Abstract
Background
Parkinson disease with orthostatic hypotension (PD + OH) and the parkinsonian form of multiple system atrophy (MSA-P) can be difficult to distinguish clinically. Recent studies indicate that PD entails a vesicular storage defect in catecholaminergic neurons. Although cardiac sympathetic neuroimaging by 18F-dopamine positron emission tomography can identify decreased vesicular storage, this testing is not generally available. We assessed whether plasma biomarkers of a vesicular storage defect can separate PD + OH from MSA-P.
Methods
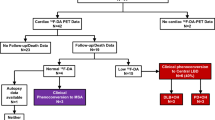
We conceptualized that after F-dopamine injection, augmented production of F-dihydroxyphenylacetic acid (F-DOPAC) indicates decreased vesicular storage, and we therefore predicted that arterial plasma F-DOPAC would be elevated in PD + OH but not in MSA-P. We measured arterial plasma F-DOPAC after 18F-dopamine administration (infused i.v. over 3 min) in patients with PD + OH (N = 12) or MSA-P (N = 21) and in healthy control subjects (N = 26). Peak F-DOPAC:dihydroxyphenylglycol (DHPG) was also calculated to adjust for effects of denervation on F-DOPAC production.
Results
Plasma F-DOPAC accumulated rapidly after initiation of 18F-dopamine infusion. Peak F-DOPAC (5–10 min) in PD + OH averaged three times that in MSA-P (P < 0.0001). Among MSA-P patients, none had peak F-DOPAC > 300 nCi-kg/cc-mCi, in contrast with 7 of 12 PD + OH patients (χ 2 = 16.6, P < 0.0001). DHPG was lower in PD + OH (3.83 ± 0.36 nmol/L) than in MSA-P (5.20 ± 0.29 nmol/L, P = 0.007). All MSA-P patients had peak F-DOPAC:DHPG < 60, in contrast with 9 of 12 PD + OH patients (χ 2 = 17.5, P < 0.0001). Adjustment of peak F-DOPAC for DHPG increased test sensitivity from 58 to 81 % at similar high specificity.
Interpretation
After F-dopamine injection, plasma F-DOPAC and F-DOPAC:DHPG distinguish PD + OH from MSA-P.





Similar content being viewed by others
Abbreviations
- 6F-DOPAC:
-
6-Fluorodihydroxyphenylacetic acid
- DHPG:
-
3,4-Dihydroxyphenylglycol
- MAO:
-
Monoamine oxidase
- OH:
-
Orthostatic hypotension
- MSA:
-
Multiple system atrophy
- PAF:
-
Pure autonomic failure
- PD:
-
Parkinson disease
- ROC:
-
Receiver operating characteristic
- VMAT2:
-
Type 2 vesicular monoamine transporter
References
Goldstein DS, Eisenhofer G, Dunn BB, Armando I, Lenders J, Grossman E, Holmes C, Kirk KL, Bacharach S, Adams R et al (1993) Positron emission tomographic imaging of cardiac sympathetic innervation using 6-[18F]fluorodopamine: initial findings in humans. J Am Coll Cardiol 22:1961–1971
Goldstein DS, Eisenhofer G, Kopin IJ (2003) Sources and significance of plasma levels of catechols and their metabolites in humans. J Pharmacol Exp Ther 305:800–811
Goldstein DS, Grossman E, Tamrat M, Chang PC, Eisenhofer G, Bacher J, Kirk KL, Bacharach S, Kopin IJ (1991) Positron emission imaging of cardiac sympathetic innervation and function using 18F-6-fluorodopamine: effects of chemical sympathectomy by 6-hydroxydopamine. J Hypertens 9:417–423
Goldstein DS, Holmes C (1997) Metabolic fate of the sympathoneural imaging agent 6-[18F]fluorodopamine in humans. Clin Exp Hypertens 19:155–161
Goldstein DS, Holmes C, Bentho O, Sato T, Moak J, Sharabi Y, Imrich R, Conant S, Eldadah BA (2008) Biomarkers to detect central dopamine deficiency and distinguish Parkinson disease from multiple system atrophy. Parkinsonism Relat Disord 14:600–607
Goldstein DS, Holmes C, Kopin IJ, Sharabi Y (2011) Intra-neuronal vesicular uptake of catecholamines is decreased in patients with Lewy body diseases. J Clin Investig 121:3320–3330
Goldstein DS, Holmes C, Li ST, Bruce S, Metman LV, Cannon RO 3rd (2000) Cardiac sympathetic denervation in Parkinson disease. Ann Intern Med 133:338–347
Goldstein DS, Holmes C, Sharabi Y, Brentzel S, Eisenhofer G (2003) Plasma levels of catechols and metanephrines in neurogenic orthostatic hypotension. Neurology 60:1327–1332
Goldstein DS, Sullivan P, Holmes C, Miller GW, Alter S, Strong R, Mash DC, Kopin IJ, Sharabi Y (2013) Determinants of buildup of the toxic dopamine metabolite DOPAL in Parkinson’s disease. J Neurochem 126:591–603
Goldstein DS, Tack C (2000) Non-invasive detection of sympathetic neurocirculatory failure. Clin Auton Res 10:285–291
Holmes C, Eisenhofer G, Goldstein DS (1994) Improved assay for plasma dihydroxyphenylacetic acid and other catechols using high-performance liquid chromatography with electrochemical detection. J Chromatogr B Biomed Appl 653:131–138
Kaufmann H (1996) Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin Auton Res 6:125–126
Orimo S, Suzuki M, Inaba A, Mizusawa H (2012) 123I-MIBG myocardial scintigraphy for differentiating Parkinson’s disease from other neurodegenerative parkinsonism: a systematic review and meta-analysis. Parkinsonism Relat Disord 18:494–500
Ziegler MG, Lake CR, Kopin IJ (1977) The sympathetic-nervous-system defect in primary orthostatic hypotension. N Engl J Med 296:293–297
Acknowledgments
Authors acknowledge the support of the intramural Research Program of the NIH, National Institute of Neurological Disorders and Stroke.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldstein, D.S., Kopin, I.J., Sharabi, Y. et al. Plasma biomarkers of decreased vesicular storage distinguish Parkinson disease with orthostatic hypotension from the parkinsonian form of multiple system atrophy. Clin Auton Res 25, 61–67 (2015). https://doi.org/10.1007/s10286-015-0268-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0268-z