Abstract
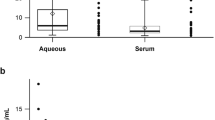
The aim of this study was to evaluate plasma adropin levels in patients with pseudoexfoliation (PEX). This retrospective case–control study included 35 patients with PEX and 35 individuals without PEX who served as controls. Plasma adropin levels with triglycerides, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and haemoglobin A1c (HGBA1C) concentrations were measured in both groups. The mean serum adropin levels were 3.24 ± 0.95 ng/mL (range, 1.90–7.88 ng/mL) in patients with PEX syndrome and 5.78 ± 2.85 ng/mL (range, 2.08–5.41 ng/mL) in PEX glaucoma patients. There was no statistically significant difference in mean adropin levels between PEX syndrome and PEX glaucoma patients. However, similar adropin levels were found in the PEX glaucoma patients and the control group (P > 0.05). The mean serum adropin levels were 3.34 ± 0.89 ng/mL (range, 1.90–5.39 ng/mL) in the PEX group and 5.78 ± 2.85 ng/mL (range, 3.08–11.06 ng/mL) in the control group. The mean serum adropin level of the PEX group was significantly lower than that of the control group (P < 0.001). There were no significant differences between the two groups in terms of serum glucose, total cholesterol, LDL, HDL, HGBA1C, triglycerides levels, or body mass index (all P > 0.05). Adropin level is lower in patients with PEX.
Similar content being viewed by others
References
Ritch R, Schlotzer-Schrehardt U (2001) Exfoliation syndrome. Surv Ophthalmol 45:265–315
Hewitt AW, Sharma S, Burdon KP, Wang JJ, Baird PN, Dimasi DP et al (2008) Ancestral LOXL1 variants are associated with pseudoexfoliation in Caucasian Australians but with markedly lower penetrance than in Nordic people. Hum Mol Genet 17:710–716
Amari F, Umihira J, Nohara M et al (1997) Electron microscopic immunohistochemistry of ocular and extraocular pseudoexfoliative material. Exp Eye Res 65:51–56
Schlötzer- Schrehardt UM, Koca MR, Naumann GO, Volkholz H (1992) Pseudoexfoliation syndrome ocular manifestation of a systemic disorder? Arch Ophthalmol 110(12):1752–1756
Mitchell P, Wang JJ, Smith W (1997) Association of pseudoexfoliation syndrome with increased vascular risk. Am J Ophthalmol 124:685–687
Shrum KR, Hattenhauer MG, Hodge D (2000) Cardiovascular and cerebrovascular mortality associated with ocular pseudoexfoliation. Am J Ophthalmol 129:83–86
Naji M, Naji F, Suran D, Gracner T, Kanic V, Pahor D (2008) Systemic endothelial dysfunction in patients with pseudoexfoliation syndrome. Klin Monbl Augenheilkd 225(11):963–967
Kumar KG, Trevaskis JL, Lam DD et al (2008) Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab 8:468–481
Lovren F, Pan Y, Quan A et al (2010) Adropin is a novel regulator of endothelial function. Circulation 122:185–192
Lian W, Gu X, Qin Y, Zheng X (2011) Elevated plasma levels of adropin in heart failure patients. Intern Med 50(15):1523–1527
Celik A, Balin M, Kobat MA et al (2013) Deficiency of a new protein associated with cardiac syndrome X; called adropin. Cardiovasc Ther 31(3):174–178
Aydin S (2015) A short history, principles, and types of ELISA, and our laboratory experience with peptide/protein analyses using ELISA. Peptides 72:4–15
Praveen MR, Shah SK, Vasavada AR et al (2011) Pseudoexfoliation as a risk factor for peripheral vascular disease: a case-control study. Eye 25:174–179
Schlötzer-Schrehardt U, Naumann GO (2006) Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol 141(5):921–937
Ovodenko B, Rostagno A, Neubert TA et al (2007) Proteomic analysis of exfoliation deposits. Invest Ophthalmol Vis Sci 48:1447–1457
Streenten BW, Li ZY, Wallace RN, Eagle RC Jr, Keshgegian AA (1992) Pseudoexfoliative fibrillopathy in visceral organs of a patient with pseudoexfoliation syndrome. Arch Ophthalmol 110:1757–1762
Mitchell P, Wang JJ, Smith W (1997) Association of pseudoexfoliation syndrome with increased vascular risk. Am J Ophthalmol 124:685–687
Shrum KR, Hattenhauer MG, Hodge D (2000) Cardiovascular and cerebro-vascular mortality associated with ocular pseudoexfoliation. Am J Ophthalmol 129:83–86
Atalar PT, Atalar E, Kilic H et al (2006) Impaired systemic endothelial function in patients with pseudoexfoliation syndrome. Int Heart J 47:77–84
Citirik M, Acaroglu G, Batman C, Yildiran L, Zilelioglu O (2007) A possible link between the pseudoexfoliation syndrome and coronary artery disease. Eye 21:11–15
French DD, Margo CE, Harman LE (2012) Ocular pseudoexfoliation and cardiovascular disease: a national cross-section comparison study. N Am J Med Sci 4:468–473
Tosun M, Simavli H, Önder HI, Erdurmus M (2014) Serum levels of omentin in pseudoexfoliation syndrome. J Glaucoma. doi:10.1097/IJG.0000000000000139
Türkyılmaz K, Öner V, Kırbas A, Sevim MS, Sekeryapan B, Özgür G, Durmus M (2013) Serum ykl-40 levels as a novel marker of inflammation and endothelial dysfunction in patients with pseudoexfoliation syndrome. Eye 27(7):854–859
Zhou JY, Chan L, Zhou SW (2014) Omentin: linking metabolic syndrome and cardiovascular disease. Curr Vasc Pharmacol 12:136–143
Topuz M, Celik A, Aslantas T, Demir AK, Aydin S, Aydin S (2013) Plasma adropin levels predict endothelial dysfunction like flow-mediated dilatation in patients with type 2 diabetes mellitus. J Investig Med 61(8):1161–1164
Kumar KG, Trevaskis JL, Lam DD et al (2008) Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab 8:468–481
Celik A, Balin M, Kobat MA et al (2013) Deficiency of a new protein associated with cardiac syndrome X; called adropin. Cardiovasc Ther 31(3):174–178
Zhang C, Zhao L, Xu W, Li J, Wang B, Gu X, Chen J (2014) Correlation of serum adropin level with coronary artery disease. Zhonghua Yi Xue Za Zhi 94:1255–1257
Funding
No funding supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Rights and permissions
About this article
Cite this article
Oğurel, T., Oğurel, R., Topuz, M. et al. Plasma adropin level in patients with pseudoexfoliation. Int Ophthalmol 36, 737–742 (2016). https://doi.org/10.1007/s10792-016-0185-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-016-0185-8