Abstract
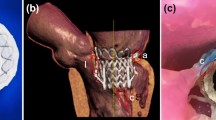
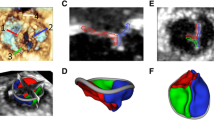
As catheter-based structural heart interventions become increasingly complex, the ability to effectively model patient-specific valve geometry as well as the potential interaction of an implanted device within that geometry will become increasingly important. Our aim with this investigation was to combine the technologies of high-spatial resolution cardiac imaging, image processing software, and fused multi-material 3D printing, to demonstrate that patient-specific models of the mitral valve apparatus could be created to facilitate functional evaluation of novel trans-catheter mitral valve repair strategies. Clinical 3D transesophageal echocardiography and computed tomography images were acquired for three patients being evaluated for a catheter-based mitral valve repair. Target anatomies were identified, segmented and reconstructed into 3D patient-specific digital models. For each patient, the mitral valve apparatus was digitally reconstructed from a single or fused imaging data set. Using multi-material 3D printing methods, patient-specific anatomic replicas of the mitral valve were created. 3D print materials were selected based on the mechanical testing of elastomeric TangoPlus materials (Stratasys, Eden Prairie, Minnesota, USA) and were compared to freshly harvested porcine leaflet tissue. The effective bending modulus of healthy porcine MV tissue was significantly less than the bending modulus of TangoPlus (p < 0.01). All TangoPlus varieties were less stiff than the maximum tensile elastic modulus of mitral valve tissue (3697.2 ± 385.8 kPa anterior leaflet; 2582.1 ± 374.2 kPa posterior leaflet) (p < 0.01). However, the slopes of the stress-strain toe regions of the mitral valve tissues (532.8 ± 281.9 kPa anterior leaflet; 389.0 ± 156.9 kPa posterior leaflet) were not different than those of the Shore 27, Shore 35, and Shore 27 with Shore 35 blend TangoPlus material (p > 0.95). We have demonstrated that patient-specific mitral valve models can be reconstructed from multi-modality imaging datasets and fabricated using the multi-material 3D printing technology and we provide two examples to show how catheter-based repair devices could be evaluated within specific patient 3D printed valve geometry. However, we recognize that the use of 3D printed models for the development of new therapies, or for specific procedural training has yet to be defined.








Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- DICOM:
-
Digital imaging and communication in medicine
- IPS:
-
Image processing software
- LA:
-
Left atrium
- LV:
-
Left ventricle
- MR:
-
Mitral regurgitation
- MV:
-
Mitral valve
- 3D TEE:
-
Three-dimensional transesophageal Echocardiography
- TMVR:
-
Trans-catheter mitral valve replacement
References
Durst, C. A., M. P. Cuchiara, E. G. Mansfield, J. L. West, and K. J. Grande-Allen. Flexural characterization of cell encapsulated PEGDA hydrogels with applications for tissue engineered heart valves. Acta Biomater. 7(6):2467–2476, 2011.
Farooqi, K. M., and P. P. Sengupta. Echocardiography and three-dimensional printing: sound ideas to touch a heart. J. Am. Soc. Echocardiogr. 28(4):398–403, 2015.
Goswami, R., C. Barker, N. Kleiman, M. Jackson, and S. H. Little. Transesophageal echocardiography-guided percutaneous intervention of a mitral valve leaflet perforation. JACC Cardiovasc. Interv. 8(5):754–755, 2015.
Kheradvar, A., E. M. Groves, G. A. Simmons, B. Griffith, S. H. Alavi, R. Tranquillo, L. P. Dasi, A. Falahatpisheh, K. J. Grande-Allen, C. J. Goergen, M. R. K. Mofrad, F. Baajijens, S. Canic, and S. H. Little. Emerging trends in heart valve engineering: part III. Novel technologies for mitral valve repair and replacement. Ann. Biomed. Eng. 43(4):858–870, 2015.
Little, S. H., M. Vukicevic, E. Avenatti, M. Ramchandani, and C. Barker. 3D Printed Modeling for Patient-specific mitral valve intervention: repair with a clip and a plug. JACC Cardiovasc. Interv. 9(9):973–975, 2016.
Mahmood, F., K. Owais, C. Taylor, M. Montealegre-Gallegos, W. Manning, R. Matyal, and K. R. Khabbaz. Three dimensional printing of mitral valve using echocardiographic data. JACC 8(2):226–231, 2015.
Maragiannis, D., M. S. Jackson, S. R. Igo, S. M. Chang, W. A. Zoghbi, and S. H. Little. Functional 3d printed patient-specific modeling of severe aortic stenosis. JACC 64(10):1066–1068, 2014.
Maragiannis, D., Jackson, MS, S. R. Igo, R. C. Schutt, P. Connell, J. Grande-Allen, et al. Replicating patient-specific severe aortic valve stenosis with functional 3D modeling. Circ. Cardiovasc. Imaging 8(10):e003626, 2015.
Merryman, W. D., H.-Y. S. Huang, F. J. Schoen, and M. S. Sacks. The effects of cellular contraction on aortic valve leaflet flexural stiffness. J. Biomech. 39(1):88–96, 2006.
Nkomo, V. T., J. M. Gardin, T. N. Skelton, J. S. Gottdiener, C. G. Scott, and M. Enriquez-Sarano. Burden of valvular heart diseases: a population-based study. Lancet 368:1005–1011, 2006.
Olivieri, L. J., A. Krieger, Y. H. Loke, D. S. Nath, P. C. Kim, and C. A. Sable. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Soc Echocardiogr. 28(4):392–397, 2015.
Richards, J. M., E. J. Farrar, B. G. Kornreich, N. S. Moıse, and J. T. Butcher. The mechanobiology of mitral valve function, degeneration, and repair. J. Vet. Cardiol. 14:47e58, 2012.
Witschey, W. R. T., A. M. Pouch, J. R. McGarvey, K. Ikeuchi, F. Contijoch, M. M. Levack, P. A. Yushkevich, C. M. Sehgal, B. M. Jackson, R. C. Gorman, and J. H. Gorman. Three-dimensional ultrasound-derived physical mitral valve modeling. Ann. Thorac. Surg. 98:691–694, 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Lakshmi Prasad Dasi oversaw the review of this article.
An erratum to this article is available at http://dx.doi.org/10.1007/s10439-016-1690-7.
Rights and permissions
About this article
Cite this article
Vukicevic, M., Puperi, D.S., Jane Grande-Allen, K. et al. 3D Printed Modeling of the Mitral Valve for Catheter-Based Structural Interventions. Ann Biomed Eng 45, 508–519 (2017). https://doi.org/10.1007/s10439-016-1676-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1676-5