Abstract
Background
Hospital-acquired pneumonia after an endoscopic submucosal dissection (ESD) can prolong the patient’s stay in the hospital, leading to greater healthcare costs. However, little is known of the characteristics and risk factors associated with this complication.
Aims
To analyze the clinical features of pneumonia after ESD and to suggest a treatment plan.
Methods
This was a retrospective study in which the cases of 1,661 consecutive patients who underwent ESD for 1,725 lesions between January 2008 and June 2011 were reviewed.
Results
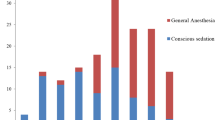
Of the 1,661 patients who underwent ESD during the study period, 38 were subsequently diagnosed with pneumonia, and an additional 18 patients exhibited lung consolidation, based on chest radiography, without respiratory signs or symptoms. The remaining 1,605 patients showed neither lung consolidation on chest radiography nor respiratory signs/symptoms. Continuous propofol infusion with intermittent or continuous administration of an opioid [odds ratio (OR) 4.498, 95 % confidence interval (CI) 2.267–8.923], a procedure time of >2 h (OR 2.900, 95 % CI 1.307–6.439), male gender (OR 2.835, 95 % CI 1.164–6.909), and age >75 years (OR 2.765, 95 % CI 1.224–6.249) were independent risk factors for pneumonia after ESD. In patients with only lung consolidation (without respiratory signs and symptoms), the length of hospital stay and prognosis were not affected by antibiotics use.
Conclusions
Deep sedation under continuous propofol infusion with opioid injection during ESD may be a risk factor for pneumonia.

Similar content being viewed by others
References
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Lochhead P, El-Omar EM. Gastric cancer. Br Med Bull. 2008;85:87–100.
Shimizu S, Tada M, Kawai K. Early gastric cancer: its surveillance and natural course. Endoscopy. 1995;27:27–31.
Anonymous. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–123.
Kojima T, Parra-Blanco A, Takahashi H, et al. Outcome of endoscopic mucosal resection for early gastric cancer: review of the Japanese literature. Gastrointest Endosc. 1998;48:550–554. discussion 554–555.
Makuuchi H, Kise Y, Shimada H, et al. Endoscopic mucosal resection for early gastric cancer. Semin Surg Oncol. 1999;17:108–116.
Coda S, Lee SY, Gotoda T. Endoscopic mucosal resection and endoscopic submucosal dissection as treatments for early gastrointestinal cancers in Western countries. Gut Liver. 2007;1:12–21.
Akasaka T, Nishida T, Tsutsui S, et al. Short-term outcomes of endoscopic submucosal dissection (ESD) for early gastric neoplasm: multicenter survey by Osaka University ESD study group. Dig Endosc. 2011;23:73–77.
Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006;41:929–942.
Isomoto H, Ohnita K, Yamaguchi N, et al. Clinical outcomes of endoscopic submucosal dissection in elderly patients with early gastric cancer. Eur J Gastroenterol Hepatol. 2010;22:311–317.
Lee IL, Wu CS, Tung SY, et al. Endoscopic submucosal dissection for early gastric cancers: experience from a new endoscopic center in Taiwan. J Clin Gastroenterol. 2008;42:42–47.
DeLegge MH. Aspiration pneumonia: incidence, mortality, and at-risk populations. JPEN J Parenter Enteral Nutr. 2002;26:S19–S24. discussion S24–S15.
Kozlow JH, Berenholtz SM, Garrett E, et al. Epidemiology and impact of aspiration pneumonia in patients undergoing surgery in Maryland, 1999–2000. Crit Care Med. 2003;31:1930–1937.
Anonymous. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112.
Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–140.
Cote GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:137–142.
Nayar DS, Guthrie WG, Goodman A, et al. Comparison of propofol deep sedation versus moderate sedation during endosonography. Dig Dis Sci. 2010;55:2537–2544.
van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, et al. Risk factors for aspiration pneumonia in frail older people: a systematic literature review. J Am Med Dir Assoc. 2011;12:344–354.
Knol W, van Marum RJ, Jansen PA, et al. Antipsychotic drug use and risk of pneumonia in elderly people. J Am Geriatr Soc. 2008;56:661–666.
Skull SA, Andrews RM, Byrnes GB, et al. Hospitalized community-acquired pneumonia in the elderly: an Australian case-cohort study. Epidemiol Infect. 2009;137:194–202.
Bleach NR. The gag reflex and aspiration: a retrospective analysis of 120 patients assessed by videofluoroscopy. Clin Otolaryngol Allied Sci. 1993;18:303–307.
Yoshida H, Ayuse T, Ishizaka S, et al. Management of exaggerated gag reflex using intravenous sedation in prosthodontic treatment. Tohoku J Exp Med. 2007;212:373–378.
Tagaito Y, Isono S, Nishino T. Upper airway reflexes during a combination of propofol and fentanyl anesthesia. Anesthesiology. 1998;88:1459–1466.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–671.
Tierney WM, Adler DG, Conway JD, et al. Overtube use in gastrointestinal endoscopy. Gastrointest Endosc. 2009;70:828–834.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, C.H., Kim, H., Kang, Y.A. et al. Risk Factors and Prognosis of Pulmonary Complications After Endoscopic Submucosal Dissection for Gastric Neoplasia. Dig Dis Sci 58, 540–546 (2013). https://doi.org/10.1007/s10620-012-2376-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2376-0