Abstract
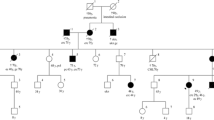
Mutations in DNA mismatch repair genes underlie lynch syndrome (HNPCC). Lynch syndrome resulting from mutations in MSH6 is considered to be attenuated in comparison to that caused by mutations in MLH1 and MSH2, thus more likely to be under diagnosed. In this study we report of a common mutation in the MSH6 gene in Ashkenazi Jews. Genetic counseling and diagnostic work-up for HNPCC was conducted in families who attended the high risk clinic for inherited cancer. We identified the mutation c.3984_3987dup in the MSH6 gene in 19 members of four unrelated Ashkenazi families. This mutation results in truncation of the transcript and in loss of expression of the MSH6 protein in tumors. Tumor spectrum among carriers included colon, endometrial, gastric, ovarian, urinary, and breast cancer. All but one family qualified for the Bethesda guidelines and none fulfilled the Amsterdam Criteria. Members of one family also co-inherited the c.6174delT mutation in the BRCA2 gene. The c.3984_3987dup in the MSH6 gene is a mutation leading to HNPCC among Ashkenazi Jews. This is most probably a founder mutation. In contrast to the c.1906G>C founder mutation in the MSH2 gene, tumors tend to occur later in life, and none of the families qualified for the Amsterdam criteria. c.3984_3987dup is responsible for 1/6 of the mutations identified among Ashkenazi HNPCC families in our cohort. Both mutations: c.3984_3987dup and c.1906G>C account for 61% of HNPCC Ashkenazi families in this cohort. These findings are of great importance for counseling, diagnosis, management and surveillance for Ashkenazi families with Lynch syndrome.



Similar content being viewed by others
Abbreviations
- AC:
-
Amsterdam criteria
- BC:
-
Breast cancer
- CRC:
-
Colorectal cancer
- DHPLC:
-
Denaturing high performance liquid chromatography
- HBOC:
-
Hereditary breast ovarian cancer
- HNPCC:
-
Hereditary non-polyposis colorectal cancer
- IHC:
-
Immunohistochemistry
- MMR:
-
Mismatch repair
- MSI:
-
Microsatellite instability
References
Abeliovich D, Kaduri L, Lerer I, Weinberg N et al (1997) The founder mutations 185delAG and 5382insc in BRCA1 and 6174delT in BRCA2 appear in 60% of ovarian cancer and 30% of early onset breast cancer patients among Ashkenazi woman. Am J Hum Genet 60:505–514
Banjerjee SK, Maldisi WF, Weston AP et al (1995) Microwave-based DNA extraction from paraffin-embedded tissue for PCR amplification. BioTechniques 18:768–773
Chan TL, Wai Chan Y, Ho JW et al (2004) MSH2 c. 1452–1455de1AATG is a founder mutation and an important cause of Hereditary Nonpolyposis Colorectal Cancer in the southern Chinese population. Am J Hum Genet 74:1035–1042
Chen S et al (2006) Prediction of germline mutations and cancer risk in the lynch syndrome. JAMA 296:1479–1487
Foulkes W, Thiffault I, Gruber SB et al (2002) The founder mutation MSH2*1906G→C is an important cause of hereditary nonpolyposis colorectal cancer in the Ashkenazi Jewish population. Am J Hum Genet 71(6):1395–1412
Fujita M et al (1995) Microsatellite instability and alterations in the hMSH2 gene in human ovarian cancer. Int J Cancer 64(6):361–366
Goldberg Y, Porat RM, Kedar I, Shochat C, Sagi M, Eilat A, Mendelson S, Hamburger T, Nissan A, Hubert A, Kadouri L, Pikarski E, Lerer I, Abeliovich D, Bercovich D, Peretz T (2008) Mutation spectrum in HNPCC in the Israeli population. Fam Cancer
Guillem JG, Glogowski E, Moore HG, Nafa K, Markowitz AJ, Shia J, Offit K, Ellis NA (2007) Single-amplicon MSH2 A636P mutation testing in Ashkenazi Jewish patients with colorectal cancer: role in presurgical management. Ann Surg 245(4):560–565
Hegde M, Blazo M, Chong B, Prior T et al (2005) Assay validation for identification of hereditary nonpolyposis colon cancer-causing mutations in mismatch repair genes MLH1, MSH2, and MSH6. J Mol Diagn 7(4):525–534
Hendriks YM, Wagner A, Morreau H et al (2004) Cancer risk in hereditary nonpolyposis colorectal cancer due to MSH6 mutations: impact on counseling and surveillance. Gastroenterology 127(1):17–25
Lynch HT, Coronel SM, Okimoto R et al (2004) A founder mutation of the MSH2 gene and hereditary nonpolyposis colorectal cancer in the United States. JAMA 291:718–724
Moisio AL, Sistonen P, Weissenbach J et al (1996) Age and origin of two common MLH1 mutations predisposing to hereditary colon cancer. Am J Hum Genet 59:1243–1251
Nilbert M, Wikman FP, Hansen TV, Krarup HB, Orntoft TF, Nielsen FC, Sunde L, Gerdes AM, Cruger D, Timshel S, Bisgaard ML, Bernstein I, Okkels H (2008) Major contribution from recurrent alterations and MSH6 mutations in the Danish Lynch syndrome population. Fam Cancer
Nystrom-Lahti M, Kristo P, Nicolaides NC et al (1995) Founding mutations and Alu-mediated recombination in hereditary colon cancer. Nat Med 1:1203–1206
Peterlongo P et al (2003) MSH6 germline mutations are rare in colorectal cancer families. Int J Cancer 107(4):571–579
Rodriguez-Bigas MA, Boland CR et al (1997) A National Cancer Institute workshop on hereditary nonpolyposis colorectal cancer syndrome: meeting highlights and Bethesda guidelines. J Natl Cancer Inst 89:1758–1762
Shiri-Sverdlov R et al (2000) Mutational analyses of BRCA1 and BRCA2 in Ashkenazi and non-Ashkenazi Jewish women with familial breast and ovarian cancer. Hum Mutat 16(6):491–501
Sun S et al (2005) The HNPCC associated MSH2*1906G C founder mutation probably originated between 1440 CE and 1715 CE in the Ashkenazi Jewish population. J Med Genet 42:766–768
Thiffault I, Hamel N, Pal T, McVety S, Marcus VA, Farber D, Cowie S, Deschênes J, Meschino W, Odefrey F, Goldgar D, Graham T, Narod S, Watters AK, MacNamara E, Du Sart D, Chong G, Foulkes WD (2004) Germline truncating mutations in both MSH2 and BRCA2 in a single kindred. Br J Cancer 90(2):483–491
Toledano H, Goldberg Y, Kedar-Barnes I, Baris H, Porat RM, Shochat C, Bercovich D, Pikarsky E, Lerer I, Yaniv I, Abeliovich D, Peretz T (2008) Homozygosity of MSH2 c.1906G–>C germline mutation is associated with childhood colon cancer, astrocytoma and signs of Neurofibromatosis type I. Fam Cancer
Umar A, Boland CR, Terdiman JP et al (2004) Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 96:261–268
Website links used
http://genome.ucsc.edu: (GenBank Accession no. NM000249, NM000251, and NM000179 for MLH1, MSH2, and MSH6, respectively)
http://www.ncbi.nlm.nih.gov/SNP/) and the HGVbase (http://hgvbase.cgb.ki.se/)
Acknowledgments
This work was supported, in part, by the Israeli Cancer Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldberg, Y., Porat, R.M., Kedar, I. et al. An Ashkenazi founder mutation in the MSH6 gene leading to HNPCC. Familial Cancer 9, 141–150 (2010). https://doi.org/10.1007/s10689-009-9298-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-009-9298-9