Abstract
Background
It has been suggested that breast and thyroid diseases may be linked. The aim of this study was to investigate the association between benign breast disease and subsequent risk of thyroid cancer.
Methods
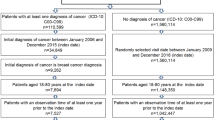
Postmenopausal women (n = 133,875) aged 50–79 years were followed up for a mean of 14 years. Benign breast disease was defined by history of biopsy. Incident thyroid cancer cases were confirmed by medical record review. Multivariable Cox proportional hazard modeling was used to estimate hazard ratios.
Results
There were 370 incident thyroid cancer cases during the follow-up period. Compared to women without BBD, women with BBD had a significant increased risk of thyroid cancer after adjusting for potential confounders (HR 1.38 95% CI 1.10–1.73), especially for women with more than two biopsies (HR 1.59 95% CI 1.10–2.26). There were no significant differences in thyroid tumor size, stage or histologic types between women with and without BBD.
Conclusion
Our large prospective study observed that postmenopausal women with BBD had an increased risk for thyroid cancer compared with women without BBD. A more detailed investigation of thyroid cancer risk according to different subtypes of benign breast disease is needed to better understand the association observed between thyroid and benign breast diseases.
Similar content being viewed by others
References
Vigneri R, Malandrino P, Vigneri P (2015) The changing epidemiology of thyroid cancer: why is incidence increasing? Curr Opin Oncol 27:1–7
Nagataki S, Nystrom E (2002) Epidemiology and primary prevention of thyroid cancer. Thyroid 12:889–896
Schonfeld SJ, Ron E, Kitahara CM et al (2011) Hormonal and reproductive factors and risk of postmenopausal thyroid cancer in the NIH-AARP Diet and Health Study. Cancer Epidemiol 35:e85–e90
Kabat GC, Kim MY, Wactawski-Wende J, Lane D, Wassertheil-Smoller S, Rohan TE (2012) Menstrual and reproductive factors, exogenous hormone use, and risk of thyroid carcinoma in postmenopausal women. Cancer Cause Control 23:2031–2040
Science JMECfCDaC (2016) Core-needle biopsy for breast abnormalities*. Rockville The Agency for Healthcare Research and Quality. (https://www.ncbi.nlm.nih.gov/books/NBK368367/pdf/Bookshelf_NBK368367.pdf)
Goehring C, Morabia A (1997) Epidemiology of benign breast disease, with special attention to histologic types. Epidemiol Rev 19:310–327
Dyrstad SW, Yan Y, Fowler AM, Colditz GA (2015) Breast cancer risk associated with benign breast disease: systematic review and meta-analysis. Breast Cancer Res Treat 149:569–575
Hartmann LC, Sellers TA, Frost MH et al (2005) Benign breast disease and the risk of breast cancer. N Engl J Med 353:229–237
Meinhold CL, Ron E, Schonfeld SJ et al (2010) Nonradiation risk factors for thyroid cancer in the US Radiologic Technologists Study. Am J Epidemiol 171:242–252
Ron E, Kleinerman RA, Boice JD Jr, LiVolsi VA, Flannery JT, Fraumeni JF Jr (1987) A population-based case-control study of thyroid cancer. J Natl Cancer Inst 79:1–12
Braganza MZ, de Gonzalez AB, Schonfeld SJ, Wentzensen N, Brenner AV, Kitahara CM (2014) Benign breast and gynecologic conditions, reproductive and hormonal factors, and risk of thyroid cancer. Cancer Prev Res (Phila) 7:418–425
Kuo JH, Chabot JA, Lee JA (2016) Breast cancer in thyroid cancer survivors: an analysis of the Surveillance, epidemiology, and end results-9 database. Surgery 159:23–29
Design of the Women's Health Initiative clinical trial and observational study (1998) The Women's Health Initiative Study Group. Control Clin Trials 19:61–109
Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, Rossouw JE (2003) The Women’s Health Initiative recruitment methods and results. Ann Epidemiol 13(9 Suppl):S18–S77
Bondy ML, Newman LA (2006) Assessing breast cancer risk: evolution of the Gail model. J Natl Cancer Inst 98:1172–1173
Yuan MK, Chang SC, Hsu LC, Pan PJ, Huang CC, Leu HB (2014) Mammography and the risk of thyroid and hematological cancers: a nationwide population-based study. Breast J 20:496–501
Zhang Y, Chen Y, Huang H et al (2015) Diagnostic radiography exposure increases the risk for thyroid microcarcinoma: a population-based case–control study. Eur J Cancer Prev 24:439–446
Sechopoulos I, Hendrick RE (2012) Mammography and the risk of thyroid cancer. AJR Am J Roentgenol 198:705–707
Ronckers CM, McCarron P, Ron E (2005) Thyroid cancer and multiple primary tumors in the SEER cancer registries. Int J Cancer 117:281–288
Mester J, Eng C (2015) Cowden syndrome: recognizing and managing a not-so-rare hereditary cancer syndrome. J Surg Oncol 111:125–130
Eng C (2000) Editorial: familial papillary thyroid cancer—Many syndromes, too many genes? J Clin Endocr Metab 85:1755–1757
Franceschi S, Preston-Martin S, Dal Maso L et al (1999) A pooled analysis of case–control studies of thyroid cancer. IV. Benign thyroid diseases. Cancer Causes Control 10:583–595
Giustarini E, Pinchera A, Fierabracci P et al (2006) Thyroid autoimmunity in patients with malignant and benign breast diseases before surgery. Eur J Endocrinol 154:645–649
Adamopoulos DA, Vassilaros S, Kapolla N, Papadiamantis J, Georgiakodis F, Michalakis A (1986) Thyroid disease in patients with benign and malignant mastopathy. Cancer 57:125–128
Bhargav PR, Mishra A, Agarwal G, Agarwal A, Verma AK, Mishra SK (2009) Prevalence of hypothyroidism in benign breast disorders and effect of thyroxine replacement on the clinical outcome. World J Surg 33:2087–2093
Acknowledgments
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C.” A short list of WHI investigators is in an appendix.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest.
Appendix: Short list of WHI investigators
Appendix: Short list of WHI investigators
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller.
Clinical Coordinating Center: Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg.
Investigators and Academic Centers:(Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Jennifer Robinson; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker; (University of Nevada, Reno, NV) Robert Brunner; (University of Minnesota, Minneapolis, MN) Karen L. Margolis.
Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Mark Espeland.
For a list of all the investigators who have contributed to WHI science, please visit: haps://www. whi. org/researchers/Documents %20%20Write %20a %2OP aper/WHI %20Investigator %20Long %20List.pdf.
Rights and permissions
About this article
Cite this article
Luo, J., Hendryx, M., Nassir, R. et al. Benign breast disease and risk of thyroid cancer. Cancer Causes Control 28, 913–920 (2017). https://doi.org/10.1007/s10552-017-0918-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-017-0918-7