Abstract
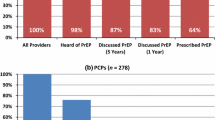
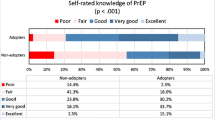
The FDA approval of emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis (PrEP) in 2012 has raised questions about the delivery of PrEP in a real-world setting. iPad-based questionnaires were given to providers at conferences in California and New York to assess knowledge, experience and attitudes regarding PrEP in HIV and non-HIV providers. HIV provider status was defined either by self-identification or by having greater than 5 years of HIV care experience. Knowledge scores were the sum of correct answers from five PrEP knowledge questions. Univariate analyses used t-test to compare knowledge scores and Fisher’s exact test for past or future PrEP prescription between HIV and non-HIV providers. Multivariable linear or logistic regression models were used to assess factors associated with the outcomes. Of 233 respondents, the mean age was 40 years, 59 % were White, 59 % were physicians and 52 % were HIV providers. In univariate analysis, mean PrEP knowledge scores (max 5) were significantly higher for HIV providers (2.8 versus 2.2; p < 0.001), age > 41 (mean 2.8 versus 2.3; p = 0.004), White race (2.7 versus 2.2; p = 0.026) and participants in the New York region (3.0 versus 2.3; p < 0.001). In a multivariable model of knowledge scores, all but age remained significant. Among 201 potential prescribers, the rate of prior PrEP prescription was higher among HIV providers than non-HIV providers (34 versus 9 %; p < 0.001) and by knowledge score, but the association with provider status was no longer significant in multivariable analysis that controlled for knowledge. Intent to prescribe PrEP in the future was high for all provider types (64 %) and was associated with knowledge scores in multivariable analysis. The most common concerns about PrEP (>40 % of providers) were drug toxicities, development of resistance and patient adherence to follow-up; 32 % identified risk compensation as a concern. HIV providers had significantly greater PrEP knowledge than non-HIV providers, but differences by provider type in past PrEP prescription were largely dependent on knowledge. Future PrEP prescription was also associated with knowledge, though all providers expressed greater future use. Education of potential PrEP providers will be a key component of successful PrEP implementation.
Resumen
La aprobación de Emtricitabina/Fumarato de Disoproxilo de Tenofovir por la FDA para PrEP en 2012 ha originado preguntas acerca del suministro de profilaxis pre-exposición (PrEP) en un escenario real. Cuestionarios a través de dispositivo iPad fueron proporcionados a proveedores de salud especialistas en VIH y proveedores de salud en general durante conferencias en California y Nueva York para evaluar conocimiento, experiencia y actitudes en cuanto a PrEP. La categoría de proveedor de salud especialista en VIH fue definida por identificación propia o por tener más de cinco años de experiencia en el cuidado de VIH. Los marcadores de conocimiento fueron la suma de respuestas correctas a cinco preguntas de conocimiento sobre PrEP. El análisis univariado utilizó la prueba t-test para comparar los marcadores de conocimiento y la prueba exacta Fisher se utilizó para pasadas o futuras prescripciones médicas de PrEP entre proveedores de salud especialistas en VIH y proveedores de salud en general. Los modelos linear multivariable o de regresión logística fueron utilizados para evaluar factores asociados con los resultados. De 233 encuestados, la edad promedio fue 40 años, 59 % fueron raza Blanca, 59 % fueron médicos y 52 % fueron proveedores de salud especialistas en VIH. En análisis univariado, el promedio en el marcador de de conocimientos sobre PrEP (max 5) fue significativamente mayor para proveedores de salud especialistas en VIH (en un 2.8 versus 2.2; p<0.001), edad >41 (promedio 2.8 versus 2.3; p=0.004), raza blanca (2.7 versus 2.2; p=0.0.26) y los participantes de la region de Nueva York (3.0 versus 2.3; p<0.001). En el modelo multivariable de marcadores de conocimiento, todo excepto la edad permaneció significantivo. Entre 201 potenciales proveedores que prescribirán una receta médica para PrEP, el índice de haber prescrito con aterioridad fue mayor entre proveedores de salud especialistas en VIH que en los proveedores de salud en general (34 % versus 9 %; p<0.001) en cuanto a marcador de conocimiento, la asociacion de la categoría de los proveedores de salud no fue significantiva en el anáslisis multivariable que controló el conocimiento. Los planes de prescribir PrEP en un futuro fue mayor para los dos tipos de proveedores de salud (64 %) y estuvo asociada con los marcadores de conocmiento en el análisis multivariable. Las preocupaciones más communes en cuanto a PrEP (>40 % de los proveedores) fue la toxicidad del medicamento, desarrollo de Resistencia y la adherencia o apego de parte del paciente; 32 % identificaron a la compensación de riesgo como una preocupación. Proveedores de salud especialistas en VIH tuvieron un conocimiento de PrEP significativamente mayor que los proveedores de salud en general, pero las diferencias entre los tipos de proveedor en prescripciones médicas de PrEP anteriores fueron ampliamente dependientes del conocimiento. Prescripciones médicas de PrEP futuras fue asociado con conocimiento, sin embargo todos los proveedores expresaron una mayor utilización en el futuro. La educación sobre PrEP en proveedores de salud será un componente clave en el éxito de la implementación de PrEP.
Similar content being viewed by others
References
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. doi:10.1056/NEJMoa1110711.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi:10.1056/NEJMoa1011205.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi:10.1056/NEJMoa1108524.
FDA. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm312210.htm 2012. Accessed 12 March 2013.
Tripathi A, Ogbuanu C, Monger M, Gibson JJ, Duffus WA. Preexposure prophylaxis for HIV infection: healthcare providers’ knowledge, perception, and willingness to adopt future implementation in the southern US. South Med J. 2012;105(4):199–206. doi:10.1097/SMJ.0b013e31824f1a1b.
White JM, Mimiaga MJ, Krakower DS, Mayer KH. Evolution of Massachusetts physician attitudes, knowledge, and experience regarding the use of antiretrovirals for HIV prevention. AIDS Patient Care STDs. 2012;26(7):395–405. doi:10.1089/apc.2012.0030.
Puro V, Palummieri A, De Carli G, Piselli P, Ippolito G. Attitude towards antiretroviral pre-exposure prophylaxis (PrEP) prescription among HIV specialists. BMC Infect Dis. 2013;13:217. doi:10.1186/1471-2334-13-217.
Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704–12. doi:10.1093/cid/cit796.
Mimiaga MJ, White JM, Krakower DS, Biello KB, Mayer KH. Suboptimal awareness and comprehension of published preexposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26(6):684–93. doi:10.1080/09540121.2013.845289.
Wimberly YH, Hogben M, Moore-Ruffin J, Moore SE, Fry-Johnson Y. Sexual history-taking among primary care physicians. J Natl Med Assoc. 2006;98(12):1924–9.
Kurth AE, Holmes KK, Hawkins R, Golden MR. A national survey of clinic sexual histories for sexually transmitted infection and HIV screening. Sex Transm Dis. 2005;32(6):370–6.
Laws MB, Bradshaw YS, Safren SA, Beach MC, Lee Y, Rogers W, et al. Discussion of sexual risk behavior in HIV care is infrequent and appears ineffectual: a mixed methods study. AIDS Behav. 2011;15(4):812–22. doi:10.1007/s10461-010-9844-3.
Metsch LR, Pereyra M, del Rio C, Gardner L, Duffus WA, Dickinson G, et al. Delivery of HIV prevention counseling by physicians at HIV medical care settings in 4 US cities. Am J Public Health. 2004;94(7):1186–92.
Duffus WA, Barragan M, Metsch L, Krawczyk CS, Loughlin AM, Gardner LI, et al. Effect of physician specialty on counseling practices and medical referral patterns among physicians caring for disadvantaged human immunodeficiency virus-infected populations. Clin Infect Dis. 2003;36(12):1577–84. doi:10.1086/375070.
Centers for Disease Control aP. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States - 2014 Clinical Practice Guideline 2014. http://www.cdc.gov/hiv/pdf/PrEPguidelines2014.pdf. Accessed 23 June 2014.
Khawcharoenporn T, Kendrick S, Smith K. HIV risk perception and preexposure prophylaxis interest among a heterosexual population visiting a sexually transmitted infection clinic. AIDS Patient Care STDs. 2012;26(4):222–33. doi:10.1089/apc.2011.0202.
Whiteside YO, Harris T, Scanlon C, Clarkson S, Duffus W. Self-perceived risk of HIV infection and attitudes about preexposure prophylaxis among sexually transmitted disease clinic attendees in South Carolina. AIDS Patient Care STD. 2011;25(6):365–70. doi:10.1089/apc.2010.0224.
Pringle K, Merchant RC, Clark MA. Is self-perceived HIV risk congruent with reported HIV risk among traditionally lower HIV risk and prevalence adult emergency department patients? Implications for HIV testing. AIDS Patient Care STD. 2013;27(10):573–84. doi:10.1089/apc.2013.0013.
Klein H, Tilley DL. Perceptions of HIV risk among internet-using, HIV-negative barebacking men. Am J Men’s Health. 2012;6(4):280–93. doi:10.1177/1557988311434825.
Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009;24(1):119–27. doi:10.1093/her/cyn003.
Centers for Disease Control. A guide to taking a sexual history. http://www.cdc.gov/std/treatment/SexualHistory.pdf. Accessed 23 June 2014.
Lanier Y, Castellanos T, Barrow RY, Jordan WC, Caine V, Sutton MY. Brief sexual histories and routine HIV/STD testing by medical providers. AIDS Patient Care STDs. 2014;28(3):113–20. doi:10.1089/apc.2013.0328.
Jenness SM, Neaigus A, Murrill CS, Wendel T, Forgione L, Hagan H. Estimated HIV incidence among high-risk heterosexuals in New York City, 2007. J Acquir Immune Defic Syndr. 2011;56(2):193–7. doi:10.1097/QAI.0b013e318202a9c4.
LaLota M, Beck DW, Metsch LR, Brewer TH, Forrest DW, Cardenas GA, et al. HIV seropositivity and correlates of infection among heterosexually active adults in high-risk areas in South Florida. AIDS Behav. 2011;15(6):1259–63. doi:10.1007/s10461-010-9856-z.
Menza TW, Hughes JP, Celum CL, Golden MR. Prediction of HIV acquisition among men who have sex with men. Sex Transm Dis. 2009;36(9):547–55. doi:10.1097/OLQ.0b013e3181a9cc41.
Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Soc Sci Med. 1997;44(9):1303–12.
Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–21. doi:10.1007/s10461-014-0839-3.
Aitken C, Power R, Dwyer R. A very low response rate in an on-line survey of medical practitioners. Aust N Z J Public Health. 2008;32(3):288–9. doi:10.1111/j.1753-6405.2008.00232.x.
Grava-Gubins I, Scott S. Effects of various methodologic strategies: survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician. 2008;54(10):1424–30.
Acknowledgments
The work was supported by award EI11-SD-005 from CHRP; by the UCSD Center for AIDS Research – Bioinformatics and Information Technology Core; and by NIAID grants AI064086 (K24 to RH), AI27670 (UCSD ACTU) AI36214 (UCSD CFAR), K23 MH098795 (to DK) and 5T32AI007036. Dr. Blumenthal is supported by Grant T32 AI007036. Dr. Krakower is supported by Grant K23 MH098795. Dr. Haubrich is supported by award from CHRP and NIAID Grants K24 AI064086, ACTU AI27670 and CFAR AI36214.
Conflict of interest
There are no relevant conflict of interests.
Disclosure
Jill Blumenthal has no financial disclosures. Sonia Jain has no financial disclosures. Douglas Krakower reports research support from Gilead Sciences and Bristol Myers Squibb. Xiaoying Sun has no financial disclosures. Jason Young has no financial disclosures. Kenneth Mayer reports research support from Gilead Sciences and Alere. Richard Haubrich reports having received honoraria or consultant fees from Bristol Myers Squibb, Gilead Sciences, Janssen and Merck and research support (to UCSD) from Abbott, GlaxoSmithKline, Pfizer and Merck.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Blumenthal, J., Jain, S., Krakower, D. et al. Knowledge is Power! Increased Provider Knowledge Scores Regarding Pre-exposure Prophylaxis (PrEP) are Associated with Higher Rates of PrEP Prescription and Future Intent to Prescribe PrEP. AIDS Behav 19, 802–810 (2015). https://doi.org/10.1007/s10461-015-0996-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-0996-z