Abstract
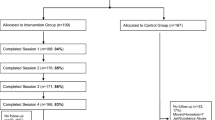
HIV risk among transgender women has been attributed to condomless sex with primary male partners. This study pilot tested a couples-focused HIV intervention program for transgender women and their primary male partners. We analyzed data from 56 transgender women and their male partners (n = 112 participants) who were randomized as a couple to one of two groups. Participants in the intervention group (27 couples) received 3 counseling sessions: 2 couples-focused sessions, which discussed relationship dynamics, communication, and HIV risk, and 1 individual-focused session on HIV prevention concerns. Participants in the control group (29 couples) received 1 session on general HIV prevention information delivered to both partners together. At 3-month follow-up, participants in the intervention reported lower odds of condomless sex with primary partners (OR 0.5, 95 % CI 0.3–1.0), reduced odds of engaging in sex with a casual partner (OR 0.3, 95 % CI 0.1–1.0), and reduction in the number of casual partners (B = −1.45, SE = 0.4) compared with the control group. Findings provide support for the feasibility and promise of a couples-focused HIV prevention intervention for transgender women and their primary male partners.
Resumen
El riesgo para el VIH entre mujeres transgénero ha sido atribuido a sexo sin condón durante relaciones sexuales con parejas masculinas primarias. Este estudio piloto probó un programa de intervención enfocado en parejas para prevenir el VIH entre mujeres transgénero y sus parejas masculinas primarias. Se analizaron los datos de 56 mujeres transgénero y sus parejas masculinas (n = 112 participantes) quienes fueron asignados al azar como pareja a uno de dos grupos. Los participantes en el grupo de intervención (27 parejas) recibieron 3 sesiones de consejería: 2 sesiones enfocadas en parejas, en la cual se discutió dinámicas de la relación, comunicación, y riesgo para el VIH, y 1 sesión individual centrada en preocupaciones relacionadas con la prevención del VIH. Los participantes en el grupo de control (29 parejas) recibieron 1 sesión enfocada en parejas sobre información general acerca de prevención del VIH. A los 3 meses de seguimiento, los participantes en la intervención reportaron probabilidades más bajas de sexo sin condón con parejas primarias (OR 0.5, 95 % CI 0.3–1.0), menores probabilidades de tener relaciones sexuales con una pareja ocasional (OR 0.3, 95 % CI 0.1–1.0), y reducción en el número de parejas ocasionales (B = −1.45, SE = 0.4) en comparación con el grupo control. Estos resultados proporcionan apoyo a la viabilidad y promesa de una intervención enfocada en parejas para prevenir el VIH entre mujeres transgénero y sus parejas masculinas primarias.

Similar content being viewed by others
References
Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17.
Poteat T, Wirtz AL, Borquez A, et al. HIV risk and prevention interventions in transgender women sex workers. Lancet Infect Dis. 2015;385(9964):274–86.
Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22.
Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV risk behaviors among male-to-female transgender persons of color in San Francisco. Am J Public Health. 2004;94:1193–9.
Bockting WO, Robinson BE, Rosser BR. HIV prevention: a qualitative needs assessment. AIDS Care. 1998;10:505–25.
Melendez RM, Pinto R. It’s a really hard life’: love, gender and HIV risk among male-to-female transgender persons. Cult Health Sex. 2007;9:233–45.
Bockting W, Miner M, Rosser BR. Latino men’s sexual behavior with transgender persons. Arch Sex Behav. 2007;36:778–86.
Operario D, Burton J, Underhill K, Sevelius J. Men who have sex with transgender women: Challenges to category-based HIV prevention. AIDS Behav. 2008;12:18–26.
Operario D, Nemoto T, Iwamoto M, Moore T. Risk for HIV and unprotected sexual behavior in male primary partners of transgender women. Arch Sex Behav. 2011;40(6):1255–61.
Rosser BS, Oakes JM, Bockting WO, Miner M. Capturing the social demographics of hidden sexual minorities: an Internet study of the transgender population in the United States. Sex Res Soc Policy. 2007;4(2):50–64.
Institute of Medicine (IOM). The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington: National Academic Press; 2011.
Hoff CC, Beougher SC, Chakravarty D, Darbes LA, Neilands TB. Relationship characteristics and motivations behind agreements among gay male couples: differences by agreement type and couple serostatus. AIDS Care. 2010;22(7):827–35.
Amaro H. Considering women’s realities in HIV prevention. Am Psychol. 1995;50(6):437.
Golub SA, Starks TJ, Payton G, Parson JT. The critical role of intimacy in the sexual behaviors of gay and bisexual men. AIDS Behav. 2012;16(3):626–32.
Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the porportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–62.
Hoff CC, Chakravarty D, Beougher SC, Darbes LA, Dadasovich R, Neilands TB. Serostatus differences and agreements about sex with outside partners among gay male couples. AIDS Educ Prev. 2009;21(1):25–38.
Gamarel KE, Reisner SL, Darbes LA, et al. Dyadic dynamics of HIV risk among transgender women and their primary male sexual partners: the role of sexual agreement types and motivations. AIDS Care 2016;28(1):104–11.
El-Bassel N, Gilbert L, Witte S, Wu E, Hunt T, Remien RH. Couples-based HIV prevention in the United States: Advantages, gaps, and future directions. J Acquir Immun Def Syn. 2010;55:S92–101.
Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS Behav. 2010;14(1):1–10.
El-Bassel N, Witte SS, Gilbert L, et al. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93(6):963–9.
Wu E, El-Bassel N, McVinney LD, et al. Feasibility and promise of a couples-based HIV/STI prevention intervention for methampetamine-using Black men who have sex with men. AIDS Behav. 2011;15(8):1745–54.
El-Bassel N, Witte S, Gilbert L, et al. HIV prevention for intimate couples: a relationship-based model. Fam Syst Health. 2001;19(4):379–95.
Larzelere RE, Huston TL. The dyadic trust scale: towards understanding interpersonal trust in close relationships. J Marriage Fam. 1980;42(3):595–604.
Sherman SG, Gielen AC, McDonnell KA. Power and attitudes in relationship (PAIR) scale among a sample of low-income, African American women: implications for HIV/AIDS prevention. Sex Roles. 2000;42:283–94.
Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. J Am Coll Health. 1992;39(5):219–25.
Milhausen RR, Sales JM, Wingood GM, DiClemente RJ, Salazar LF, Crosby RA. Validation of a partner sexual communication scale for use in HIV/AIDS prevention interventions. J HIV/AIDS Prev Child Youth. 2007;8(1):11–33.
Sabin CA, Cozzi A, Phillips AN. a practical guide to applying the intention-to-treat principle to clinical trials in HIV infection. HIV Clin Trials. 2000;1:31–8.
Saha C, Jones MP. Bias in the last observation carried forward method under informative dropout. J Stat Plan Inference. 2009;139(2):246–55.
World Health Organization (WHO). Guidance on couples HIV testing and counselling–including antiretroviral therapy for treatment and prevention in serodiscordant couples: recommendations for a public health approach. Geneva: WHO HIV/AIDS Programme; 2012.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. New England J Med. 2011;365(6):493–505.
Ware NC, Wyatt MA, Haberer JE, et al. What’s love got to do with it? Explaining adherence to oral antiretroviral pre-exposure prophylaxis (PrEP) for HIV serodiscordant couples. J Acquir Immun Def Syn. 2012;59(5):463–68.
Schumm JA, O’Farrell TJ, Kahler CW, Murphy MM, Muchowski P. A randomized clinical trial of behavioral couples therapy versus individually based treatment for women with alcohol dependence. J Consult Clin Psychol. 2014;82(6):993–1004.
Denton WH, Wittenborn AK, Golden RN. Augmenting antidepressant medication treatment of depressed with with emotionally focused therapy for couples: a randomized pilot study. J Marital Fam Ther. 2012;38(S1):23–38.
McMahon JM, Pouget ER, Tortu S, Volpe EM, Torres L, Rodrigue W. Couples-based HIV counseling and testing: a risk reduction intervention for US drug-involved women and their primary male partners. Prev Sci. 2015;16(2):341–51.
Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19(8):807–14.
Funding
This study was funded by NIH Grants R34MH093232 and U24AA022000. Support was also provided by T32MH07878 and P30AI042853
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Operario, D., Gamarel, K.E., Iwamoto, M. et al. Couples-Focused Prevention Program to Reduce HIV Risk Among Transgender Women and Their Primary Male Partners: Feasibility and Promise of the Couples HIV Intervention Program. AIDS Behav 21, 2452–2463 (2017). https://doi.org/10.1007/s10461-016-1462-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1462-2