Summary
Introduction
The human immunodeficiency virus (HIV) is still a remarkable challenge throughout the world, especially in developing countries. Despite the fact that HIV in children is becoming one of the most challenging diseases, it seems that pediatric AIDS in Iran is an unknown disease and there is a lack of studies about it. The aim of this study was to describe the characteristics of HIV-positive children who referred to the hospitals of Tehran, Kermanshah, Kurdistan, and Qom provinces of Iran.
Materials and methods
This study was a retrospective investigation of medical records among 61 children with a diagnosis of HIV who were admitted to the children’s hospitals in the four provinces of Iran during a 3-year period (2013–2016).
Results
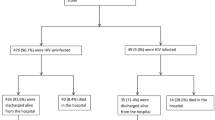
The frequency of HIV in the center of Iran (Tehran and Qom provinces) was higher (N = 37, 61%). Most of the infected patients were between 5 and 15 years old, 52% were male, and 93% had a history of HIV in their family. Median age at diagnosis of HIV was 2 years. Most of the hospitalized patients were discharged and only two patients (3%) died due to HIV infection. The vast majority of patients (93%) were infected through maternal transmission and a low percentage (29%) were diagnosed before 1 year of age. All of them were in the third stage of the disease. All patients had a positive HIV PCR test. HIV EIA was positive in the majority of cases (98%). A history of addiction in the family was demonstrated in 22 cases (36%). Weight loss (N = 51, 84%), prolonged fever (N = 50, 81%), and respiratory infection (N = 26, 47%) were the most common symptoms.
Conclusion
This study demonstrated a high frequency of pediatric HIV among children aged 5–15 years in four provinces of Iran. Novel strategies to prevent and eliminate mother-to-child transmission of HIV, diagnostic facilities, and treatment of infected mothers during pregnancy in our country are highly recommended.
Similar content being viewed by others
References
Bryant M, Beard J. Orphans and vulnerable children affected by human immunodeficiency virus in sub-Saharan Africa. Pediatr Clin North Am. 2016;63(1):131–47.
World Health Organization, TMB Initiative. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants: Guidelines on care, treatment and support for women living with HI. 2015.
World Health Organization. HIV diagnosis and ARV use in HIV-exposed infants: A programmatic update. 2018.
Brown LK, Lourie KJ. Children and adolescents living with HIV and AIDS: A review. J Child Psychol Psychiatry. 2000;41(1):81–96.
Joint United Nations Programme on HIV/AIDS. Global AIDS update 2016. Geneva: UNAIDS; 2016.
Powis KM, Slogrove AL, Mofenson L. Protecting the health of our AIDS-free generation: Beyond prevention of mother-to-child HIV transmission. AIDS. 2017;31(2):315–6.
Weiler G. Global update on HIV treatment 2013: Results, impact and opportunities. 2013.
Zamani S, et al. High prevalence of HIV infection associated with incarceration among community-based injecting drug users in Tehran, Iran. J Acquir Immune Defic Syndr. 2006;42(3):342–6.
Merchant RH, Lala MM. Common clinical problems in children living with HIV/AIDS: Systemic approach. Indian J Pediatr. 2012;79(11):1506–13.
Read JS. Diagnosis of HIV-1 infection in children younger than 18 months in the United States. Pediatrics. 2007;120(6):e1547–e62.
Joint United Nations Programme on HIV/AIDS, UNICEF. Children and AIDS: Fifth Stocktaking Report, 2010. 2010.
Parinitha S, Kulkarni M. Haematological changes in HIV infection with correlation to CD4 cell count. Australas Med J. 2012;5(3):157–62.
World Health Organization. WHO child growth standards: Length/height for age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age, methods and development. 2006.
Ferrand RA, et al. HIV infection presenting in older children and adolescents: A case series from Harare, Zimbabwe. Clin Infect Dis. 2007;44(6):874–8.
Shahrin L, et al. Clinical profile of hospitalized HIV-infected children in Bangladesh, a low-HIV-prevalence country. Paediatr Int Child Health. 2014;34(2):133–7.
Poudel P, et al. Profile of HIV infected children: A hospital based study at Eastern Nepal. Asian Pac J Trop Dis. 2014;4(3):169–75.
Lodha R, et al. Clinical profile and natural history of children with HIV infection. Indian J Pediatr. 2006;73(3):201–4.
Heidary M, Nasiri MJ. Why has HIV/AIDS prevalence increased in Iran? Clin Infect Dis. 2016;63(6):846.
Movahedi Z, et al. Epidemiology of children with acquired immune deficiency syndrome (stage 3): A referral hospital-based study in Iran. J Med Virol. 2016;88(1):64–8.
Shokoohi M, et al. HIV knowledge, attitudes, and practices of young people in Iran: Findings of a National Population-Based Survey in 2013. PLoS ONE. 2016;11(9):e161849.
Brown BJ, et al. Clinical and immunological profile of pediatric HIV infection in Ibadan, Nigeria. J Int Assoc Physicians AIDS Care. 2011;10(1):49–53.
Shah SR, Tullu MS, Kamat JR. Clinical profile of pediatric HIV infection from India. Arch Med Res. 2005;36(1):24–31.
Baghaei P, et al. HIV and tuberculosis trends and survival of coinfection in a referral center in Tehran: A 12-year study. Int J Mycobacteriol. 2016;5:S16–S7.
Reust CE. Evaluation of primary immunodeficiency disease in children. Am Fam Physician. 2013;87(11):773–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Mahmoudi, B. Pourakbari, M. Moradzadeh, Z. Movahedi, K. Ghadiri, M. Abedini, A. Aziz-Ahari, A. Ramezani, and S. Mamishi declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Pasteur Institute of Iran ethics committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahmoudi, S., Pourakbari, B., Moradzadeh, M. et al. Epidemiologic and clinical findings of children with acquired immunodeficiency syndrome in four provinces of Iran. Wien Med Wochenschr 170, 212–217 (2020). https://doi.org/10.1007/s10354-019-0703-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-019-0703-1