Abstract
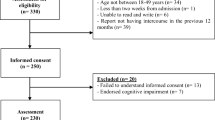
Substance-abusing pregnant and postpartum women are less likely to maintain consistent condom use and drug and alcohol abstinence, which is particularly concerning in high HIV-prevalence areas. Data from 224 pregnant and postpartum women in substance abuse treatment were analyzed to examine effects of history of substance use, child abuse, and mental health problems on current substance use and condom-use barriers. Mediators were depression, relationship power and social support. Most participants (72.9 %) evidenced current depression. Less social support (−0.17, p < 0.05) and relationship power (−0.48, p < 0.001), and greater depression (−0.16, p < 0.05) predicted more condom-use barriers. History of mental health problems predicted condom-use barriers, mediated by recent depression and relationship power (0.15, p < 0.001). These findings suggest depression and diminished relationship power limit highest-risk women’s ability to negotiate condom use and abstain from substance use, increasing their risk of acute HIV infection and vertical transmission.
Resumen
Las mujeres embarazadas o en el postparto que abusan de sustancias adictivas tienden a ser menos propicias a perseverar en el uso consistente del condón y en el abstenerse del uso de las drogas y alcohol, circunstancias particularmente preocupantes en regiones con alta prevalencia de VIH. Datos de 224 mujeres embarazadas y en el postparto en tratamiento para al abuso de sustancias se analizaron para examinar los efectos de un historial de abuso de sustancias, abuso infantil, y problemas de salud mental en su uso actual de sustancias adictivas y su reporte de barreras al uso del condón. Factores que mediaban dichas relaciones eran la depresión, el poder en la relación íntima, y la percepción de apoyo social. La mayoría de las participantes (72.9 %) exhibían una depresión en el periodo de estudio. Menos apoyo social (−0.17, p < 0.05) y poder en su relación íntima (−0.48, p < 0.001), y severidad de la depresión (−0.16, p < 0.05) predecían más barreras al uso del condón. Un historial de problemas de salud mental predecía barreras al uso del condón, mediado por depresión reciente y menos poder en la relación íntima (0.15, p < 0.001). Estos hallazgos sugieren que la depresión y el déficit de poder en la relación íntima limitan la habilidad de las mujeres en más alto riesgo de poder negociar el uso del condón y evitar el uso de sustancias adictivas, aumentando su riesgo de infección aguda por el VIH y de la transmisión vertical.

Similar content being viewed by others
References
Centers for Disease Control and Prevention (CDC). HIV surveillance report, 2011. http://www.cdc.gov/hiv/topics/surveillance/resources/reports/23 (2013).
El-Sadr WM, Mayer KH, Hodder SL. AIDS in America: forgotten but not gone. N Engl J Med. 2010;362(11):967.
CDC. HIV/AIDS data through December 2008 provided for the Ryan White HIV/AIDS Treatment Extension Act of 2009, for fiscal year 2010. HIV Surveillance Supplemental Report. http://www.cdc.gov/hiv/pdf/statistics_2009_HIV_Surveillance_Report_vol_17_no1.pdf (2012).
White House Office of National AIDS Policy and Advisor on Violence Against Women. Addressing the Intersection of HIV/AIDS, Violence against Women and Girls, & Gender Related Health Disparities. http://www.whitehouse.gov/blog/2013/09/06/addressing-intersection-hivaids-violence-against-women-and-girls-and-gender-related (2013).
Lemly DC, Shepherd BE, Hulgan T, et al. Race and sex differences in antiretroviral therapy use and mortality among HIV-infected persons in care. J Infect Dis. 2009;199(7):991–8.
Health Resources and Services Administration. HRSA CARE action newsletter: ryan white providers address HIV/AIDS among African American women. http://hab.hrsa.gov/newspublications/careactionnewsletter/sept2012.pdf (2012).
Denning P, DiNenno E. Communities in crisis: is there a generalized HIV epidemic in impoverished urban areas of the United States? http://origin.glb.cdc.gov/hiv/risk/other/poverty.html (2014).
Wyatt GE, Gómez CA, Hamilton AB, Valencia-Garcia D, Gant LM, Graham CE. The intersection of gender and ethnicity in HIV risk, interventions, and prevention: new frontiers for psychology. Am Psychol. 2013;68(4):247.
Richardson ET, Collins SE, Kung T, et al. Gender inequality and HIV transmission: a global analysis. J Int AIDS Soc. 2014;17:19035.
Russell BS, Eaton LA, Petersen-Williams P. Intersecting epidemics among pregnant women: alcohol use, interpersonal violence, and HIV infection in South Africa. Curr HIV/AIDS Rep. 2013;10(1):103–10.
Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. 1996;24(2):99.
Rosenberg R, Malow R. The hard science of hard risks in women’s HIV prevention: making biology part of the context. In: Pope C, White R, Malow R, editors. HIV/AIDS: global frontiers in prevention/intervention. New York: Routledge; 2009. p. 73–81.
Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17:18845.
Tsai AC, Weiser SD. Population-based study of food insecurity and HIV transmission risk behaviors and symptoms of sexually transmitted infections among linked couples in Nepal. AIDS Behav. 2014;18(11):2187–97.
Kinuthia J, Drake A, Matemo D, Richardson B, McClelland RS, John-Stewart G. Incidence and cofactors of acute HIV during pregnancy and postpartum. Conference on retroviruses and opportunistic infections (CROI) Boston, Massachusetts; 2014.
Kouyoumdjian FG, Findlay N, Schwandt M, Calzavara LM. A systematic review of the relationships between intimate partner violence and HIV/AIDS. PLoS One. 2013;8(11):e81044.
Teitelman AM, Ratcliffe SJ, Morales-Aleman MM, Sullivan CM. Sexual relationship power, intimate partner violence, and condom use among minority urban girls. J Interpers Viol. 2008;23(12):1694–712.
Amaro H. Love, sex, and power. Considering women’s realities in HIV prevention. Am Psychol. 1995;50(6):437–47.
Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: evidence and possible underlying psychological processes. Rev Gen Psychol. 1997;1(1):72.
Ramsey SE, Bell KM, Engler-Field PA. HIV risk behavior among female substance abusers. J Addict Dis. 2010;29(2):192–9.
Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7–8):637–60.
Campbell AN, Tross S, Hu MC, Pavlicova M, Nunes EV. Predictors of relationship power among drug-involved women. AIDS Behav. 2012;16(6):1532–41.
Campbell AN, Tross S, Dworkin SL, et al. Relationship power and sexual risk among women in community-based substance abuse treatment. J Urban Health. 2009;86(6):951–64.
Matsuda Y, McGrath JM, Jallo N. Use of the sexual relationship power scale in research: an integrative review. Hisp Health Care Int. 2012;10(4):175–89.
Nduna M, Jewkes RK, Dunkle KL, Shai NP, Colman I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc. 2010;13(1):44.
Higgins JA, Mathur S, Eckel E, et al. Importance of relationship context in HIV transmission: results from a qualitative case-control study in Rakai, Uganda. Am J Publ Health. 2014;104(4):612–20.
Woolf-King SE, Maisto SA. The effects of alcohol, relationship power, and partner type on perceived difficulty implementing condom use among African American adults: an experimental study. Arch Sex Behav. 2014;44:1–11.
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–21.
Kershaw TS, Small M, Joseph G, Theodore M, Bateau R, Frederic R. The influence of power on HIV risk among pregnant women in rural Haiti. AIDS Behav. 2006;10(3):309–18.
Hatcher AM, Tsai AC, Kumbakumba E, et al. Sexual relationship power and depression among HIV-infected women in rural Uganda. PLoS One. 2012;7(12):e49821.
Miami-Dade Community Action Agency. Comprehensive community needs assessment. http://metropolitan.fiu.edu/research/economic-and-demographic-research/1279547400_caa_presentation.pdf (2008).
Miami Dade County. Miami-Dade County Workforce Housing Plan, 2008 to 2015. http://www.docstoc.com/docs/48121891/Miami-Dade-County-Workforce-Housing-Plan-2008-to-2015 (2008).
Carey MP, Carey K, Maisto S, Gordon C, Weinhardt L. Assessing sexual risk behaviour with the timeline followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS. 2001;12(6):365–75.
Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. Adv Pers relatsh. 1987;1(1):37–67.
Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress 1. J Appl Soc Psychol. 1983;13(2):99–125.
Cohen S, Mermelstein R, Kamarck T, Hoberman H. Interpersonal support evaluation list. In: Sarason I, Sarason B, editors. Social support: theory, research and application. Washington DC: Martinus Nijhoff; 1985. p. 77–94.
Radloff LS, Locke BZ. The community mental health assessment survey and the CES-D scale. Community Surv Psychiatr Disord. 1986;4:177–88.
Van Dam NT, Earleywine M. Validation of the center for epidemiologic studies depression scale—revised (CESD-R): pragmatic depression assessment in the general population. Psychiatry Res. 2011;186(1):128–32.
Lawrence JSS, Chapdelaine AP, Devieux JG, O’Bannon RE, Brasfield TL, Eldridge GD. Measuring perceived barriers to condom use: psychometric evaluation of the condom barriers scale. Assessment. 1999;6(4):391–404.
Yuan K-H, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24:71–83.
EQS. Multivariate software (computer program). Encino: Multivariate Software Inc; 2006.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55.
Chou C-P, Bentler PM. Model modification in covariance structure modeling: a comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivar Behav Res. 1990;25(1):115–36.
Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
MacCallum R. Specification searches in covariance structure modeling. Psychol Bull. 1986;100(1):107.
American College of Obstetricians Gynecologists Committee on Health. Care for underserved women. AGOG Committee Opinion No. 473: substance abuse reporting and pregnancy: the role of the obstetrician-gynecologist. Obstet Gynecol. 2011;117(1):200–1.
Terplan M, McNamara EJ, Chisolm MS. Pregnant and non-pregnant women with substance use disorders: the gap between treatment need and receipt. J Addict Dis. 2012;31(4):342–9.
Cohen MS, Shaw GM, McMichael AJ, Haynes BF. Acute HIV-1 infection. N Engl J Med. 2011;364(20):1943–54.
Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. Women and infants transmission study group. N Engl J Med. 1999;341(6):394–402.
Reece M, Herbenick D, Schick V, Sanders SA, Dodge B, Fortenberry JD. Condom use rates in a national probability sample of males and females ages 14 to 94 in the United States. J Sex Med. 2010;7(s5):266–76.
Davis KC, Schraufnagel TJ, Kajumulo KF, Gilmore AK, Norris J, George WH. A qualitative examination of men’s condom use attitudes and resistance:“it’s just part of the game”. Arch Sex Behav. 2014;43(3):631–43.
Harvey SM, Bird ST, Galavotti C, Duncan EA, Greenberg D. Relationship power, sexual decision making and condom use among women at risk for HIV/STDs. Women Health. 2002;36(4):69–84.
Pulerwitz J, Amaro H, Jong WD, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800.
Minieri AM, Staton-Tindall M, Leukefeld C, Clarke JG, Surratt HL, Frisman LK. Relationship power as a mediator of intimate partner violence and mental health issues among incarcerated, substance-using women. Int J Offender Ther Comp Criminol. 2014;58(3):303–19.
Seth P, Raiji PT, DiClemente RJ, Wingood GM, Rose E. Psychological distress as a correlate of a biologically confirmed STI, risky sexual practices, self-efficacy and communication with male sex partners in African-American female adolescents. Psychol Health Med. 2009;14(3):291–300.
Wingood GM, DiClemente RJ. The effects of an abusive primary partner on the condom use and sexual negotiation practices of African-American women. Am J Publ Health. 1997;87(6):1016–8.
Qiao S, Li X, Stanton B. Social support and HIV-related risk behaviors: a systematic review of the global literature. AIDS Behav. 2014;18(2):419–41.
Lippman SA, Donini A, Díaz J, Chinaglia M, Reingold A, Kerrigan D. Social-environmental factors and protective sexual behavior among sex workers: the encontros intervention in Brazil. Am J Publ Health. 2010;100(S1):S216–23.
Neblett RC, Davey-Rothwell M, Chander G, Latkin CA. Social network characteristics and HIV sexual risk behavior among urban African American women. J Urban Health. 2011;88(1):54–65.
Fullilove MT, Fullilove RE III, Haynes K, Gross S. Black women and AIDS prevention: a view towards understanding the gender rules. J Sex Res. 1990;27(1):47–64.
Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Women’s Health. 2003;12(4):373–80.
Steiner M, Dunn E, Born L. Hormones and mood: from menarche to menopause and beyond. J Affect Disord. 2003;74(1):67–83.
Friedman SH, Loue S. Incidence and prevalence of intimate partner violence by and against women with severe mental illness. J Women’s Health. 2007;16(4):471–80.
Rosenberg R, Malow R. Hardness of risk: poverty, women and new targets for HIV/AIDS prevention. Psychol AIDS Exch. 2006;34:3–4.
Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27(5):539–65.
Crosby RA, DiClemente RJ, Wingood GM, et al. Sexual agency versus relational factors: a study of condom use antecedents among high-risk young African American women. Sex Health. 2008;5(1):41–7.
El-Bassel N, Gilbert L, Wu E, Go H, Hill J. HIV and intimate partner violence among methadone-maintained women in New York City. Soc Sci Med. 2005;61(1):171–83.
Rosenthal L, Levy SR. Understanding women’s risk for HIV infection using social dominance theory and the four bases of gendered power. Psychol Women Q. 2010;34(1):21–35.
El-Bassel N, Caldeira NA, Ruglass LM, Gilbert L. Addressing the unique needs of African American women in HIV prevention. Am J Publ Health. 2009;99(6):996.
O’Leary KD. Developmental and affective issues in assessing and treating partner aggression. Clin Psychol. 1999;6(4):400–14.
Connell RW. Gender and power: society, the person and sexual politics. Stanford: Stanford University Press; 1987.
Niccolai LM, Ethier KA, Kershaw TS, Lewis JB, Ickovics JR. Pregnant adolescents at risk: sexual behaviors and sexually transmitted disease prevalence. Am J Obstet Gynecol. 2003;188(1):63–70.
Koniak-Griffin D, Stein JA. Predictors of sexual risk behaviors among adolescent mothers in a human immunodeficiency virus prevention program. J Adolesc Health. 2006;38(3):297. e291-297. e211.
Sales J, DiClemente R, Davis T, Sullivan S. Exploring why young African American women do not change condom-use behavior following participation in an STI/HIV prevention intervention. Health Educ Res. 2012;27(6):1091–101.
Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatr Clin N Am. 1999;22(2):241–52.
Strain EC. Assessment and treatment of comorbid psychiatric disorders in opioid-dependent patients. Clin J Pain. 2002;18(4):S14–27.
Higgins PG, Clough DH, Frank B, Wallerstedt C. Changes in health behaviors made by pregnant substance users. Subst Use Misuse. 1995;30(10):1323–33.
Kershaw TS, Magriples U, Westdahl C, Rising SS, Ickovics J. Pregnancy as a window of opportunity for HIV prevention: effects of an HIV intervention delivered within prenatal care. Am J Publ Health. 2009;99(11):2079.
Abdool Karim Q, Humphries H, Stein Z. Empowering women in human immunodeficiency virus prevention. Best Pract Res Clin Obstet Gynaecol. 2012;26(4):487–93.
Abdool Karim SS, Baxter C. Antiretroviral prophylaxis for the prevention of HIV infection: Future implementation challenges. Future Med. 2009;3(1):3–6.
Lennon CA, Huedo-Medina TB, Gerwien DP, Johnson BT. A role for depression in sexual risk reduction for women? A meta-analysis of HIV prevention trials with depression outcomes. Soc Sci Med. 2012;75(4):688–98.
Brown JL, Sales JM, Swartzendruber AL, Eriksen MD, DiClemente RJ, Rose ES. Added benefits: reduced depressive symptom levels among African-American female adolescents participating in an HIV prevention intervention. J Behav Med. 2013;37:1–9.
Yonkers KA, Blackwell KA, Glover J, Forray A. Antidepressant use in pregnant and postpartum women. Annu Rev Clin Psychol. 2014;10:369–92.
Logan T, Cole J, Leukefeld C. Women, sex, and HIV: social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychol Bull. 2002;128(6):851.
Acknowledgments
This study was funded by Grant 5 RO1 DA021521 from the National Institute of Drug Abuse. Data used for this study was collected from participants in a group level, HIV risk reduction intervention in Miami, Florida, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No authors report any conflict of interest associated with this manuscript.
Rights and permissions
About this article
Cite this article
Dévieux, J.G., Jean-Gilles, M., Rosenberg, R. et al. Depression, Abuse, Relationship Power and Condom Use by Pregnant and Postpartum Women with Substance Abuse History. AIDS Behav 20, 292–303 (2016). https://doi.org/10.1007/s10461-015-1176-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1176-x