Summary
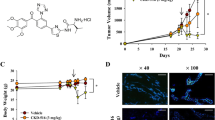
Targeting tumor vasculature is an emerging strategy in cancer treatment. Promising results have been shown in preclinical studies when vascular disrupting agents (VDAs) are used in combination with other anticancer therapies. Because radiation therapy with concurrent cisplatin or cetuximab has become standard treatment for patients with locally advanced head and neck squamous cell carcinoma (HNSCC), we investigated whether the VDA ombrabulin (AVE8062) could improve the antitumor activity of radiation plus cisplatin and radiation plus cetuximab combinations. HNSCC HEP2 or FaDu tumor bearing mice were treated with ombrabulin, cisplatin, cetuximab, local radiation therapy or combinations of these treatments. Ombrabulin attenuated tumor growth of HEP2 and FaDu xenografts compared to control tumors. A more pronounced tumor growth delay and tumor regression were induced when ombrabulin was added to local irradiation, cisplatin or cetuximab in FaDu tumors compared to single agent treatments. Finally, triple agent therapies combining ombrabulin, irradiation, and either cisplatin or cetuximab were more effective than double combination treatment regimens and increased tumor growth delay in both HEP2 and FaDu tumor models. Of note, complete tumor regression was achieved in FaDu tumor model for the triple combination including platinum. Immunohistochemistry on FaDu tumors demonstrated a specificity of ombrabulin towards intratumoral vessels, in contrast to peritumoral vasculature. Our results provide a rationale for the use of ombrabulin in combination with two standard treatment regimens that are concurrent cisplatin-based chemoradiation and cetuximab plus ionizing radiation therapies, for the treatment of HNSCC.




Similar content being viewed by others
References
Fung C, Grandis JR (2010) Emerging drugs to treat squamous cell carcinomas of the head and neck. Expert Opin Emerg Drugs 15:355–373
Marur S, Forastiere AA (2010) Challenges of integrating chemotherapy and targeted therapy with radiation in locally advanced head and neck squamous cell cancer. Curr Opin Oncol 22:206–211
Mehra R, Cohen RB, Burtness BA (2008) The role of cetuximab for the treatment of squamous cell carcinoma of the head and neck. Clin Adv Hematol Oncol 6:742–750
Pan Q, Gorin MA, Teknos TN (2009) Pharmacotherapy of head and neck squamous cell carcinoma. Expert Opin Pharmacother 10:2291–2302
Bonner JA, Harari PM, Giralt J et al (2006) Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med 354:567–578
Koutcher L, Sherman E, Fury M et al (2010) Concurrent cisplatin and radiation versus cetuximab and radiation for locally advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys 81:915–922
Denekamp J, Hill SA, Hobson B (1983) Vascular occlusion and tumour cell death. Eur J Cancer Clin Oncol 19:271–275
Horsman MR, Siemann DW (2006) Pathophysiologic effects of vascular-targeting agents and the implications for combination with conventional therapies. Cancer Res 66:11520–11539
Kanthou C, Tozer GM (2009) Microtubule depolymerizing vascular disrupting agents: novel therapeutic agents for oncology and other pathologies. Int J Exp Pathol 90:284–294
Siemann DW (2010) The unique characteristics of tumor vasculature and preclinical evidence for its selective disruption by Tumor-Vascular Disrupting Agents. Cancer Treat Rev 37:63–74
Delmonte A, Sessa C (2009) AVE8062: A new combretastatin derivative vascular disrupting agent. Expert Opin Investig Drugs 18:1541–1548
Dark GG, Hill SA, Prise VE et al (1997) Combretastatin A-4, an agent that displays potent and selective toxicity toward tumor vasculature. Cancer Res 57:1829–1834
Hori K, Saito S, Kubota K (2002) A novel combretastatin A-4 derivative, AC7700, strongly stanches tumour blood flow and inhibits growth of tumours developing in various tissues and organs. Br J Cancer 86:1604–1614
Hori K, Saito S, Sato Y, Kubota K (2001) Stoppage of blood flow in 3-methylcholanthrene-induced autochthonous primary tumor due to a novel combretastatin A-4 derivative, AC7700, and its antitumor effect. Med Sci Monit 7:26–33
Nihei Y, Suzuki M, Okano A et al (1999) Evaluation of antivascular and antimitotic effects of tubulin binding agents in solid tumor therapy. Jpn J Cancer Res 90:1387–1395
Ohsumi K, Nakagawa R, Fukuda Y et al (1998) Novel combretastatin analogues effective against murine solid tumors: Design and structure-activity relationships. J Med Chem 41:3022–3032
Hori K, Saito S (2003) Microvascular mechanisms by which the combretastatin A-4 derivative AC7700 (AVE8062) induces tumour blood flow stasis. Br J Cancer 89:1334–1344
Hori K, Saito S, Nihei Y et al (1999) Antitumor effects due to irreversible stoppage of tumor tissue blood flow: Evaluation of a novel combretastatin A-4 derivative, AC7700. Jpn J Cancer Res 90:1026–1038
Lavisse S, Lejeune P, Rouffiac V et al (2008) Early quantitative evaluation of a tumor vasculature disruptive agent AVE8062 using dynamic contrast-enhanced ultrasonography. Invest Radiol 43:100–111
Sessa C, Soria JC, Tolcher A et al. (2009) A phase I safety, pharmacokinetic and pharmacodynamic study of AVE8062, a novel vascular disrupting agent, in patients with advanced solid tumors. Ann Oncol 20: 7th International Symposium on Targeted Anticancer Therapies: abstract O36.
Kim TJ, Ravoori M, Landen CN et al (2007) Antitumor and antivascular effects of AVE8062 in ovarian carcinoma. Cancer Res 67:9337–9345
Ohno T, Kawano K, Sasaki A et al (2002) Antitumor and antivascular effects of AC-7700, a combretastatin A-4 derivative, against rat liver cancer. Int J Clin Oncol 7:171–176
Chaplin DJ, Hill SA (2002) The development of combretastatin A4 phosphate as a vascular targeting agent. Int J Radiat Oncol Biol Phys 54:1491–1496
Tozer GM, Kanthou C, Baguley BC (2005) Disrupting tumour blood vessels. Nat Rev Cancer 5:423–435
Plowman J, Dykes DJ, Hollingshead M et al. (1999) Human Tumor Xenograft Models in NCI drug development. Feibig HH BA, editor. Basel: Karger. 101–125.
Maggiorella L, Frascogna V, Poullain MG et al (2001) The olivacine S16020 enhances the antitumor effect of ionizing radiation without increasing radio-induced mucositis. Clin Cancer Res 7:2091–2095
Jordan MA, Kamath K (2007) How do microtubule-targeted drugs work? An overview. Curr Cancer Drug Targets 7:730–742
Thorpe PE (2004) Vascular targeting agents as cancer therapeutics. Clin Cancer Res 10:415–427
McKeage MJ, Baguley BC (2010) Disrupting established tumor blood vessels: an emerging therapeutic strategy for cancer. Cancer 116:1859–1871
Ekshyyan O, Rong Y, Rong X et al (2009) Comparison of radiosensitizing effects of the mammalian target of rapamycin inhibitor CCI-779 to cisplatin in experimental models of head and neck squamous cell carcinoma. Mol Cancer Ther 8:2255–2265
Joschko MA, Webster LK, Bishop JF et al (1997) Radioenhancement by cisplatin with accelerated fractionated radiotherapy in a human tumour xenograft. Cancer Chemother Pharmacol 40:534–539
Simons AL, Fath MA, Mattson DM et al (2007) Enhanced response of human head and neck cancer xenograft tumors to cisplatin combined with 2-deoxy-D-glucose correlates with increased 18 F-FDG uptake as determined by PET imaging. Int J Radiat Oncol Biol Phys 69:1222–1230
Morinaga Y, Suga Y, Ehara S et al (2003) Combination effect of AC-7700, a novel combretastatin A-4 derivative, and cisplatin against murine and human tumors in vivo. Cancer Sci 94:200–204
Hori K, Furumoto S, Kubota K (2008) Tumor blood flow interruption after radiotherapy strongly inhibits tumor regrowth. Cancer Sci 99:1485–1491
Ting LL, Belfi CA, Tefft M, Ngo FQ (1991) KHT sarcoma blood perfusion change after single-dose X-ray irradiation. Int J Radiat Biol 60:335–339
Siemann DW, Horsman MR (2004) Targeting the tumor vasculature: A strategy to improve radiation therapy. Expert Rev Anticancer Ther 4:321–327
Feng FY, Lopez CA, Normolle DP et al (2007) Effect of epidermal growth factor receptor inhibitor class in the treatment of head and neck cancer with concurrent radiochemotherapy in vivo. Clin Cancer Res 13:2512–2518
Harari PM, Huang SM (2001) Head and neck cancer as a clinical model for molecular targeting of therapy: Combining EGFR blockade with radiation. Int J Radiat Oncol Biol Phys 49:427–433
Huang SM, Bock JM, Harari PM (1999) Epidermal growth factor receptor blockade with C225 modulates proliferation, apoptosis, and radiosensitivity in squamous cell carcinomas of the head and neck. Cancer Res 59:1935–1940
Huang SM, Harari PM (2000) Modulation of radiation response after epidermal growth factor receptor blockade in squamous cell carcinomas: Inhibition of damage repair, cell cycle kinetics, and tumor angiogenesis. Clin Cancer Res 6:2166–2174
Krause M, Schutze C, Petersen C et al (2005) Different classes of EGFR inhibitors may have different potential to improve local tumour control after fractionated irradiation: A study on C225 in FaDu hSCC. Radiother Oncol 74:109–115
Goldman CK, Kim J, Wong WL et al (1993) Epidermal growth factor stimulates vascular endothelial growth factor production by human malignant glioma cells: A model of glioblastoma multiforme pathophysiology. Mol Biol Cell 4:121–133
Chen DJ, Nirodi CS (2007) The epidermal growth factor receptor: A role in repair of radiation-induced DNA damage. Clin Cancer Res 13:6555–6560
Dittmann K, Mayer C, Fehrenbacher B et al (2005) Radiation-induced epidermal growth factor receptor nuclear import is linked to activation of DNA-dependent protein kinase. J Biol Chem 280:31182–31189
Dittmann K, Mayer C, Rodemann HP (2005) Inhibition of radiation-induced EGFR nuclear import by C225 (Cetuximab) suppresses DNA-PK activity. Radiother Oncol 76:157–161
Gorski DH, Beckett MA, Jaskowiak NT et al (1999) Blockage of the vascular endothelial growth factor stress response increases the antitumor effects of ionizing radiation. Cancer Res 59:3374–3378
Schmidt-Ullrich RK, Mikkelsen RB, Dent P et al (1997) Radiation-induced proliferation of the human A431 squamous carcinoma cells is dependent on EGFR tyrosine phosphorylation. Oncogene 15:1191–1197
Raben D, Bianco C, Damiano V et al (2004) Antitumor activity of ZD6126, a novel vascular-targeting agent, is enhanced when combined with ZD1839, an epidermal growth factor receptor tyrosine kinase inhibitor, and potentiates the effects of radiation in a human non-small cell lung cancer xenograft model. Mol Cancer Ther 3:977–983
Ng QS, Mandeville H, Goh V et al (2011) Phase Ib trial of radiotherapy in combination with combretastatin-A4-phosphate in patients with non-small-cell lung cancer, prostate adenocarcinoma, and squamous cell carcinoma of the head and neck. Ann Oncol 23:231–237
Acknowledgments
We thank the Animal Department of the Gustave Roussy Institute for animal care, and Cyrus Chargari and Laurence Maggiorella for critical reading of the manuscript. This work was supported by a grant from Sanofi-Aventis R&D France to E. Deutsch.
Conflict of interest
C. Rubin-Carrez, A. Merino-Trigo and E. Jouannot are employees of Sanofi-Aventis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clémenson, C., Jouannot, E., Merino-Trigo, A. et al. The vascular disrupting agent ombrabulin (AVE8062) enhances the efficacy of standard therapies in head and neck squamous cell carcinoma xenograft models. Invest New Drugs 31, 273–284 (2013). https://doi.org/10.1007/s10637-012-9852-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-012-9852-4