Abstract
While there has been a trend toward greater disciplinary collaboration over the last several decades, the emergence of the HIV pandemic has required that disciplines work more closely and creatively to generate the multiple and innovative approaches necessary to meet the demands for effective prevention and treatment. This paper describes the nature of collaborative relationships among U.S. and Indian anthropologists, psychologists, demographers, epidemiologists, physicians and representatives of other fields and sectors in conducting a large scale, multi-year HIV/STD prevention project directed toward married men in urban poor communities in Mumbai (Bombay), India. The project has challenged members of the participating disciplines to develop a transdisciplinary conceptual model, to test the model with community-based formative research and to utilize the results in the development and implementation of a multi-level (community, provider and patient) intervention. The paper describes the interaction among disciplines and international sectors in the conceptualization, methodology and community-based action components of the project. In addition, it examines both the inhibiting and facilitating factors that are a part of the collaborative process. The paper concludes with implications for future transdisciplinary partnerships.
Similar content being viewed by others
The historical boundaries that defined and segmented one academic discipline from another are inadequate for addressing evolving societal problems. The protective environment of the academy has responded by allowing newly formed disciplines to develop innovative perspectives, methods, and concepts, distinct from and avoiding the hegemony and dominant paradigms of the more mature disciplines. Eventually, these youthful disciplines mature and develop their own conceptual and methodological rigidities, with appropriate calls for change and modification. The recent response of the biomedical sciences to this challenge has been to override departments by developing centers (e.g., neurological sciences, cancer and cardiology) that replace biochemistry, pharmacology, physiology, anatomy and other basic sciences. Another approach is to build conceptual bridges between disciplines by sharing the task of addressing real world problems, and in the process becoming transformed by this collaboration. This paper focuses on this latter approach to adapting disciplines to current problems–in this case the collaboration of anthropology, psychology, demography, epidemiology and medicine in addressing the challenges presented by the HIV/AIDS epidemic in urban poor communities in India.
The project that is at the focus of this paper is currently being conducted in three urban poor communities in Mumbai (Bombay), India. The project, entitled, Research and Intervention in Sexual Health: Theory to Action (RISHTA, an acronym meaning “relationship” in Hindi and Urdu, the local languages) is a collaboration of the Center for International Community Health Studies (CICHS) at the University of Connecticut Health Center, the Institute for Community Research (ICR), Hartford, CT and the International Institute for Population Sciences (IIPS) in Mumbai, the leading demographic institution in India. The project also involves significant input from TN Medical College (Mumbai) and CORO for Literacy, a non-governmental organization (NGO) that has been active in the study communities. The project uses a mixed-method (qualitative-quantitative) approach to examine the psychological and sociocultural factors that influence the risk of HIV/STD for married men in urban poor communities of India and has utilized the resulting data to design and evaluate a multi-level (community, health provider, patient) intervention to reduce this risk.
The international and interdisciplinary partnership that characterizes this project grew out of collaborative efforts between anthropologists and psychologists that began in the early 1990s (Bentley & Pelto, 2004; Schensul et al., 1996; Silva et al., 1997). In particular, the collaboration of the authors, Drs. Schensul, Verma, and Nastasi, represent the coming together of an anthropologist with a career commitment to applied and action research, both domestically and internationally; a psychologist from India with considerable training and research experience in reproductive health and men’s sexual risk; and a psychologist from the U.S. with a commitment to comprehensive and culturally sensitive intervention both domestically and internationally. The anthropologist (SL Schensul) was concerned not only with describing culture but utilizing that understanding to design intervention. The US-based psychologist (BK Nastasi) became interested in interdisciplinary and cross-cultural work as a way of expanding her understanding of psychological phenomenon related to health risks from an ecological and cultural perspective. The exploration into theories and research methods outside of Western psychology necessitated partnering with professionals from other disciplines such as anthropology and with psychologists from countries in South Asia. The Indian psychologist (RK Verma) was committed to a mix of qualitative and quantitative methods and a cultural perspective on men’s sexual risk.
As the project developed, the interdisciplinary focus was extended to include demographers with expertise in large-scale survey research, and STD epidemiologists and public health physicians with extensive experience in HIV/STD prevention and control and community health in India. Further institutional and community linkages brought together allopathic physicians, microbiologists, educators, and traditional healers and activists from the study communities. The RISHTA team thus reflects a partnership across countries, cultures, organizations, and disciplines as well as collaboration among researchers, interventionists, activists and community residents. Within the RISHTA team, we talk about RISHTA, East referring to the India faculty and staff and RISHTA, West referring to the US faculty and staff.
In this article, we describe the contributions of these collaborations to the conceptualization, methodology, and community-based action components of the project. In addition, we examine the factors that contributed to effective collaboration to meet the demands of a large-scale international community-based project. We conclude with implications of our work for future disciplinary partnerships.
Transdisciplinary research
In commenting on the need for collaboration among medical and social scientists, Rosenfield (199) states,
Creative collaboration requires more than social and medical scientists working on the same team. To achieve the level of conceptual and practical progress needed to improve human health, collaborative research must transcend individual disciplinary perspectives and develop a new process of collaboration (p. 1344).
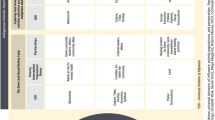
She defines three levels of disciplinary collaboration, which became a standard for evaluating disciplinary relationships: (1) “multidisciplinary [in which] researchers work in parallel or sequentially from [a] disciplinary-specific base to address common problems …” (2) “interdisciplinary [in which] researchers work jointly but [italics hers] still from [a] disciplinary-specific basis to address a common problem …” (3) “transdisciplinary in which researchers work jointly using [a] shared conceptual framework drawing together disciplinary-specific theories, concepts and approaches to address a common problem (p.1351).” Our complex, multi-year, international project was undoubtedly a combination of all three approaches, with our objective to be transdisciplinary in conception and action.
The development of a transdisciplinary approach generally starts on a personalistic level. Dr. Verma, a psychologist at IIPS and his team had produced groundbreaking work (funded by the Ford Foundation, Delhi) in identifying men’s concerns about sexual health problems in an urban community in Mumbai (Verma 2003; Verma et al., 2001; Verma et al., 2003). Dr. Schensul, an anthropologist and faculty member at UCHC, and a consultant to a series of Ford Foundation funded projects on sexuality and sexual risk in India worked with Dr. Verma, as the leader of one of the Foundation projects, to examine the implications of his work for intervention. Their initial discussions linked culturally-based definitions of sexuality and sexual morbidity with cognitively-defined perceptions of men’s priorities. Joint analyses conducted by Verma and Schensul (2004) demonstrated a relationship between men’s risky behavior and these culturally-based sexual concerns. In this case, the anthropological focus on culture melded effectively with the psychological perspective on cognition to address medical and epidemiological critics who saw these culturally-based concerns as esoteric and unrelated to addressing sexual risk. The collaboration also provided a direction for intervention, as men’s concerns about sexual health problems were seen as the basis for addressing the multiple factors in men’s lives that were involved in sexual risk behavior and HIV/STD transmission. With the cultural and psychological basis for intervention established, Dr. Nastasi joined to assist in identifying an intervention approach that would fit both the cultural concerns and the cognitive priorities of the population to be served. After assessing a number of approaches, the integration of techniques from narrative therapy with existing cognitive-behavioral approaches to risk prevention became the basis for an ecological approach to a multi-level intervention directed toward the community, provider and individual.
This model formed the basis for a successful response to a “request for proposal” (RFA) issued by the National Institute for Mental Health (NIH, USA), entitled, International Initiatives to Prevent HIV/STD Infection (MH-01-004, 2000). The RFA called for, “… new and expanded efforts between US-supported researchers and researchers in other nations to identify successful interventions for targeted populations; conduct scientifically valid and ethically sound HIV/AIDS prevention research, and, develop methods to implement prevention programs for large-scale use.” The extra-disciplinary and collaborative nature of this RFA provided the necessary context for the development and approval of the proposal, “Male Sexual Health Concerns and Prevention of HIV/STD in India” (Schensul, Verma, & Nastasi, 2004).
Disciplinary relationships
Anthropology brought to the world of ideas and concepts in the 20th century a commitment to empirically-based field research, a concern for understanding the diversity of cultures, a respect for the functional legitimacy of those cultures, and skepticism about the utility of the introduction of western ideas and technology. By the mid-point in the 20th century, the relatively young disciplines of psychology, demography and epidemiology became prominent in their separate domains providing varied perspectives on health issues. Psychology generated the primary theory and models of intervention for behavioral change that have been applied to a wide range of health concerns including mental health, substance abuse, lifestyle factors related to chronic disease, and HIV/AIDS. Demography, focused on population growth and transition, has played a central role in issues of fertility and family planning, infant and child morbidity, and reproductive health. A key element of international demography has been the Demographic and Health Survey (Macro International, 2005), which has been administered over 200 times in 70 countries. Epidemiological concepts and methods have become the hallmark of studies on infectious and chronic diseases in the US and internationally, and have established the designs and criteria for testing the efficacy of interventions and for monitoring disease vectors through sentinel surveillance.
The interface of anthropology with psychology, demography, and epidemiology has involved mutual criticism for much of the latter part of the 20th century. On the one hand anthropology is seen as qualitative, anecdotal, utilizing small samples and limited in its generalizations. On the other hand, anthropologists viewed the three other disciplines as imposing universal theories and results, not providing sufficient recognition of cultural diversity and context, and not utilizing the perspectives of members of the population under study. The broad survey approaches of epidemiology and demography were critically viewed by anthropologists, whereas epidemiologists and demographers looked with some disdain on ethnographic methods.
Nevertheless, each of the disciplines had sectors that reached out to one another, evolving sub-fields such as personality and culture (Barnouw, 1963; Wallace, 1970), anthropological demography (Kertzer & Fricke, 1997), cultural and social epidemiology (Janes et al., 1986; Trostle, 2005), and cross-cultural psychology (Bingham et al., 1999; Lopez & Guarnaccia 2000). Furthermore, professionals within the respective disciplines have called for greater collaboration to address societal problems (e.g., Sherif, 1963; Janes et al., 1986; Kertzer & Fricke, 1997; Trostle, 2005).
The rise of large scale NIH-funded domestic health projects in the realms of chronic disease, mental health, alcohol and drug abuse, and international projects funded by USAID have created the opportunities for the fields of anthropology, psychology and epidemiology to work together in addressing common problems. By the 1980s, research and intervention projects in minority and low income communities in the United States and in developing countries brought together representatives from multiple disciplines to address cultural differences, design interventions, promote behavioral change and evaluate efficacy. The growing degree of disciplinary collaboration was given even more impetus with the emergence of the HIV pandemic. Here was a problem that could not be the province of one discipline and required multiple and innovative approaches to treatment and prevention.
The conceptual and methodological world of HIV prevention
After almost a quarter of a century of HIV prevention programs, there is little consensus on the best approaches to HIV prevention. Because HIV is not casually acquired (as for example airborne diseases such as tuberculosis), transmission can be avoided by not having penetrative sex with an infected partner, and by not having direct blood to blood contact through the sharing of needles (either for vaccinations or through intravenous drug use) or in transfusions involving HIV-contaminated blood. If individuals could not avoid sex or intravenous drug use with an infected partner the prevention focus shifted to “harm reduction” by encouraging and supporting the use of condoms and clean needles through behavioral change interventions.
With the initial focus on behavioral change, the fields of psychology and communications were at the center of theories and models that guided intervention. Many of these conceptualizations, such as the health belief model (Rosenstock et al., 1988), cognitive (learning) theory (Bandura, 1980), theory of reasoned action (Ajzen & Fishbein, 1980), stages of change model (Prochaska & DiCelemente 1992), and theory of planned behavior (Ajzen, 1985) were developed in other arenas and adapted to HIV prevention. Others such as the AIDS Risk Reduction Model (ARRM, Catania, 1990) and the Information, Motivation, Behavior Model (IMB, Fisher & Fisher, 2000) were developed specifically for HIV prevention. These interventions are directed toward providing information; influencing attitudes, ideas, and motivations; and teaching skills to support engagement in health-promoting or risk-reducing behavior. Recognition of the importance of social ecology subsequently stimulated approaches for creating a supportive social environment for behavioral change, leading researchers and interventionists to develop approaches based on diffusion of innovation theory (Rogers, 1983) or to utilize opinion leaders (Kelly et al., 1993) or community mobilization (Kegeles et al., 1996) to support behavioral change. Consistent with an ecological perspective, Rhodes et al. (2005) describes interventions at the individual, micro (family and individual social network), meso (community) and macro levels (city, region and nation). Furthermore, recognition that the target of change could not be limited to the individual and community led to a focus on structural change (Blankenship et al., 2002) in laws, institutions, and societal stigmatization of persons living with AIDS.
After the first stage of the epidemic in most countries, HIV/AIDS became a disease of the poor. A number of authors (e.g., Basu, 2004; Mann, 1992; Mosley, 2004, Rhodes et al., 2005) have pointed to the spread of the epidemic among poor urban and rural communities, among the poorest countries and the most vulnerable populations (Heise & Elias, 1995; UNAIDS, 2001) and have argued that community mobilization that emphasizes risk reduction, vulnerability reduction and impact reduction provides the most effective approach.
Those who venture into the realm of HIV prevention must make many choices concerning level, focus, population, gender, and type of intervention. The RISHTA project sought to balance these choices by focusing intervention at the community, provider and individual level. It sought not only knowledge, attitudinal and behavioral change at these levels but structural change in the nature of health service provision for men. In addition, a supplementary grant provided by the Office of AIDS Research (2002–2005) allowed the RISHTA project to pursue a focus on women’s risk for acquiring HIV/STD within marriage that has resulted in a complementary research and intervention effort directed toward both women and the marital dyad. We were fortunate to have an NIMH RFA that called for a comprehensive approach to prevention of HIV/STD and a budget that allowed for the scope and length of the project.
The challenge
The HIV epidemic in India and other parts of Asia is growing rapidly. It is now estimated that more than five million people aged 15–49 are living with HIV/AIDS in India with a prevalence of 0.9% (National AIDS Control Organization, 2004; UNAIDS, 2004). Kumar (1999) has estimated the actual burden of HIV-infected people as 1.5% or 11.5 million individuals already infected with HIV, and Eberstat (2002) estimated 30–140 million new cases of HIV/AIDS in the period of 2000–2025. Although the actual and projected figures are in some dispute, it is generally agreed that AIDS will emerge as the single most important cause of adult mortality in India in the coming decade (UNAIDS, 2004).
In the absence of effective vaccine development and limitations on treatment, the emphasis for these countries and others in the developing world must be on prevention of transmission. Much of the transmission centers on men’s sexual behavior, both among those in special high-risk groups (e.g., truck drivers, long-distance traders, clients of sex workers) and those in the general population having risky premarital and extramarital sexual relationships. However, reproductive health services in India and in most other countries have not yet found effective approaches for consistent involvement of males in utilization of HIV/STD services and in engagement in reproductive health information, education, communication, and service programs (Collumbien & Hawkes, 2000). The majority of preventive efforts are in the form of safe sex messages and promotion of condoms (Behavioral Change Communication [BCC]) among those who are at high risk. Intervention programs, particularly for men, that provide a bridge between a population at risk and others in the general population are rare. Involving males in the reduction of sexually risky behavior and improvement of reproductive health is vital to reducing HIV/STD transmission both for themselves and their female and male sexual partners. Finding an approach that begins with and addresses men’s most salient reproductive health issues can establish a policy framework and an intervention methodology that has significant implications for India as well as for other developing and developed countries.
Both the literature (Bhugra & de Silva, 1995; Kulhara & Avasthi, 1995; Pelto, Joshi, & Verma, 1999) and our preliminary studies showed that most men in India have a very clear culturally-derived sense of sexual problem priority (e.g., performance over disease), etiology (inappropriate semen loss), consequences (threats to masculinity), and treatment approach (preference for traditional over allopathic providers). This culturally-driven sense of sexual problems also seems to be closely intertwined with how men construct masculinity and reflect sex-stereotypes that boys and girls grow up with in the South Asian context. At a time of increasing incidence of HIV/STD, these cultural concepts and their psychological manifestations, beliefs, and actions strongly contrast with the usual intervention focus on disease prevention, risky behavior reduction, early allopathic treatment, and accurate sexual health information.
The concerns of many Indian and South Asian men center on the concept of gupt rog (“secret illnesses” in Hindi), which relate primarily to sexual performance problems such as impotence, erectile dysfunction and early ejaculation. Although gupt rog can also incorporate symptoms of sexually transmitted diseases, the emphasis is on problems in sexual functioning related to the cultural expectations of a “real man.” In preliminary research leading to this project in one of the study communities, 43.7% of a random sample of 1344 men reported a gupt rog problem in the last two months (Verma & Schensul, 2004). In the baseline survey of a systematic random sample of 2408 men in three communities in this project, 53.6% reported that they had at least one gupt rog problem in the last three months. The primary cause of these problems are seen as a result of excessive semen loss due to nocturnal emission and masturbation. The consequences of these problems are evidenced in low self-esteem, marital conflict, domestic violence and validation of masculinity through extramarital sex, many of the factors that increase risk for HIV/STD (Schensul et al, 2004). A significant number of men (18–58% depending on the specific problem) seek treatment for gupt rog problems primarily from the traditional, non-allopathic Indian systems of medicine including ayurveda, unani and homeopathy, where men can expect an understanding of and respect for gupt rog problems in contrast with the primarily disdainful attitudes of the allopathic providers.
The RISHTA program sought to apply this culturally-based concept of gupt rog as a means of addressing HIV and other sexually transmitted diseases with the following reasoning, derived from formative data:
-
The concept of gupt rog provided a “gift” for interventionists in that it identified a culturally salient and focal concept of sexual health problems that could be extended to HIV/STD
-
Gupt rog problems were a part of men’s perceived needs; any reproductive health service in India that hoped to introduce early identification of HIV/STD and to increase safer sex practices for men needs to start by addressing these male sexual health concerns
-
Men showed limited knowledge of sexually transmitted diseases and had many misconceptions associated with STDs and gupt rog.
-
A significant number of men sought treatment for these problems from non-allopathic traditional providers, thus establishing a resource system and an epistemological approach to these problems that could be a focal point for intervention
-
The nature of gupt rog problems were identified as deeply linked to men’s self-esteem and sense of masculinity, providing an opportunity to assess and address linkages between cultural concepts and psychological manifestations.
-
The complex and misdirected sense of masculinity reinforced by the cultural concept of gupt rog led many men to seek risky sex outside marriage in their effort to validate their potency and male control.
-
Gupt rog problems were related to the nature of the marital relationship that included a wife’s negative perception of her husband’s sexual performance, domestic violence, and alcohol use.
The anthropologists, psychologists and epidemiologists hypothesized that risky sex was linked to both gupt rog problems and sexually transmitted diseases and that gupt rog problems would be an indicator of sexually transmitted diseases. We further hypothesized that negative concepts of masculinity, reinforced by peers, would be related to risky behavior and that negative concepts of masculinity (male domination) would be associated with negative marital and household relationships. The researchers adopted an ecological model that was consistent with approaches in both anthropology and psychology and was a result of considerable interaction among the framers of the proposal.
The RISHTA model
The discussions among the international and transdisciplinary partners led to the formulation of a conceptual model that incorporated culturally-specific elements of sexual health and structural changes in health service provision within the sociocultural realities of the urban poor of India. The model drew on approaches to HIV/STD prevention developed in the United States, and the anthropological, psychological, demographic and epidemiological perspectives of professionals from both countries. To facilitate a broader understanding of sexual health problems in India and development of culture-specific interventions for prevention and risk-reduction of HIV/STDs, the project called for an interdisciplinary approach consistent with recent thinking about health promotion (Leviton, 1996) and with our earlier work on sexual risk in South Asia (Nastasi et al., 1998–99; Silva et al., 1997; Verma et al., 1998).
At the same time, the research team drew on the perspective of both Indian psychologists and non-allopathic providers in addressing the issue of sexual health behavior. Traditional health practitioners have continued to be the primary source of health information and beliefs among people in India. These beliefs influence health practices in terms of diet, hygiene, preventive measures, and traditional choices. A large body of research by Kleinman and his associates (1980) based on their work in India and China has demonstrated the prevalence of these concepts. However, the field of culturally-based beliefs and health practices has largely remained unexplored and Indian psychologists have only recently realized the potential of this area (Dalal, 2001).
Barring a few exceptions (Kakar, 1982, 1991), Indian psychologists have largely focused on universal personality traits and attitudes as derived from the West as the crucial dispositional factors associated with different diseases and health behavior (Dalal, 2001; Singh, 1984). In an extensive review of health psychology, Dalal (2001) points out two dispositional factors: one referring to behavior (Type A personality) and the other to attitude (health modernity, Singh, 1984). The concepts related to traditional culture and healing underlying the RISHTA program have been only recently explored by Indian psychologists. As Dalal (2001) has stated, “A striking and obvious need is to more thoroughly investigate traditional Indian health beliefs and practices; religious and cultural beliefs not only relate to the broader issues of life and suffering but also greatly influence our perceptions of health and disease, causality, treatment related decisions and long term care (p. 399).”
Key steps in the formulation of the research and intervention were the review of existing literature and preliminary research with the non-allopathic providers in the study communities. The RISHTA ecological model was in part geared to be consistent with the canons and historical texts of all three non-allopathic healing traditions. Despite some differences between these non-allopathic healing disciplines, their common canons focus on a holistic preventive and positive health approach that seeks to effect a balanced state of the body, mind and emotions to contribute to preservation and restoration of health (Leslie & Young, 1992). Preliminary data, however, indicated that the traditional providers were rapidly taking on the approach of the allopaths including short visits, symptom orientation and treatment with antibiotics and other allopathic medicines. It was concluded that it would be possible to develop training that would support and strengthen the still salient characteristics of the traditions of Indian systems of healing, while also providing training on effective diagnosis and treatment of STDs and an ecological approach to addressing the factors in men’s lives contributing to risky sex. Although anthropology has consistently signaled the importance of the traditional healer, much of the incorporation of the healer into intervention has emphasized allopathic approaches. In the RISHTA project, issues associated with gupt rog, STD and risky sex called for a return to the holistic traditions.
The intervention approach adopted by the RISHTA team reflected the integration of theory, research, and practice from psychology, anthropology, and medicine. Drawing upon the research conducted by the RISHTA team and others, a culture-specific intervention for HIV/STD risk reduction and prevention—the Narrative Intervention Model (NIM)—was developed. The approach integrated principles and strategies from narrative therapy (Eron & Lund, 1996; Howard, 1991; McNamee, 1996; McNamee & Gergen, 1992; Sarbin, 1986), cognitive therapy (Beck, 1976; Ellis, 1962), cross-cultural psychology, cognitive-behavioral approaches to sexual risk prevention and risk reduction (Azjen & Fishbein, 1980; Fisher & Fisher; 1993; Kelly, 1995), with preliminary data on gupt rog and its treatment by traditional providers and approaches to syndromic management advocated by the World Health Organization (WHO, 1993). The theoretical underpinnings of NIM reflect social construction (Berger & Luckman, 1966; Nastasi et al., 1998/1999; Vygotsky, 1978; Wertsch, 1991), bioecological (Bronfenbrenner, 1989, 1999), anthropological (Kleinman, 1986; Pelto & Pelto, 1997; Wallace, 1961) and social-psychological perspectives (Abrams & Niaura, 1987; Azjen & Fishbein, 1980; Bandura, 1986; Fisher & Fisher, 1993; Jemmott & Jones, 1983; Miller, Bettencourt, DeBro, & Hoffman, 1993).
The rationale underlying NIM developed out of extended discussions across disciplinary and national boundaries; perhaps what is most indicative of the transdisciplinary underpinnings of NIM is the difficulty in identifying which ideas and principles were contributed by specific disciplinary members of the team. The RISHTA team proposed that human behavior, particularly behavior related to sexual health, is influenced by the interaction of biological, psychological, and sociocultural factors. Behavior linked to sexual risk is influenced by cognitions (ideas, attitudes, beliefs) that develop or are transmitted primarily through social or interpersonal interactions. Through these interpersonal interactions, culture (embodied in ideas, beliefs, values, and norms) is transmitted and influences the development of cognitions and behavior patterns. Culturally-transmitted cognitions influence not only behavioral responses but also the interpretation of internal responses (e.g., emotions, perceptions, bodily processes) and external contextual (physical and social environment) experiences. Through repeated experiences, individuals develop narratives or scripts that guide their behavior. Consistent with cognitive-behavioral intervention models (e.g., Fisher & Fisher, 1993), the NIM emphasizes the role of cognition in guiding behavior and is based on the assumption that changes in thinking (e.g., ideas, beliefs, values) are critical to behavioral change. The importance of culture in guiding human behavior reflected our anthropological and psychological focus and is consistent with bio-ecological perspectives in psychology (Bronfenbrenner, 1989, 1999) and with the holistic principles of traditional healing in India.
The process of narrative therapy (e.g., Eron & Lund, 1996), based in social constructionist thinking, guided the approach to addressing men’s culturally based thinking about sexuality and sexual health problems. Narrative therapy is focused on the use of clients’ stories (narratives constructed through interaction with the provider) to assess the affective, cognitive, behavioral and social-cultural elements of the presenting problem, and to facilitate change in these elements through a systematic de-construction and re-construction of the story. Thus, a primary limitation of extant cognitively oriented approaches—failure to focus adequately on social and cultural factors—was addressed directly through the use of narrative.
The idea for using narratives as the basis for intervention grew out of the stories that men in the study communities told about their lives as they described their sexual health concerns during in-depth interviews conducted in the formative research. This sample of Indian men linked performance issues, masculinity, risky sex and complicated primary relationships with wives or other sex partners in their narratives about sexual health problems. Thus, it was hypothesized that any approach to issues of behavioral change required knowledge of the individual’s sociocultural history to provide a sense of how to structure interpersonal interactions between provider and client that could lead to reconstruction of the relevant personal narratives to incorporate health-promoting beliefs, attitudes, and behaviors. Through the use of focused interpersonal interactions, trained practitioners could then help individuals to: (a) identify the narrative related to the presenting problem (construct the narrative), (b) critically examine the psychological and socio–cultural factors that influence or maintain the problem (deconstruct), and (c) create a revised narrative that leads to solving the problem (reconstruct). The construction-deconstruction-reconstruction process would thus lead to the development of a personal narrative supporting health-promoting and risk-reducing behaviors related to HIV/STD prevention and treatment.
In the development of the intervention model, the RISHTA team attempted to integrate psychological and anthropological perspectives within an intervention that incorporated (a) medical diagnosis and treatment of men’s sexual health concerns, (b) evidenced-based cognitive-behavioral risk-reduction strategies based in psychology, (c) current Indian medical practices that reflected both indigenous and Western-influenced approaches, and (d) cultural beliefs and normative behaviors of Indian men. Based on his own formative research, the Indian psychologist on the team identified gupt rog as an appropriate culturally-based concept. The anthropologist viewed gupt rog as an emic (insider; participant) approach to the endogenously defined problem of HIV/STD risk. The U.S. psychologist utilized the concept of narrative therapy to construct the epistemological basis for structuring therapeutic intervention; that is, constructing, deconstructing, and reconstructing a narrative that would alter misconceptions, reduce risky behavior, and address the ecological factors contributing to sexual risk. The Indian psychologist drew on his knowledge of the priorities of Indian men and the orientation of traditional Indian providers. The physicians contributed the medical perspective through adoption of the WHO-endorsed (WHO, 1993) syndromic management approaches to diagnosis and treatment of sexually transmitted diseases. Syndromic management involves a process of diagnosis, treatment, referral, partner notification, and education based on the patients’ symptoms, and is particularly relevant to contexts in which expensive medical testing is prohibitive.
Thus, the resulting model, referred to as the NIM, reflected current medical, psychological, and sociocultural perspectives. The collaboration across the disciplines was critical to development of a model that integrated biological, psychological, and cultural dimensions of men’s sexual health problems into a coherent intervention approach. The articulation of this model into practice was dependent on learning from and inclusion of community-based medical practitioners, thus extending the medical perspective to include indigenous systems of medicine.
Project implementation
The project consists of three phases: (a) formative research with men with sexual health problems, identification of treatment resources, an assessment of the study communities, refinement of community and patient instruments and implementation of a baseline survey with 2400 men from three communities; (b) development and implementation of a multi-level intervention involving community education, training and capacity building for allopathic doctors in one experimental community and non-allopathic doctors in the other experimental community, and a culturally based therapeutic approach to treatment of patients presenting sexual health problems; and (c) evaluation of the intervention among patients and in the communities as a whole. The project employs a quasi-experimental design utilizing pre-test, post-test, comparison and experimental groups and mixed methods (qualitative-quantitative) to examine the acceptability, integrity, effectiveness and sustainability of the multi-level (community, provider, patient) intervention.
The formulation of a quasi-experimental design drawn from psychology and epidemiology was relatively new for the anthropological and demographic team members for two reasons: (a) the role of research was to generate the development and effective implementation of an intervention; and (b) the testing of the intervention required a design that would control for threats to the validity of outcome results. All the represented disciplines engaged in extensive discussions about the design and its logistic implications, allowing those discipline representatives who were less familiar with experimental design to learn about its advantages, provide input to the implementation of components, and recognize the demands of NIH. In addition, the disciplinary representatives with expertise in intervention design were provided with opportunities to consider ideas from other perspectives that ultimately enhanced the design and implementation of the project.
Formative research
Interdisciplinary collaboration resulted in the use of mixed methods in the formative and evaluative components of the project and the development of an integrated intervention model (the NIM) that addressed medical, psychological, and cultural factors related to men’s sexual risk. The dominant methodology for the demographically-oriented IIPS had been quantitative survey research. Over the last decade a number of anthropologists, including Pelto (see Pelto & Pelto, 1997), Schensul (Schensul & Le Compte, 1999) and Schensul (Schensul et al., 1999) had presented and discussed the utility of a mixed methodology that would include qualitative data collection methods. The Indian psychologist (Verma), based at IIPS, utilized qualitative methods extensively in his research and trained his staff in interviewing, social mapping and consensus modeling (Weller & Romney, 1988). At the time of initiation of this project, qualitative research was well established at IIPS and was a core part of the methodological curriculum for demography graduate students. The U.S. psychologist (Nastasi) had engaged in mixed-methods research for the purpose of design and evaluation of assessment and intervention tools and collaborated with the anthropologist on an examination of the role of qualitative methods in evaluation of interventions (Nastasi and Schensul 2005). Thus, the use of mixed-methods not only reflected the integration of methods across disciplinary lines resulting from the interactions within the RISHTA project, but also indicated the prior influence of transciplinary study and work for individual team members.
In the formative phase (one and a half years), the team relied heavily on anthropological methods to examine the cultural beliefs, values, language, norms, and practices of the target populations—married men living in three urban poor communities in India, the doctors (allopathic and non-allopathic) who provided medical treatment for men’s sexual health concerns, and the communities in which the men lived and the doctors practiced. The central methods of qualitative anthropology were used, including key-informant interviews with community experts (e.g., governmental officials, community leaders, members of community-based organizations) who could characterize the overall situation (approximately 50); individual in-depth interviews with men (52), providers (39) and women (66) about their own lives and practices; and social and geographic mapping of the communities to locate where the men lived, sought treatment, and practiced risky sex. Although the methods were primarily anthropological, members of all participating disciplines took part in formulating interview questions and procedures, training and supervision of field staff, and preliminary review of interview data. While the India staff focused on primary data collection, U.S. staff also participated in the field visits and interview process with the help of bilingual interpreters. As a result, U.S. staff had first hand experience in participation in field research and learning from community residents and community activities. Similarly, although analysis of qualitative data, utilizing a computer-based, text search program (Atlas.ti, Scientific Software, 2004) was conducted at the US component, the overall analysis plan and specific code categories and their definitions were developed, examined and reviewed jointly. Quantitative data analysis was shared based on allocations that were negotiated among disciplines and members of the India and US components.
The final step in the formative research phase was conducting a baseline survey for a random sample of 2400 men in the three study communities and the collection of urine and blood samples for STD testing. Survey construction began with a collaborative review of the qualitative data to operationalize the major domains and factors in this study. While there was some use of scales from other validated instruments, the great majority of the items on the survey instrument came directly from the qualitative data in the formative research phase, leading us to term this approach to instrument construction, an “ethnographic survey” (Schensul et al., 1999). This approach combined the cultural and local focus of the anthropologists with the survey approaches of the demographers and the epidemiologists.
The draft items were reviewed by the full team and the resulting instrument was pre-tested and modified, pilot-tested with analysis conducted jointly by US and India staff, and a final instrument developed. The IIPS demographers utilized their sampling expertise to generate a “systematic random sample” utilizing the smallest units (lanes) in each of the three study communities.
The process of STD testing for gonorrhea, Chlamydia, HSV-2 and syphilis was a unique step for all the disciplines, with the exception of the STD epidemiologists, and represented one of the first community-based surveys for sexually-transmitted diseases in India. In this phase of the project, the RISHTA East project coordinator, who had an extensive background as a public health physician, took leadership. The procedures for this component were established by the STD epidemiological and microbiological consultants to the project. A random sample of 640 men from the 2400 who had been administered the survey instrument were selected for STD testing. Reviewing the pros and cons of various STD tests, developing the logistics for sample collection and identifying local and national laboratories for analyzing the samples provided an excellent opportunity for the varied disciplines to learn from microbiology, public health and STD epidemiology.
The next task involved the physician coordinator and demographers informing the community leadership of the STD survey and seeking their support. In addition, it was necessary to identify multiple locations in the communities with private rooms and a toilet where samples could be collected. Community leadership that included local government officials, Hindu and Muslim religious leaders, heads of local political parts and members of community-based organizations, recognized the importance of the project, were assured that all individuals that were STD positive would receive appropriate treatment and worked with the project to make announcements at mosques, temples and organizations throughout the community. The physician coordinator recruited male physicians and residents from the Department of Social and Preventive Medicine of TN Medical College in Mumbai to assist in pre-test general exams and counseling. The STD operation was completed with 642 men tested in multiple locations in the communities without any adverse reactions. With the RISHTA banner flying over each location, the project became well-known in the communities as a result of STD testing, even prior to the intervention. Throughout the process of STD testing and the return of results, the social scientists became increasingly knowledgeable about and participatory in the microbiology of the testing, the epidemiology of the results and the logistics of managing a community-based STD survey.
Intervention
The initial plan for the intervention involved three components: (a) community-level education in the three study communities; (b) provider-level capacity building and training for allopathic doctors at the governmental urban health clinic in one experimental community and for private non-allopathic doctors in the other experimental community; and (c) patient-level intervention by the trained doctors in the two experimental communities. In each of these three levels of intervention, the cultural model of sexual health problems was the starting point, with the development of new narratives as a means of addressing the need for reduction in risky behavior.
The objective of the community-level intervention was to create on the part of the community at large a revised narrative that linked performance-related problems to issues of masculinity, lifestyle, and spousal relationships that would support the development of health-promoting and risk-reducing behaviors related to HIV/STD prevention and treatment. In the experimental communities the objective was also to create awareness on the part of the residents of the presence and accessibility of project-trained providers who were able to address their sexual health problems with respect, comprehensiveness, and efficacy. Community level education is being delivered in all three communities in the form of local media (posters, local advertisements), community meetings, street drama, special community events (melas), and interpersonal communication between intervention team members and residents.
The training of service providers (public allopathic and private non-allopathic doctors) to deliver patient-level intervention involved the use of a participatory consultation approach based on our previous work in South Asia (Nastasi et al., 2000a; Nastasi, 2000b). In this approach practitioners received skills development training in a workshop format preceding the intervention implementation (initial training), with follow-up training and consultation throughout implementation on both a scheduled and ad hoc basis (ongoing consultation). Practitioners received approximately 20 hours of initial training (conducted by RISHTA staff) on empirical and conceptual underpinnings of the intervention, key intervention strategies, and on the application of syndromic management, an algorithm developed by WHO to treat STD on the basis of observed and reported symptoms (WHO, 1993). Workshop activities included lecture, demonstration, practice, and feedback. Formal follow-up training sessions were conducted every three months to provide additional instruction on components of the intervention (e.g., syndromic management, psychological aspects of sexual health problems) and to enhance implementation (e.g., practice in assessment and intervention for psychological and social-cultural factors). Weekly visits to the practitioners by project field staff served the dual purpose of providing support to practitioners and monitoring implementation integrity and acceptability. Based on feedback from these visits, monthly meetings with practitioners were also initiated to provide a context for discussion of challenges in implementing NIM.
The patient intervention delivered by the trained allopathic and traditional providers was seen as fostering knowledge, attitude/belief, and behavioral changes in individual clients that would lead to appropriate culture-specific, care-seeking behaviors and HIV/STD risk-reduction behaviors. The intervention combined assessment, education, counseling and treatment to (a) address the medical/physical, psychological and social relationship issues related to male sexual health concerns; (b) provide accurate information about STDs, particularly HIV/AIDS transmission, risk reduction, and prevention; (c) determine the presence of STD symptoms to make referrals for STD testing and treatment as warranted; and (d) assess the need for social services related to economic, family, and individual psychological concerns and make referrals as warranted.
The results of the formative research phase presented new challenges for the project’s international, interdisciplinary team. The task at this point was to develop the intervention components based on sound empirical results. Again the diversity of perspectives played an important role in the final design of the intervention. In particular, findings about men’s utilization of the health care system and the nature of the providers’ practice suggested modifications of the proposed provider component.
The public (governmental) primary care system in the three study communities consists of three urban health centers and two health posts. Health posts are primarily staging areas for community education and health campaigns (e.g., immunization, case-finding and treatment of tuberculosis). Urban health centers are located in large, permanent facilities and in theory provide a range of services. The municipal government provides the physical infrastructure, nursing and lower level staff, while Mumbai-based medical colleges are assigned specific urban health centers to which they provide physicians, residents and interns. Utilization data from the urban health center in one of the study communities indicated that very few men sought care at the facility, which was defined in the community as a maternal and child health center. Of the men who did seek treatment there, none presented sexual health problems of either performance dysfunction or STD symptoms. In addition, the data showed that only 10% of the 245 private providers in the three study communities were allopaths, presenting the problem that there were not a sufficient number to establish a trained private allopathic group in any one community.
The team proposed an enhanced capacity that would attract males to the urban health center and address both general and sexual health problems. A series of discussions between the project physician on the India side, the faculty from TN Medical College that provided physician staffing and the administration of the urban health center resulted in the formulation of a male health clinic at the urban health center with hours and days of operation distinct from the women’s clinics and staffed by male TN Medical College faculty and residents. A general health clinic for men based in a facility that heretofore was focused on maternal and child health was new to India. Yet, for a relatively small expenditure, the concept of a male health clinic reaching and engaging men held great promise. The formulation of that idea was a result of the interaction and collaboration of multiple disciplines, the perspective of community residents, and the linkage of multiple institutions working jointly on a problem.
The traditional providers constituted our second experimental intervention. Formative research data indicated that the 245 private practitioners identified in the three study communities could be categorized into ayurveda (79, 32.2%), homeopathy (73, 29.8%), unani (67, 27.3%) and allopathy (MBBS 26, 10.6%). Based on the provider reports of utilization, it was estimated that the 245 private practitioners see more than 6800 patients daily in the three study communities. Furthermore, the private practitioners saw more men (an estimated 3000 per month) than any other sector of the Indian health care system. These providers saw a monthly average of over 2400 male patients with sexual health problems and an estimated 1350 individuals with STD-like problems. These data suggested that the private practice providers, of which the private, non-allopathic practitioners represented over 90%, were a major resource for addressing the general health of communities, a particularly important resource for men, and even more importantly, for men with sexual health problems.
Initially, it was proposed that the Narrative Intervention Model (NIM) would be a good match to the practice model of traditional providers because of the epistemological emphasis on holistic medicine. In line with this notion, the training was to be designed to reinforce the holistic model through NIM and to upgrade the syndromic management of sexually transmitted infections. However, the formative data and initial training with non-allopathic providers indicated that the actual practice of these doctors reflected a move away from traditional holistic models toward a symptom-focused approach utilizing allopathic medicines (Schensul et al., 2005). Working with the community-based providers forced the team to rethink the training model in order to increase the emphasis on holistic medicine (i.e., addressing the psychological, cultural and biological aspects of disease). This required extended training on the process components of NIM such as how to gather data from men about lifestyle and beliefs, and how to integrate these data into education and prevention messages and supportive counseling. Currently, the team is continuing its efforts to promote a return to a holistic approach. Successful development of a sustainable and transferable model in India is likely to depend on integrating this reality of contemporary indigenous systems of medicine with our efforts to reduce sexual risk. In this process, the community-based providers have become key partners, thus broadening the interdisciplinary focus. In the process of these interactions, not only has the RISHTA model for training and implementation expanded, but the trained traditional providers have begun to return to their epistemological roots. As the patients respond positively to the focus on psychological and cultural factors, the doctors have renewed their commitment to a holistic approach.
The methodological design of this large scale project was a result of the contributions of professionals from the disciplines of epidemiology, demography, medicine, biochemistry, anthropology, and psychology. It is unlikely that professionals from any single discipline could bring the necessary range of methodological expertise to such a project. In addition, involving several disciplines as partners in the process of project development and implementation served to foster ownership and commitment that is rarely the case when using a more typical consultation model in which professionals provide advice to project staff about methodology but are not key partners.
The collaborative process: facilitating and inhibiting factors
This project team represented great diversity in terms of country of origin and residence (USA and India), institutional base (universities, nongovernmental institutions, private business and governmental agencies), discipline (anthropology, demography, medicine, microbiology, psychology, and public health), religion (Hindu, Muslim, Christian, and Jewish) and work experience (research and intervention), age (30–63), gender, and socioeconomic and educational background. The enormous potential for positive production by such a diverse team is balanced with the equivalent potential for misunderstanding and miscommunication both professionally and interpersonally. In this section we examine the inhibiting and facilitating factors that influenced the process of collaboration.
Inhibiting factors
Inhibiting factors reflected the influence of geographical distance, institutional culture, language differences, and disciplinary and personal variations in belief systems and practices. The two parts of the RISHTA team, East and West, were 10,000 miles apart and had to depend on e-mail as the major mode of long distance communication. E-mail can greatly facilitate communication; for example, e-mails sent from the U.S. in the evening could be responded to by morning and e-mails sent in the evening from India were available in the U.S. by early morning. At the same time, e-mail can be a quicker mode of “miscommunication” as short statements are used to sort out complex issues or a lack of communication is viewed as a kind of message. E-mail correspondence thus became another forum for negotiating perspectives and modes of communication across disciplines and cultures.
The two collaborating universities each had concerns about the nature of the project. The demographic university in India was unsure about its role in intervention in local communities, because research and national policy had been its primary foci to date. There has also been some uncertainty expressed at IIPS as to demography’s role in sexuality and sexual risk research. Some faculty at IIPS have been concerned that the interest in RISHTA among the demography graduate students has provided too much encouragement for them to focus their Master’s and Ph.D. theses on sexual risk. At the same time, UCHC in the U. S. had not shown a strong commitment to international research. The Institute for Community Research primarily focused on local research and intervention but was committed to international work with other current projects in China, India, and South America.
The NIMH grant was received by the UCHC and funds were committed to a sub-contract with IIPS. In the original budget proposal it was envisaged that the U.S. University would receive 80% of the funds and the Indian university 20%. This was estimated largely due to the imbalance in the salaries that were ten times higher in U.S. than in India. However, over the lifetime of the project, additional funds from the U.S. side were allocated to the India side increasing Indian share to the total budget to 35%. The additional funds were allocated to the India side due to the weakness of the US dollar, the rising costs of personnel in India and the costs associated with STD testing. On the India-side, the staff consists of 18 full-time staff and two faculty, whereas on the US-side there are one full-time faculty equivalent (PI, co-PI and statistician) and two full time staff. The process of negotiating budgets for the IIPS sub-contract is primarily conducted by the PI (S. Schensul) and the co-PIs at IIPS. Despite the re-budgeting there is a sense on the India-side that flexible funds are always available on the US-side and that cost-overruns and expansion of the sub-contract is always possible, giving way to some degree of tension at the beginning and end of each grant year.
The University in the Indian context is very hierarchically structured, with clear distinctions between senior and junior faculty, faculty and staff, and male and female faculty and staff. At the same time, undue credit is given for the conceptual and methodological expertise of the US faculty and staff. These real and perceived hierarchies served from time to time to undermine the transdisciplinary objective of the RISHTA project by limiting the input by some of the junior members of the collaborative group. These limitations included a reluctance to contribute to the discussion, the domination of the discussion by senior people, or the devaluation of the input based on the lower status of the speaker. The U.S. faculty and staff were required to understand this hierarchy and negotiate multiple lines of communication by being careful not to dominate discussions and to ensure that all individuals were being heard. The process of negotiating relationships and integrating ideas across these cultural boundaries is ongoing.
Although all key personnel on the India team were bi- or multi-lingual and fluent in English, there were sufficient differences between Indian and U. S. English to create miscommunication and misunderstandings. In one instance, for example, the use of the US English term “shame” meant to communicate “a pity that things did not work out” was interpreted to mean an “accusation” that an Indian team member had not acted “appropriately.”
Another element of the interplay of nationality and discipline was that the dominant discipline paradigm for IIPS was demography, which placed the RISHTA project in a position that challenged demography’s boundaries with regard to methods, intervention, and relationships with local communities. Disciplinary boundaries could emerge at any time, for example, with regard to ownership or leadership of particular project components based on discipline. The demographers “owned” the sampling and survey process, the anthropologists owned the qualitative data, the medical/public health people owned the STD testing and sample collection process and the psychologists owned the intervention and evaluation. This sense of ownership at times inhibited contributions of others, who too readily ceded a research or intervention activity to the primary discipline. On the other hand, the demonstration of a willingness to learn about each other’s discipline and to respect its core knowledge frequently opened the door to greater transdisciplinary participation. Nevertheless, this process of crossing established cultural, disciplinary and hierarchical boundaries involved the development of trust and openness to ideas from others. As the expertise of individual team members was honored over time, mutual respect developed and team members became more willing to integrate ideas from others. The process of relationship building was critical to the success of this collaboration.
The organization of the RISHTA project meant that both RISHTA East and RISHTA West staff owned every aspect of the project ranging from conceptualization, data collection, analysis and rights to publication and dissemination. In terms of operations however, responsibilities were divided to ensure accountability and efficiency. For example, RISHTA East staff took on the responsibility for data collection and transcription/entry, while the RISHTA-West staff was responsible for putting together the qualitative and quantitative data analysis plan and preliminary analysis. It is expected that as the project moves into its final year, the reduced need for field operations and staff will be replaced by an increased involvement of individuals on the India side in data analysis.
The ongoing challenges that occur in any project are magnified with such a diverse project team. The team experienced misunderstandings regarding time pressures and competing responsibilities for key personnel, inevitable delays, bureaucratic procedures, and external pressures. These misunderstandings led to expressions of frustration both within and across geography, culture, institution and discipline. Fortunately, the RISHTA East and West team members’ commitment to the project and the needs of the community overshadowed such misunderstandings and frustrations.
Facilitating factors
The many facilitating factors more than balanced the barriers to effective collaboration and communication. The close personal relationships between the core collaborators included sharing many dinners both at home and in restaurants, participation in family events such as weddings, religious festivals, and temple visits, and meeting and spending time with families and relaxed time together. When RISHTA, West members travel to RISHTA, East there is a flurry of dinner invitations, concern about welfare and assistance with any medical needs. When work became overwhelming, a day off was planned collaboratively. In turn, when RISHTA, East staff visit they are put up in the home of the PI and have joined family events, observed religious rituals, are taken to see the sights of the northeast US, and have traded their Indian cooking skills for the ethnic cooking of their US counterparts.
US faculty and staff generally stay on the campus at the IIPS Guest House or in hotels in close proximity to IIPS and the study communities. These locations are not “five star” but are comfortable and have the advantage of creating a modest and more locally appropriate residential location for US colleagues than the more extravagant hotels in Central Mumbai.
The US-based principal investigator, co-PI and project coordinator have been alternatively on-site in RISHTA, East for approximately six months in each year of the grant. This regular presence has had a number of advantages in terms of transdisciplinary work. First, the constant feedback in the interaction between the field and the project, unplanned events, and community response requires rapid re-conceptualization and planning. US staff presence means greater understanding of needs and demands, representation in the planning process and participation in problem solving. Second, the visits provide the opportunity for US staff to expand their understanding of the language, culture and lives of the residents in the study communities. To facilitate this learning process, US staff make it a point to spend time in the communities, participating in group discussions, street dramas, individual interviews, community events and other project activities. Although no one on the US-side speaks Hindi, members of the RISHTA staff provide effective translation and facilitate communication with residents. This regular field and site involvement increases communication among disciplines and international components and allows the project to build inductively through on-going feedback from the communities. Furthermore, the frequency of visits facilitates the development of collegial and personal relationships that form the basis for the ongoing transdisciplinary and international partnerships.
Electronic transmission has played a significant role in facilitating analysis and interpretation of data. Once qualitative and quantitative data are transcribed, translated, entered and de-identified on the India-side, they are sent to the US. This rapid transmittal has meant that preliminary analyses could be conducted on an ongoing basis, feedback could be provided quickly to data gatherers and the efficacy of interview guides, pilot instruments and other field operations could be assessed by RISHTA, East and West. Thus, despite its limitations, electronic communication provides a mechanism for supplementing the face-to-face interactions afforded by periodic visits to project sites.
In addition to the facilitating factors related to mechanisms of communication, there are a number of other factors that transcend modes of communication. These include shared values related to project goals, long-term professional relationships and collaborative experiences, the multi-year nature of the project, the openness of individual team members to learn from others, and shared commitment to mutual benefit. Each of the US and Mumbai-based sectors and discipline representatives are strongly committed to the project goals and to the welfare of the residents of the study communities. Consequently, even when disagreements across disciplinary or national boundaries arise, the focus on project goals and the local community is maintained. This commitment has been paramount in ensuring successful integration of perspectives across disciplines and cultural and structural boundaries.
The success of transdisciplinary collaboration within the RISHTA project is dependent in large part on the long-term nature of the relationships among team members. These relationships have included the long-term collaboration of the anthropologist and psychologist from the U.S., university to community partnerships in India, psychologist and demographer collaborations at IIPS, and psychologist and medical doctor and medical doctor and community relationships in India. Thus, team members possessed the necessary personal and interpersonal characteristics and skills to work effectively together. Furthermore, the majority of team members have a demonstrated commitment to working with and learning from others. These experiences and characteristics of individual team members contributed to open and respectful communication about conceptual, methodological and action components of the project. The RISHTA team’s communication was characterized by “listening to all the voices” irrespective of discipline or status.
The open dialogue that characterized the face-to-face and electronic communications among team members was viewed as a recursive process in which issues could be revisited at the request of any team members. Consequently, team members frequently requested discussion of conceptual, methodological, or logistic aspects of the project as they identified information from the field or the professional community or as they developed new insights. The recursive process was reflected also in the procedures for data collection and project monitoring. RISHTA East and West team members engaged in ongoing communication about data collected in the field or issues that arose with regard to project implementation. Project procedures were established to facilitate communication, for example, through regular meetings of project staff members with community-based doctors and educators, regular staff meetings for data dissemination and decision making, and periodic visits of US team members to the project site in Mumbai. Consistent with the commitment to community participants, team members gave priority to community feedback from doctors, community educators, project participants and other community members.
The long-term nature of the project is also a critical factor in facilitating transdisciplinary collaboration. Sufficient time is needed to develop relationships, learn from each other, accommodate to different work styles and personalities, and integrate disciplinary perspectives and methodologies effectively. An indication of the multi-year opportunity provided by the NIH grant is reflected in the adoption of shared perspectives that demonstrate a synergistic integration across disciplines, cultures, and individuals. Such perspectives are reflected not only in the project products but also in the individual thinking of team members. For example, the anthropologists and psychologists developed an integrated anthropological-psychological-medical-epidemiological perspective that influences not only their thinking about the project but their view of the world.
Such integration of views has been evident among team members who explicitly acknowledge their changed perspectives. For example, in the development of the NIM, debates centered on the relative predominance of psychological, cultural or medical approaches; that is, should the approach be primarily medical with some attention to psychological and cultural considerations, or should the approach be driven primarily by psychological theory with integration of medical and cultural perspectives. The debates over the predominance of disciplinary approaches resulted in the integrated model in which medical, cultural and psychological factors are considered of equal importance. Reaching agreement on a transdiciplinary model required that each of the disciplinary representatives change their thinking to include a broader and newly defined perspective.
Finally, the potential for professional benefits to all team members is critical. For example, joint presentations at professional meetings in the US, India and internationally have taken place among all the represented disciplines and collaborative writing for publication is required. The development of these products provides opportunities for individual team members to take leadership in dissemination (e.g., each member has an opportunity to serve as primary presenter or lead author). Such products benefit not only the respective disciplinary audiences, but also the individual team members. In addition, dissemination of findings to the community participants is viewed as a key outcome and is consistent with the project team’s commitment to the community.
In the final years of the grant, RISHTA has begun to focus on the issue of sustainability and replicability of various components. Several steps have been taken by the transdisciplinary team. They have included: (1) developing a transdisciplinary proposal focused on reducing the risk of transmission for married women in the three study communities; (2) recruiting other NGOs and community-based organizations to maintain and expand community education focused on sexual risk; (3) seeking support from Mumbai municipal authorities to provide funding for the male health clinic and the training and support of the non-allopathic providers; (4) presenting the results of the RISHTA project to Indian national conferences and policymakers for replication in other locations; and (5) presentation and discussion with international researchers and policymakers to replicate the RISHTA model in other countries. Each of these steps is being pursued by representatives of all the disciplines and institutions, resulting in new transdisciplinary challenges in conceptualization and action.
As these examples of facilitating factors suggest, effective collaboration depends on mutual commitment to project goals, interpersonal relationships, and continual communication and negotiation to insure the involvement of all participants and the addressing of conflicts in perspectives and needs. Perhaps most importantly, the benefits of such collaborative research extend beyond the contributions to knowledge and practice to include benefits to individual members of the community and the research team. The opportunities for personal and professional growth along with contributions to the local and scientific community are key factors in fostering commitment to the participatory process.
Discussion: Implications for transdisciplinary partnerships
Transdisciplinary research requires considerable effort in developing professional and personal relationships that lead to effective collaboration. At the first level is the relationship among disciplines as disciplinary theories and perspectives compete for a role in the development of conceptual models driving both research and intervention. Although disciplinary competition, sharing, and negotiation can go on ad infinitum, it is the community-based component that keeps the disciplinary representatives honest and focused, and exposes alternative theoretical models to the empirical reality of community life. Thus community-based research may hold the key that opens the passageway between disciplines in that it continually calls for the best ideas and methods (not those presented most forcibly, or by a particular discipline, or by a senior person) to encompass the realities and complexities of local communities, rather than abstraction of large national and global populations. We posit that the emphasis on addressing key social issues and application in a local setting is an essential element of transdisciplinary research.
A central feature of the collaboration that characterizes the RISHTA project was the opportunity for Schensul to work closely with Verma on the analysis of the preliminary data that led to this project. The principle here is that relationships must begin early and prior to the point where a project has been conceived or developed for funding. This early start provides the opportunity to develop rapport, to meet mutual agendas, to share methods and perspectives, and to collaborate on next steps. As a result, new and expanded projects can be built on solid relationships that have developed over time.
Transdisciplinary projects involve significant time to share theory and methods, to develop participatory rather than hierarchical structures, to develop personal relationships, to jointly analyze data, and to jointly develop the products of research, intervention and evaluation. An element of this extended time involves sharing of skills and knowledge to achieve effective participation. Time also needs to be allocated to interpersonal dynamics that, if ignored, can serve to inhibit the achievement of the objectives of the project.
The initial selection of collaborating disciplines may be a result of both happenstance and a priori decisions, but the team should not be considered set because the research may call at any time for new skills and knowledge to address emerging issues. In the RISHTA project, much more time, effort and money was spent on the STD testing process than anticipated, with special emphasis on the specific procedures used for STD testing. Although we had two excellent STD epidemiologists as consultants, in retrospect, we needed more consistent input in selection of the tests, assessment of interim results, and analysis of final data. In addition, it was necessary to significantly increase our clinical focus both in relationship to the male health clinic and to the traditional providers. As a result, we made significant efforts, after the initiation of the project, to involve the physicians at TN Medical College and bring in non-allopathic expertise to strengthen our training and consultation to providers. Additionally, our relationships with CORO were developed when community outreach and education needed enhancement. The principle here is that new community challenges may require mid-stream additions to the disciplinary mix, in terms of all aspects of the project including basic research, intervention design and evaluation.
The issue of selection of discipline representatives in a transdisciplinary effort must be considered in the light of variations within each discipline. For example, there are anthropologists that consider it inappropriate to transform human behavior into numbers and anthropologists who are committed exclusively to mathematical quantification, anthropologists who are post-modernists and those who stand by ecological theory. It is best to avoid assumptions and stereotypes about particular disciplines and assess individuals for their ability to contribute to the collaborative process. Perhaps what most contributed to the success of this transdisciplinary collaboration was that the professionals from the respective disciplines had personal histories of working across disciplines and tended to function on the margins of their own disciplines.
While it may seem trite, interdisciplinary research requires that the people working together from different disciplines like and respect one another. This process can be facilitated by spending work and non-work time together, going to the field together, presenting together, and coming to know each other in the context of families, events, and rituals. Professional and personal tensions are inevitable and perhaps made more difficult by disciplinary and cultural differences; close personal relationships can be particularly advantageous in addressing these problems. Genuine transdisciplinary collaboration is an evolving process requiring attention, re-adjustment, continuing negotiation; personal commitment, and stability—just like a marriage. It must survive in the face of international, societal, institutional, and individual forces, which may not favor and even seek to undermine such relationships. And just like a good marriage, collaborative transdisciplinary work can greatly add to the quality of professional and personal life.
References
Abrams, D. B., & Niaura, R. S. (1987). Social learning theory. In H. T. Blane & K. E. Leonard (Eds.), Psychological theories of drinking and alcoholism (pp. 131–178). New York: Guilford.
Azjen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Barnouw, V. (1963). Culture and personality. Homewood, IL: The Dorsey Press.
Basu, S. (2004). AIDS, empire and public health behaviorism. International Journal of Health Services, 34(1), 1–155.
Beck, A. T. (1976). Cognitive therapy and emotional disorders. New York: International Universities Press.
Bentley, M. E., & Pelto, P. J. (2004). Preface—Ten years of sexuality research and action in India. In R. K. Verma, P. J. Pelto, S. L. Schensul, & A. Joshi (Eds.), Sexuality in the time of AIDS: Contemporary perspectives from communities in India. New Delhi: Sage Publications.
Berger, P. L., & Luckman, T. (1966). The social construction of reality: A treatise in the sociology of knowledge. Garden City, NJ: Doubleday.
Bhugra, D., & deSilva, P. (1995). Sexual dysfunction and sex therapy: An historical perspective. International Review of Psychiatry, 72(2), 2–159.
Blankenship, K. M., Bray, S. J., & Merson, M. H. (2002). Structural interventions in public health. AIDS, 14(Suppl. A), S11–S21.
Bronfenbrenner, U. (1989). Ecological systems theory. In R. Vasta (Ed.), Annals of child development, Vol. 6 (pp. 187–249). Greenwich, CT: JAI Press.
Bronfenbrenner, U. (1999). Environments in developmental perspectives: Theoretical and operational models. In S. L. Friedman & T. D. Wachs (Eds.), Measuring environment across the life span: Emerging methods and concepts (pp. 3–28). Washington, DC: American Psychological Association.
Catania, J. A., Kegeles, S. M., & Coates, T. J. (1990). Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM). Health Education Quarterly, 17(1), 1–53.
Collumbien, M., & Hawkes, S. (2000). Missing men’s messages: Does the reproductive health approach respond to men’s sexual health needs? Culture, Health and Sexuality, 2(2), 135–150.
Dalal, A. K. (2001). Health psychology. In J. Pandey (Ed.), Psychology in India revisited: Development in the discipline: Vol. 2. Personality and health psychology. New Delhi: Sage.
Eberstat, N. (2002). The future of AIDS. Foreign Affairs, 81(6), 6–22.
Ellis, A. (1962). Reason and emotion in psychotherapy. New York: Lyle Stuart.
Eron, J. B., & Lund, T. W. (1996). Narrative solutions in brief therapy. New York: Guilford.
Fisher, J. D., & Fisher, W. A. (2000). Theoretical approaches to individual level change in HIV risk behavior. In J. L. Peterson & R. J. DiClemente (Eds.), Handbook of HIV prevention. New York: Kluwer Academic/Plenum Publishers.
Fisher, W. A., & Fisher, J. D. (1993). A general social psychological model for changing AIDS risk behavior. In J. B. Pryor & G. D. Reeder (Eds.), The social psychology of HIV infection. Hillsdale, NJ: Erlbaum.
Heise, L. L., & Elias, C. (1995). Transforming AIDS prevention to meet women’s needs: A focus on developing countries. Social Science and Medicine, 40(7), 7–931.
Howard, G. S. (1991). Culture tales: A narrative approach to thinking, cross-cultural psychology and psychotherapy. American Psychologist, 46, 187–197.
Janes, C. R., Stall, R., & Gifford, S. M. (1986). Introduction: Medical anthropology and epidemiology. In Anthropology and epidemiology: Interdisciplinary approaches to the study of health and disease. Boston, MA: D. Reidel Publishing Company.
Kakar, S. (1982). Shaman, mystics and doctors: A psychological enquiry into India and its healing traditions. New Delhi: Oxford University Press.
Kakar, S. (1991). The analyst and the mystic. New Delhi: Oxford University Press.
Kegeles, S. M., Hays, R., & Coates, T. J. (1996). The Mpowerment Project: A community-level HIV prevention intervention for young gay men. American Journal of Public Health, 86(8), 8–1129.
Kelly, J. A. (1995). Changing HIV risk behavior: Practical strategies. New York: Guilford.
Kelly, J. A., Lawrence, J., Stevenson, Y., Hauth, A., Kalichman, S., Diaz, Y. et al. (1992). Community AIDS/HIV risk: The effects of endorsements by popular people in three cities. American Journal of Public Health, 82(11), 11–1483.
Kertzer, D. I., & Fricke, T. (1997). Anthropological demography: Toward a new synthesis. Chicago: University of Chicago Press.
Kleinman, A. (1980). Patients and healers in the context of culture. Berkeley, CA: University of California Press.
Kleinman, A. (1986). Social origins of distress and disease. New Haven: Yale University Press.
Kulhara, P., & Avasthi, A. (1995). Sexual dysfunction on the Indian subcontinent. International Review of Psychiatry, 7(2), 2–231.
Kumar, S. (1999). India has the largest number of people infected with HIV. The Lancet, 353(9146), 48.
Leslie, C., & Young, A. (eds.) (1992). Paths to Asian Medical Knowledge. University of California Press
Leviton, L. C. (1996). Integrating psychology and public health: Challenges and opportunities. American Psychologist, 51, 42–51.
Lopez, S. R., & Guarnaccia, P. J. (2000). Cultural psychopathology: Uncovering the social world of mental illness. Annual Review of Psychology, 51, 571–598.
Macro International (2005). Demographic and Health Survey (DHS), from www.measuredhs.com.
Mann, J. M., Tarantola, D. J. M., & Netter, T. W. (1992). AIDS in the world. Cambridge, MA: Harvard University Press.
McNamee, S. (1996). Psychotherapy as a social construction. In H. Rosen & K. Kuehlwein (Eds.), Constructing realities: Meaning-making perspectives for psychotherapists. San Francisco: Jossey-Bass.
McNamee, S., & Gergen, K. J. (1992). Therapy as a social construction. New Park, CA: Sage.
Miller, L. C., Bettencourt, B. A., DeBro, S. C., & Hoffman, V. (1993). Negotiating safer sex: Interpersonal dynamics. In J. B. Pryor & G. D. Reeder (Eds.), The social psychology of HIV infection (pp. 85–123). Hillsdale, NJ: Erlbaum.
Mosley, A. (2004). Does HIV or poverty cause AIDS? Biomedical and epidemiological perspectives. Theoretical Medicine and Bioethics, 25(5–6), 399–421.
NACO. (2004). HIV estimates in India (based on HIV sentinel surveillance), from www.naco.nic.in/indianscene/esthiv.htm
Nastasi, B. K., & Schensul, S. L. (2005). Contributions of qualitative research to the validity of intervention research. Special issue of Journal of School Psychology, 43(3), 3–177.
Nastasi, B. K. (2004). Mental health program evaluation: A multi-component, multi-perspective mixed-method approach. In K. E. Robinson (Ed.), Advances in school-based mental health: Best practices and program models. Kingston, NJ: Civic Research Institute.
Nastasi, B. K., Moore, R. B., & Varjas, K. M. (2004). Creating comprehensive and culturally specific programs. Washington, DC: American Psychological Association.
Nastasi, B. K., Schensul, J. J., deSilva, M. W. A., Varjas, K., Silva, K. T., Ratnayake, P. et al. (1998–1999). Community based sexual risk prevention program for Sri Lankan youth: Influencing sexual-risk decision making. International Quarterly of Community Health Education, 18(1), 1–139.
Nastasi, B. K., Varjas, K., Berstein, R., & Jayasena, A. (2000). Conducting participatory culture-specific consultation: A global perspective on multicultural consultation. School of Psychology Quarterly, 29(3), 3–401.
Nastasi, B. K., Varjas, K., Schensul, S. L., Silva, K. T., Schensul, J. J., & Ratnayake, P. (2000). The participatory intervention model: A framework for conceptualizing and promoting intervention acceptability. School of Psychology Quarterly, 15, 207–232.
Pelto, P. J., Joshi, A., & Verma, R. K. (1999). The development of Indian male sexuality. Population Council: South and Southeast Asian Regional Office.
Pelto, P. J., & Pelto, G. H. (1997). Studying knowledge, culture and behavior in applied medical anthropology. Medical Anthropology Quarterly, 11(2), 149–163.
Prochaska, J., & DiClemente, C. (1992). Stages of change in the modification of problem behaviors. Progress in behavior modification. Progress in Behavior Modification, 28, 183–218.
Rhodes, T., Singer, M., Bourgois, P., Friedman, S. L., & Strathdee, S. (2005). The social and structural production of HIV risk among injecting drug users. Social Science and Medicine, 61, 1026–1044.
Rogers, E. M. (1983). Diffusion of Innovations. New York: The Free Press.
Rosenfield, P. L. (199). The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Social Science and Medicine, 35(11), 11–1343–1357.
Rosenstock, I, Strecher, V., & Becker, M. (1988). Social learning theory and ther health belief model. Heath Education Quarterly 15(2), 75–83.
Sarbin, T. (1986). Narrative psychology: The storied nature of human conduct. New York: Praeger.
Schensul, S. L., Mekki-Berrada, Saggurti, N., Nastasi, B. K., Verma, R. K. (2006). Healing traditions and men’s sexual health in Mumbai, India: The realities of practiced medicine in urban poor communities in India. Social Science and Medicine.
Schensul, J. J., & LeCompte, M. (1999). Ethnographer’s toolkit. Walnut Creek, CA: AltaMira Press.
Schensul, S. L., Schensul, J. J., & LeCompte, M. (1999). Essential ethnographic methods. Walnut Creek, CA: AltraMira Press.
Schensul, S. L., Verma, R. K., & Nastasi, B. K. (2004). Responding to men’s sexual concerns: research and intervention in slum communities in Mumbai, India. International Journal of Men’s Health, 3(3), 197–220.
Scientific Software Development. (2004). ATLAS.ti 5.0 [Computer software]. Berlin, Germany: Author. [website: http://www.atlasti.com]
Sherif, M. (1963). Social psychology: problems and trend in interdisciplinary relationships. In S. Koch (Ed.), A study of science, Vol. 6 - Investigation of man as socius: Their place in psychology and the social sciences. New York: McGraw Hill.
Silva, K. T., Schensul, S. L., Schensul, J. J., Nastasi, B. K., deSilva, M. W. A., Sivayoganathan, C. et al. (1997). Youth and sexual risk in Sri Lanka. Women and AIDS research program phase II. Research report series no. 3. Washington, DC: International Center for Research on Women.
Singh, A. K. (1984). Health modernity: concept and correlates. Social Change, 14, 3–16.
Sue, D. W., Bingham, R. P., Porche-Burke, L., & Vasquez, M. (1999). The diversification of psychology: A multiple revolution. American Psychologist, 54, 1061–1069.
Trostle, J. (2005). Epidemiology and Culture. New York: Cambridge University Press.
UNAIDS. (2001). The global strategy framework on HIV/AIDS. Geneva: Switzerland.
Verma, R. K. (2003). Male sexual health concerns and it’s implications: research findings from community-based studies in Mumbai. In A. Mahajan (Ed.), Perspectives on culturally-based concepts of semen loss: A key to prevention of STIs/HIV. Baroda: Deepak Charitable Trust.
Verma, R. K., Khaitan, B. K., & Singh, O. P. (1998). The frequency of sexual dysfunctions in patients attending a sex therapy clinic in North India. Archives of Sexual Behavior, 27(3), 309–313.
Verma, R. K., Rangaiyan, G., Singh, R., Sharma, S., & Pelto, P. J. (2001). A study of male sexual health problems in a Mumbai slum population. Culture, Health and Sexuality, 3(3), 339–352.
Verma, R. K., & Schensul, S. L. (2004). Male sexual health problems in Mumbai: Cultural constructs that present opportunities for HIV/AIDS risk education. In R. K. Verma, P. J. Pelto, S. L. Schensul & A. Joshi (Eds.), Sexuality in the time of AIDS: Contemporary perspectives from communities in India (pp. 1–431). New Delhi: Sage Publications.
Verma, R. K., Sharma, S., Rangaiyan, G., Singh, R., & Pelto, P. J. (2003). Beliefs concerning male sexual health problems and treatment seeking among men in Mumbai slums. Culture, Health and Sexuality, 3(May–June), 165–173.
Vygotsky, L. S. (1978). Mind in society: The development of higher psychological processes. Cambridge, MA: Harvard University Press.
Wallace, A. F. C. (1961). Culture and personality. New York: Random House.
Wallace, A. F. C. (1970). Culture and personality. New York: Random House.
Weller, S., & Romney, A. (1988). Systematic data collection. In J. Maaren, P. Manning & M. Miller (Eds.), Qualitative research methods. Thousand Oaks, CA: Sage Publications.
Wertsch, J. V. (1991). Voices of the mind: A sociocultural approach to mediated action. Cambridge, MA: Harvard University Press.
World Health Organization/Global Programme on AIDS/STD. (1993). Recommendations for the management of sexually transmitted diseases. Geneva: World Health Organization.
Acknowledgement
The data presented in this paper is drawn from an Indo-U.S. collaborative project funded by a grant from the National Institute for Mental Health (1RO1-MH64875, S. Schensul PI). The authors would like to thank Prof. Pertti J. Pelto (University of Connecticut, Emeritus) who provided the base for this project through his commitment to the training and development of transdisciplinary researchers in India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schensul, S.L., Nastasi, B.K. & Verma, R.K. Community-Based Research in India: A Case Example of International and Transdisciplinary Collaboration. Am J Community Psychol 38, 95–111 (2006). https://doi.org/10.1007/s10464-006-9066-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-006-9066-z