Abstract
Purpose
The purposes of this study were to determine whether predictors of phrenic nerve palsy (PNP) exist and to test whether a standardized ablation protocol may prevent PNP during cryoballoon (CB) ablation using the 28 mm CB.
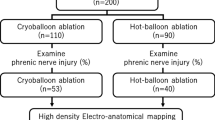
Methods
Three-dimensional (3D) geometry of the pulmonary veins (PV) and their relationship to the superior vena cava (SVC) was analyzed. Phrenic nerve (PN) stimulation was performed during ablation of the right-sided PVs with a 28-mm CB. The freezing cycle was immediately terminated in case of loss of PN capture.
Results
Sixty-five patients (age, 58 ± 11 years; ejection fraction, 0.59 ± 0.06; left atrial size, 40 ± 5 mm) with paroxysmal atrial fibrillation were included. No persistent PNP was observed. Transient PNP occurred in 4 of 65 patients (6 %). PN function normalized within 24 h in all four patients. A short distance between the right superior PV and the SVC was significantly associated with PNP, but left atrial and 3D PV anatomy were not. Low temperature early during the freezing cycle (<−41 °C at 30 s) predicted PNP with a sensitivity and a specificity of 100 and 98 %, respectively.
Conclusion
The anatomical relationship between the right superior PV and the SVC is a preprocedural predictor for the development of transient PNP, and low temperature early during ablation at the right superior PV is a sensitive warning sign of impending PNP. Despite the use of the 28 mm CB, transient PNP occurred in 6 % of patients undergoing CB ablation.




Similar content being viewed by others
References
Haissaguerre, M., Jais, P., Shah, D. C., Takahashi, A., Hocini, M., Quiniou, G., et al. (1998). Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. The New England Journal of Medicine, 339, 659–666.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., et al. (2010). Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation: Arrhythmia and Electrophysiology, 3, 32–38.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm, 9, 632–696.
Van Belle, Y., Janse, P., Rivero-Ayerza, M. J., Thornton, A. S., Jessurun, E. R., Theuns, D., et al. (2007). Pulmonary vein isolation using an occluding cryoballoon for circumferential ablation: feasibility, complications, and short-term outcome. European Heart Journal, 28, 2231–2237.
Neumann, T., Vogt, J., Schumacher, B., Dorszewski, A., Kuniss, M., Neuser, H., et al. (2008). Circumferential pulmonary vein isolation with the cryoballoon technique results from a prospective 3-center study. Journal of the American College of Cardiology, 52, 273–278.
Chun, K. R., Schmidt, B., Metzner, A., Tilz, R., Zerm, T., Koster, I., et al. (2009). The ‘single big cryoballoon’ technique for acute pulmonary vein isolation in patients with paroxysmal atrial fibrillation: a prospective observational single centre study. European Heart Journal, 30, 699–709.
Kuhne, M., Suter, Y., Altmann, D., Ammann, P., Schaer, B., Osswald, S., et al. (2010). Cryoballoon versus radiofrequency catheter ablation of paroxysmal atrial fibrillation: biomarkers of myocardial injury, recurrence rates and pulmonary vein reconnection patterns. Heart Rhythm, 7, 1770–1776.
Packer, D., Irwin, J. M., Champagne, J., Guerra, P., Dubuc, M., Wheelan, K., et al. (2010). Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front STOP-AF pivotal trial. Journal of the American College of Cardiology, 55, E3015–E3016.
Andrade, J. G., Khairy, P., Guerra, P. G., Deyell, M. W., Rivard, L., Macle, L., et al. (2011). Efficacy and safety of cryoballoon ablation for atrial fibrillation: a systematic review of published studies. Heart Rhythm, 8, 1444–1451.
Sanchez-Quintana, D., Cabrera, J. A., Climent, V., Farre, J., Weiglein, A., & Ho, S. Y. (2005). How close are the phrenic nerves to cardiac structures? Implications for cardiac interventionalists. Journal of Cardiovascular Electrophysiology, 16, 309–313.
Van Belle, Y., Knops, P., Janse, P., Rivero-Ayerza, M., Jessurun, E., Szili-Torok, T., et al. (2009). Electro-anatomical mapping of the left atrium before and after cryothermal balloon isolation of the pulmonary veins. Journal of Interventional Cardiac Electrophysiology, 25, 59–65.
Andrade, J., Dubuc, M., Guerra, P.G., Macle, L., Mondésert, B., Rivard, L., et al. (2012). The biophysics and biomechanics of cryoballoon ablation. Pacing and Clinical Electrophysiology, 35, 1162–1168
Schmidt, B., Chun, K. R., Ouyang, F., Metzner, A., Antz, M., & Kuck, K. H. (2008). Three-dimensional reconstruction of the anatomic course of the right phrenic nerve in humans by pace mapping. Heart Rhythm, 5, 1120–1126.
Kojodjojo, P., O’Neill, M. D., Lim, P. B., Malcolm-Lawes, L., Whinnett, Z. I., Salukhe, T. V., et al. (2010). Pulmonary venous isolation by antral ablation with a large cryoballoon for treatment of paroxysmal and persistent atrial fibrillation: medium-term outcomes and non-randomised comparison with pulmonary venous isolation by radiofrequency ablation. Heart, 96, 1379–1384.
Nieto-Tolosa, J., Rodriguez-Sanchez, D., Hurtado-Martinez, J.A., Pinar-Bermudez, E., Penafiel-Verdu, P., Sanchez-Munoz, J.J., et al. (2011). Phrenic nerve identification with cardiac multidetector computed tomography. Revista Española de Cardiología, 64, 942–944
Horton, R., Di Biase, L., Reddy, V., Neuzil, P., Mohanty, P., Sanchez, J., et al. (2010). Locating the right phrenic nerve by imaging the right pericardiophrenic artery with computerized tomographic angiography: implications for balloon-based procedures. Heart Rhythm, 7, 937–941.
Okumura, Y., Henz, B. D., Bunch, T. J., Dalegrave, C., Johnson, S. B., & Packer, D. L. (2009). Distortion of right superior pulmonary vein anatomy by balloon catheters as a contributor to phrenic nerve injury. Journal of Cardiovascular Electrophysiology, 20, 1151–1157.
Kim, D. H., Lu, N., Ghaffari, R., Kim, Y. S., Lee, S. P., Xu, L., et al. (2011). Materials for multifunctional balloon catheters with capabilities in cardiac electrophysiological mapping and ablation therapy. Nature Materials, 10, 316–323.
Franceschi, F., Dubuc, M., Guerra, P. G., & Khairy, P. (2011). Phrenic nerve monitoring with diaphragmatic electromyography during cryoballoon ablation for atrial fibrillation: the first human application. Heart Rhythm, 8, 1068–1071.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Commentary
Kuhne et al. evaluated whether a standardized protocol including phrenic nerve stimulation and the use of a large size (28 mm) balloon might prevent phrenic nerve palsy during Cryoballoon ablation of the right superior pulmonary vein. Although no case of persistent phrenic nerve palsy was reported, transient palsy occurred in 6% of patients. These findings support the notion that larger balloon sizes do not provide enough protection against the risk of phrenic nerve paralysis. Of note, the authors found that a short distance between the right superior pulmonary vein and the superior vena cava, and low temperature (< 41 degrees Celsius) during the first 30 seconds of the freezing cycle were predictors of phrenic nerve palsy with very high sensitivity (100%) and specificity (98%). Further studies are warranted to define whether a pre-operative assessment of the distance between the right superior pulmonary vein and the superior vena cava might be useful to select patients with the lower risk of phrenic nerve palsy during Cryoballoon ablation of the right superior pulmonary vein.
M. Kühne and S. Knecht contributed equally to this manuscript
Rights and permissions
About this article
Cite this article
Kühne, M., Knecht, S., Altmann, D. et al. Phrenic nerve palsy during ablation of atrial fibrillation using a 28-mm cryoballoon catheter: predictors and prevention. J Interv Card Electrophysiol 36, 47–54 (2013). https://doi.org/10.1007/s10840-012-9740-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-012-9740-z