Abstract
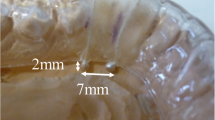
Oral appliance (OA) can effectively treat obstructive sleep apnea; however, numerous types of oral appliances and designs are variable and the precise mechanisms behind differences in treatment outcomes are uncertain. The objective of this study was to evaluate the effects of different degrees of mandibular position [4° of bite openings (BO): 2, 4, 8 and 12 mm; and protrusion (P): 0, 50%, MAX], for both the upright and supine positions: BO2 mm_P0%, BO4 mm_P0%, BO4 mm_P50%, BO4 mm_PMAX, BO8 mm_P0%, BO12 mm_P0%; with an OA on the: (1) activity of the genioglossus (GG) muscle by electromyogram, (2) inspiration by airflow sensor, and (3) recording mandibular movements (incisor and mandibular condyle point) in each position. Nine healthy male adults (age 27.5 ± 1.30 years) were recruited. The results show that GG muscle activity increased significantly from BO 4 mm_P0% to BO12 mm_P0% during the supine position, and the strongest signal was found in BO4 mm_PMAX, compared to all of the other positions, and GG muscle activity in BO4 mm_P0% tended to be lower. From supine to upright position the inspiration increased significantly but GG muscle activity did not. These results might be a stimulus to augment a compensatory mechanism of GG muscle induced by OA, however, mainly in protrusion position. The increase of BO (2–12 mm) and even maximum protrusion might not negatively affect the temporomandibular joint.




Similar content being viewed by others
References
George PT. Selecting sleep-disordered-breathing appliances. Biomechanical considerations. J Am Dent Assoc. 2001;132:339–47.
Otsuka R, Ono T, Honda E, Sasaki T, Kuroda T. Effect of titrated mandibular advancement and jaw opening on the upper airway in nonapneic men: a magnetic resonance imaging and cephalometric study. Am J Orthod Dentofac Orthop. 2004;125:191–9.
Tsuiki S, Ono T, Kuroda T. Mandibular advancement modulates respiratory-related genioglossus electromyographic activity. Sleep Breath. 2000;4:53–7.
Ogawa T, Long J, Sutherland K, Chan AS, Sasaki K, Cistulli PA. Effect of mandibular advancement splint treatment on tongue shape in obstructive sleep apnea. Sleep Breath. 2015;19:857–63.
Rose E, Staats R, Virchow C, Jonas IE. A comparative study of two mandibular advancement appliances for the treatment of obstructive sleep apnoea. Eur J Orthod. 2002;24:191–8.
Vroegop AV, Vanderveken OM, Van de Heyning PH, Braem MJ. Effects of vertical opening on pharyngeal dimensions in patients with obstructive sleep apnoea. Sleep Med. 2012;13:314–6.
Nikolopoulou M, Naeije M, Aarab G, Hamburger HL, Visscher CM, Lobbezoo F. The effect of raising the bite without mandibular protrusion on obstructive sleep apnoea. J Oral Rehabil. 2011;38:643–7.
Pitsis AJ, Darendeliler MA, Gotsopoulos H, Petocz P, Cistulli PA. Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166:860–4.
Alonso JF, Mañanas MA, Rojas M, Bruce EN. Coordination of respiratory muscles assessed by means of nonlinear forecasting of demodulated myographic signals. J Electromyogr Kinesiol. 2011;21:1064–73.
Okawara Y, Tsuiki S, Hiyama S, Hashimoto K, Ono T, Ohyama K. Oral appliance titration and nasal resistance in nonapneic subjects. Am J Orthod Dentofac Orthop. 2004;126:620–2.
Doble EA, Leiter JC, Knuth SL, Daubenspeck JA, Bartlett D Jr. A noninvasive intraoral electromyographic electrode for genioglossus muscle. J Appl Physiol. 1985;58:1378–82.
Mezzanotte WS, Tangel DJ, White DP. Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism). J Clin Invest. 1992;89:1571–9.
Meurice JC, Marc I, Carrier G, Sériès F. Effects of mouth opening on upper airway collapsibility in normal sleeping subjects. Am J Respir Crit Care Med. 1996;153:255–9.
Lee CH, Kim DK, Kim SY, Rhee CS, Won TB. Changes in site of obstruction in obstructive sleep apnea patients according to sleep position: a DISE study. Laryngoscope. 2015;125:248–54.
Acknowledgements
The authors are grateful to Professor Peter A. Cistulli and Dr. Kate Sutherland from Centre for Sleep Health and Research, Department of Respiratory Medicine, Royal North Shore Hospital, St Leonards, NSW, Australia, and Woolcock Institute of Medical Research and Sydney Medical School, University of Sydney, for important scientific advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
J. Long and T. Ogawa contributed equally to this work.
Rights and permissions
About this article
Cite this article
Long, J., Ogawa, T., Ito, T. et al. Effect of bite openings and mandibular protrusion on genioglossus muscle activity in healthy adults with oral appliance. Odontology 106, 90–95 (2018). https://doi.org/10.1007/s10266-017-0299-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-017-0299-0