI Kissela, Grant No R01NS030678-20].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael J. McCarthy, Heidi J. Sucharew, Kathleen Alwell, Charles J. Moomaw, Daniel Woo, Matthew L. Flaherty, Pooja Khatri, Simona Ferioli, Opeolu Adeoye, Dawn O Kleindorfer and Brett M Kissela declare that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
McCarthy, M.J., Sucharew, H.J., Alwell, K. et al. Age, subjective stress, and depression after ischemic stroke. J Behav Med 39, 55–64 (2016). https://doi.org/10.1007/s10865-015-9663-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-015-9663-0