Abstract
Purpose
To compare the corneal biomechanical properties of eyes that have undergone penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK), and Descemet stripping automated endothelial keratoplasty (DSAEK).
Methods
This case–control study comprised 20 post-PK eyes, 14 post-DALK eyes, 15 post-DSAEK eyes, and 50 normal control eyes. A dynamic Scheimpflug analyzer (the Corvis ST) was used to evaluate the corneal biomechanical properties including deformation amplitude (DA) and radius at the highest concavity (R hc).
Results
In post-PK eyes, the mean DA was 1.20 ± 0.13 mm, which was significantly higher than those of the control eyes (1.07 ± 0.09) and the post-DSAEK eyes (1.08 ± 0.12). The DA (1.18 ± 0.18) in the post-DALK eyes was significantly higher than in the control eyes. The R hc in the post-PK (6.34 ± 0.37 mm), -DALK (6.04 ± 1.22), and -DSAEK (6.44 ± 0.58) eyes was significantly smaller than in the control eyes (7.57 ± 0.78).
Conclusions
The dynamic Scheimpflug analyzer provides a method to obtain new biomechanical information on the cornea such as the DA and R hc, and these parameters differed among eyes that had undergone 3 different types of corneal surgery. Abnormalities in these parameters after the different corneal transplantation techniques may indicate larger deviations in the stress–strain reaction of the cornea and more uncertainty in the intraocular pressure measurements than in normal eyes.




Similar content being viewed by others
References
Archila EA. Deep lamellar keratoplasty dissection of host tissue with intrastromal air injection. Cornea. 1984–1985;3:217–8.
Sugita J, Kondo J. Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol. 1997;81:184–8.
Anwar M, Teichmann KD. Big-bubble technique to bare Descemetʼs membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28:398–403.
Melles GR, Eggink FA, Lander F, Pels E, Rietveld FJ, Beekhuis WH, et al. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998;17:618–26.
Terry MA, Ousley PJ. Replacing the endothelium without corneal surface incisions or sutures: the first United States clinical series using the deep lamellar endothelial keratoplasty procedure. Ophthalmology. 2003;110:755–64.
Price FW Jr, Price MO. Descemet’s stripping with endothelial keratoplasty in 200 eyes: early challenges and techniques to enhance donor adherence. J Cataract Refract Surg. 2006;32:411–8.
Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, Shtein RM. Descemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:1818–30.
Melles GR, Ong TS, Ververs B, van der Wees J. Descemet membrane endothelial keratoplasty (DMEK). Cornea. 2006;25:987–90.
Price MO, Giebel AW, Fairchild KM, Price FW Jr. Descemetʼs membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology. 2009;116:2361–8.
Koh S, Maeda N, Nakagawa T, Higashiura R, Saika M, Mihashi T, et al. Characteristic higher-order aberrations of the anterior and posterior corneal surfaces in 3 corneal transplantation techniques. Am J Ophthalmol. 2012;153:284–90.
Rudolph M, Laaser K, Bachmann BO, Cursiefen C, Epstein D, Kruse FE. Corneal higher-order aberrations after Descemetʼs membrane endothelial keratoplasty. Ophthalmology. 2012;119:528–35.
Kawashima M, Kawakita T, Shimmura S, Tsubota K, Shimazaki J. Characteristics of traumatic globe rupture after keratoplasty. Ophthalmology. 2009;116:2072–6.
Sari ES, Koytak A, Kubaloglu A, Culfa S, Erol MK, Ermis SS, et al. Traumatic wound dehiscence after deep anterior lamellar keratoplasty. Am J Ophthalmol. 2013;156:767–72.
Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31:156–62.
Feigenbaum SK, Qazi MA, Sanderson JP, Roberts CJ, Pepose JS. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic, and noncontact tonometry. Am J Ophthalmol. 2007;143:39–47.
Fontes BM, Ambrósio R Jr, Jardim D, Velarde GC, Nosé W. Corneal biomechanical metrics and anterior segment parameters in mild keratoconus. Ophthalmology. 2010;117:673–9.
Vinciguerra P, Albè E, Mahmoud AM, Trazza S, Hafezi F, Roberts CJ. Intra- and postoperative variation in ocular response analyzer parameters in keratoconic eyes after corneal cross-linking. J Refract Surg. 2010;26:669–76.
Yenerel NM, Kucumen RB, Gorgun E. Changes in corneal biomechanics in patients with keratoconus after penetrating keratoplasty. Cornea. 2010;29:1247–51.
Jafarinasab MR, Feizi S, Javadi MA, Hashemloo A. Graft biomechanical properties after penetrating keratoplasty versus deep anterior lamellar keratoplasty. Curr Eye Res. 2011;36:417–21.
Hosny M, Hassaballa MA, Shalaby A. Changes in corneal biomechanics following different keratoplasty techniques. Clin Ophthalmol. 2011;5:767–70.
Acar BT, Akdemir MO, Acar S. Corneal biomechanical properties in eyes with no previous surgery, with previous penetrating keratoplasty and with deep anterior lamellar keratoplasty. Jpn J Ophthalmol. 2013;57:85–9.
Hon Y, Lam AK. Corneal deformation measurement using Scheimpflug noncontact tonometry. Optom Vis Sci. 2013;90:e1–8.
Hong J, Xu J, Wei A, Deng SX, Cui X, Yu X, et al. A new tonometer—the Corvis ST tonometer: clinical comparison with noncontact and Goldmann applanation tonometers. Invest Ophthalmol Vis Sci. 2013;54:659–65.
Faria-Correia F, Ramos I, Valbon B, Luz A, Roberts CJ, Ambrósio R Jr. Scheimpflug-based tomography and biomechanical assessment in pressure-induced stromal keratopathy. J Refract Surg. 2013;29:356–8.
Nemeth G, Hassan Z, Csutak A, Szalai E, Berta A, Modis L Jr. Repeatability of ocular biomechanical data measurements with a Scheimpflug-based noncontact device on normal corneas. J Refract Surg. 2013;29:558–63.
Reznicek L, Muth D, Kampik A, Neubauer AS, Hirneiss C. Evaluation of a novel Scheimpflug-based non-contact tonometer in healthy subjects and patients with ocular hypertension and glaucoma. Br J Ophthalmol. 2013;97:1410–4.
Acknowledgments
Publication of this article was supported in part by a Grant-in-Aid for Scientific Research (no. 24592669; to Naoyuki Maeda) from the Japanese Ministry of Education, Culture, Sports, Science and Technology. The authors would like to thank Duco Hamasaki, PhD, for the English language review.
Conflicts of interest
N. Maeda, Research Grant (Topcon), Instrument (Corvis® ST: Oculus); R. Ueki, None; M. Fuchihata, None; H. Fujimoto, None; S. Koh, None; K. Nishida, None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10384_2014_344_MOESM2_ESM.mpg
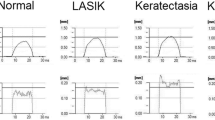
Supplementary material 2: Video 1. This video indicates the difference in dynamic air pulse-induced changes in corneal shape between the normal eye (left) and the eye following penetrating keratoplasty (right) shown in Figure 1 (MPG 1,912 kb)
About this article
Cite this article
Maeda, N., Ueki, R., Fuchihata, M. et al. Corneal biomechanical properties in 3 corneal transplantation techniques with a dynamic Scheimpflug analyzer. Jpn J Ophthalmol 58, 483–489 (2014). https://doi.org/10.1007/s10384-014-0344-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-014-0344-2