Abstract
Background
Femoral fracture in adolescents is a significant injury. It is generally agreed that operative fixation is the treatment of choice, and rigid intramedullary nail fixation is a treatment option. However, numerous types of rigid nails to fix adolescent femoral fractures have been described. Hence, the aim of this paper was to collate and evaluate the available evidence for managing diaphyseal femoral fractures in adolescents using rigid intramedullary nails.
Materials and methods
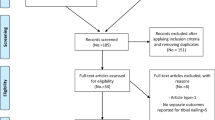
A literature search was undertaken using the healthcare database website (http://www.library.nhs.uk/hdas). Medline, CINAHL, Embase, and the Cochrane Library databases were searched to identify prospective and retrospective studies of rigid intramedullary nail fixation in the adolescent population.
Results
The literature search returned 1,849 articles, among which 51 relevant articles were identified. Of these 51 articles, 23 duplicates were excluded, so a total of 28 articles were reviewed. First-generation nails had a high incidence of limb length discrepancy (Küntscher 5.8 %, Grosse–Kempf 9 %), whilst second-generation nails had a lower incidence (Russell–Taylor 1.7 %, AO 2.6 %). Avascular necrosis was noted with solid Ti nails (2.6 %), AO femoral nails (1.3 %) and Russell–Taylor nails (0.85 %). These complications have not been reported with the current generation of nails.
Conclusions
Rigid intramedullary nail fixation of femoral fractures in adolescents is a useful procedure with good clinical results. A multiplanar design and lateral trochanteric entry are key to a successful outcome of titanium alloy nail fixation.
Similar content being viewed by others
Introduction
Femoral fractures account for 1.4 % [1] to 1.7 % [2] of all fractures in children. The incidence of femoral fractures in children has been reported as 20–33 per 100,000 per year [1, 3–5]. The common modes of injury resulting in femoral fractures in adolescents include road traffic collisions, sports injuries and falls from height [3, 6, 7]. The risk of sustaining a femoral fracture is higher in boys than in girls [3, 5, 6, 8]. Management of femoral fractures in the adolescent population poses unique challenges due to the relative sizes of the femur and the open physes [7, 9]. Treatment options of these complex injuries have evolved over the last few decades [7, 10, 11]. Operative fixation techniques described in the current literature include external fixation, open reduction and internal fixation with plate, minimally invasive plate osteosynthesis (MIPO), and flexible and rigid intramedullary nails [7, 11–13].
Rigid intramedullary nailing has been suggested as a treatment option in these patients due to the perceived advantages of stable fixation with higher union and low complication rates [9, 14]. However, several studies have questioned this approach given the risks of avascular necrosis [15–18] and proximal femoral valgus deformity [19, 20]. Some authors have explored the lateral aspect of the greater trochanter to minimise these serious complications and obtain a good outcome [21, 22]. Hence, the aim of this paper was to collate and evaluate the available evidence for managing diaphyseal femoral fractures in adolescents using rigid intramedullary nails.
Numerous types of rigid nails have been described to treat adolescent femoral fractures. Due to the lack of consistency in reported outcomes, a comparison of various rigid nails is difficult and subject to observer variability. Based on their initial experience, Flynn and colleagues proposed criteria to grade the clinical outcome following fixation of femoral fractures [23]. They classified a major complication and/or lasting morbidity, a limb length discrepancy of >2.0 cm and malunion of >10° as a poor result. However, there is no agreement in the literature regarding similar outcome criteria for rigid intramedullary nail fixation [7, 9, 11]. Initial papers [14, 24, 25] on this topic reported on the radiographic parameters described by Edgren [26]. On the other hand, some studies have not reported on the radiological outcomes [16, 27, 28]. Therefore, to ensure that we performed an objective comparison of different nails, we analysed the reported clinical outcomes from the various studies with respect to major complications (avascular necrosis, limb length discrepancy >2.0 cm, malunion >10°).
Materials and methods
Study identification
A current literature search of all available evidence was undertaken using the healthcare database website (http://www.library.nhs.uk/hdas). The databases searched were Medline, CINAHL, Embase, and the Cochrane Library.
A Medline search was performed using boolean statements and the wildcard symbol (*) with the following search criteria: “(femur* OR femoral*) AND (shaft* OR diaph*) AND fracture* AND (child* OR pediat* OR paediat* OR adolescent*) AND (intramedullary* OR rod* OR nail*)”. An Embase search was performed using boolean statements and the wildcard symbol ($) with the following search criteria: “(femur$ OR femoral$) AND (shaft$ OR diaph$) AND fracture$ AND (child$ OR pediat$ OR paediat$ OR adolescent$) AND (intramedullary$ OR rod$ OR nail$)”. The CINAHL database was searched using the following criteria: “(femur* OR femoral*) AND (shaft* OR diaph*) AND fracture* AND (child* OR pediat* OR paediat* OR adolescent*) AND (intramedullary* OR rod* OR nail*)”. A review of the Cochrane database for relevant articles was performed using the search criteria ‘adolescent’ AND ‘femur’ AND ‘intramedullary nail’ OR ‘intramedullary rod’.
Eligibility criteria for the studies
Prospective and retrospective studies from the international literature describing rigid intramedullary nail fixation in the adolescent population were identified. Articles that reported on the description of the nail and/or design, clinical results and complications (specifically: avascular necrosis, limb length discrepancy and malunion) were included. Additionally, the bibliographies of all selected articles were scrutinised for relevant articles. Isolated case reports of complications following rigid nail fixation were excluded. Articles that only examined the flexible nail technique and results of its use, based on their title and abstract, were also excluded.
Classification of rigid intramedullary nails
In this review, we adopted the classification of rigid intramedullary nails based on the generation of the design and material technology [29]:
-
First generation: intramedullary nail with a cloverleaf design that resulted from pioneering work by Gerhard Küntscher [30], and was manufactured from stainless steel.
-
Second generation: the length and rotation of the intramedullary nail could be controlled through the use of a bicortical screw, which led to an expansion in the indications for this technique; examples include Küntscher interlocking, Grosse–Kempf, and Russell–Taylor nails.
-
Third generation: research into nail failures led to an improved design with interlocking screws manufactured from fatigue-resistant titanium alloys that were placed in a multiaxial direction.
-
Current generation: multiplanar nails incorporating improvements in design and material technology from the previous three generations.
Results
The literature search returned 1,849 articles, among which 51 relevant articles were identified. Of these 51 articles, 23 were duplicates, so 28 articles were reviewed (Table 1). A search through the bibliographies of the above articles identified a further 3 relevant articles which were also included in the analysis [27, 31–33]. A summary of the various studies on rigid nails identified from the literature search is presented in Table 2. We identified 2 papers from Ramseier [34, 35] and 1 paper from Stans [36] which discussed the results of rigid nail fixation, but these papers lacked descriptive detail regarding the type of rigid nail used. Hence, we included only the larger of the two studies from Ramseier [34] for analysis.
The Küntscher nail has been used for the fixation of femoral fractures in children [19, 24, 25, 37], but resulted in growth disturbance [19, 24]. This prompted some authors to question the use of the Küntscher nail in children [19]. There are numerous biomechanical studies [38–40] of this implant in the literature, but none of them focus on femoral fractures in children. Furthermore, biomechanical testing indicated that the Küntscher nail did not provide adequate stability for comminuted fractures in torsion and compression [39]. Hence, the use of Küntscher nails was largely abandoned in favour of new nail designs.
With the introduction of interlocking, second-generation nails such as the Grosse–Kempf nail [14, 32, 41], the Russell–Taylor nail, and its delta version (with a triangular section, a thicker wall and a thinner diameter) were used in adolescents [28, 42, 43]. However, the indication for their use in adolescents was simply an extension of the indication for their use in adults, even though there was only a limited understanding of the intricate vascularity of proximal femoral epiphysis in adolescents. This resulted in the growth disturbances noted in patients in these series [42, 43]. The current literature has descriptions of different rigid intramedullary nails, such as the Street–Hansen nail [44], tibial nail [45, 46], and flexible interlocking intramedullary nail (FIIN) [47]. However, these represent a limited series, as the use of such devices at other centres has not been reported.
Avascular necrosis of the femoral head, limb length discrepancy (>2 cm), and malunion >10° are significant complications that have been associated with intramedullary nail fixation of adolescent femoral fractures [9, 11, 15, 17, 19]. In order to analyse the heterogeneous data in the current literature, we collated the reported complications for the different intramedullary nails (Table 3). The early-generation nails (Küntscher/Grosse–Kempf) were noted to have high rates of limb length discrepancy (5–9 %). It is interesting that AVN was not reported in the earlier series [24, 37, 48]. However, this may be due to a combination of a limited understanding of this condition and a lack of widespread availability of investigative tools such as magnetic resonance imaging (MRI) at the time. The reporting of subclinical AVN in the later series [16, 42] using MRI is indicative of this development. Results obtained with Russell–Taylor nails show good improvement, with a lower incidence of limb length discrepancy (2.8 %). It has been reported that, by and large, multiplanar nails are not associated with such complications. Two studies [34, 36] have reported on AVN and limb length discrepancy, but a lack of detail regarding the type or design of the nail used limits their interpretation.
Discussion
The recent consensus on the age limit for rigid intramedullary fixation is ≥11 years [9, 11], although some authors advocate their use in children ≥9 years [49]. This is largely due to the increased complication rate reported following the use of flexible nails in this subset of patients [50]. Adolescents ≥49 kg have poor outcomes following other modalities of treatment for femoral fractures [11, 51], so these heavier adolescents are better managed with a rigid, locked intramedullary nail [9, 49, 52]. Excessive weight has also been shown to be an independent predictor of increased postoperative complications [51].
Attempts have been made to modify existing adult interlocking nails to overcome the limitations of the initial rigid uniplanar nail design [53]. Multiplanar nails, unlike uniplanar nails, allow a greater degree of freedom in choosing the entry point for nail insertion [21, 22, 52]. Earlier studies with piriformis entry had patients with complications such as avascular necrosis [16], coxa valga, and growth arrest of the greater trochanter [19]. Subsequent studies of nail designs with a lateral entry point report no such complication [21, 52]. Hence, the entry point of the intramedullary nail has been a subject of much debate due to the potential impact on the vascularity of the femoral head [9] and malalignment or iatrogenic fractures [54]. The entry point is largely dictated by the type/design of the nail [53]. Recent nails [21, 22, 27] have a multiplanar/helical design to avoid the piriformis entry point, which has been shown in a recent systematic review to be associated with a higher rate of avascular necrosis [55]. Specific paediatric nails are a welcome development and are suggested by some authors to be safe in skeletally immature patients younger than 12 years [56]. However, it should be noted that the results from this study were preliminary.
The design of these devices has evolved from the initial Küntscher nail to the current multiplanar rigid nails which allow introduction through a lateral entry portal. The majority of the improvements in this area have resulted from a better understanding of the femoral anatomy, in terms of both bony architecture [57, 58] and the vascularity of the physes [59]. Implant material and metallurgy is another interesting aspect of research aimed at developing devices that are fatigue resistant and possess superior biomechanical properties [60]. Multiplanar or helical design intramedullary nails are examples of this new development [22, 27, 61]. However, biomechanical studies and (more crucially) long-term clinical results of using such nails are lacking in the current literature [11].
The salient points from the current literature review point to the optimal features of an ideal rigid intramedullary nail for use in an adolescent and the subsequent management of such patients in order to achieve a good outcome. These are summarised below:
-
In terms of the design, multiplanar nail curvature is desirable in order to get a close match to the femoral anatomy, along with well-designed locking screws/bolts [22, 27, 46].
-
The optimal material is a titanium-based alloy with fatigue-resistant properties [27, 46].
-
The entry point should be the lateral aspect of the trochanter to minimise iatrogenic damage to the femoral head vasculature and avascular necrosis [55].
-
Postoperative review should pay careful attention to the recognition of major complications such as avascular necrosis to prevent morbidity [11]. When there is a diagnostic dilemma in cases with subtle and subclinical findings, MRI can be a useful investigative tool to facilitate a diagnosis [16, 42].
-
The duration of follow-up should be sufficient to identify asymptomatic cases [16, 41]. There is a lack of consensus regarding the maximum length of time [11], but a minimum duration of 24 months is useful for identifying cases of late AVN [16, 36, 41, 62].
-
Implant-related problems can be multifactorial. In cases with mechanical failure or iatrogenic complications secondary to the nail, nail removal and appropriate remedial procedures should be performed [9, 16, 63]. Adequate callus formation and disappearance of the fracture lines in the radiographs are simple yet useful indicators of sufficient bone healing to allow implant removal [64]. Implant removal following adequate fracture healing has also been suggested, as it is helpful to restore the normal bone mineral density in adolescents [65]. Early removal of the implant should be avoided.
In conclusion, rigid intramedullary nail fixation of femoral fractures in adolescents is a useful procedure with good clinical results. Standardisation of terminology and outcome parameters for intramedullary nail fixation in adolescents is required. Further evidence in terms of long-term clinical data and biomechanical studies is needed to be able to improve on the design of intramedullary nails in current use.
Appropriate patient selection, meticulous surgical technique, and nails that are purpose-built to avoid iatrogenic damage to the physes are key to achieving a good long-term clinical outcome.
References
Sahlin Y (1990) Occurrence of fractures in a defined population: a 1-year study. Injury 21(3):158–160
McCartney D, Hinton A, Heinrich SD (1994) Operative stabilization of pediatric femur fractures. Orthop Clin North Am 25(4):635–650
Hinton RY et al (1999) Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am 81(4):500–509
Nafei A et al (1992) Femoral shaft fractures in children: an epidemiological study in a Danish urban population, 1977–86. J Pediatr Orthop 12(4):499–502
Rewers A et al (2005) Childhood femur fractures, associated injuries, and sociodemographic risk factors: a population-based study. Pediatrics 115(5):e543–e552
Bridgman S, Wilson R (2004) Epidemiology of femoral fractures in children in the West Midlands region of England 1991 to 2001. J Bone Joint Surg Br 86(8):1152–1157
Hunter JB (2005) Femoral shaft fractures in children. Injury 36(Suppl 1):A86–A93
Hedlund R, Lindgren U (1986) The incidence of femoral shaft fractures in children and adolescents. J Pediatr Orthop 6(1):47–50
Hosalkar HS et al (2011) Intramedullary nailing of pediatric femoral shaft fracture. J Am Acad Orthop Surg 19(8):472–481
Dameron TB Jr, Thompson HA (1959) Femoral-shaft fractures in children. Treatment by closed reduction and double spica cast immobilization. J Bone Joint Surg Am 41-A:1201–1212
Kocher MS et al (2010) American Academy of Orthopaedic Surgeons clinical practice guideline on treatment of pediatric diaphyseal femur fracture. J Bone Joint Surg Am 92(8):1790–1792
Poolman RW, Kocher MS, Bhandari M (2006) Pediatric femoral fractures: a systematic review of 2422 cases. J Orthop Trauma 20(9):648–654
Heinrich SD et al (1992) Stabilization of pediatric diaphyseal femur fractures with flexible intramedullary nails (a technique paper). J Orthop Trauma 6(4):452–459
Galpin RD, Willis RB, Sabano N (1994) Intramedullary nailing of pediatric femoral fractures. J Pediatr Orthop 14(2):184–189
Mileski RA, Garvin KL, Crosby LA (1994) Avascular necrosis of the femoral head in an adolescent following intramedullary nailing of the femur. A case report. J Bone Joint Surg Am 76(11):1706–1708
Buford D Jr, Christensen K, Weatherall P (1998) Intramedullary nailing of femoral fractures in adolescents. Clin Orthop Relat Res 350:85–89
Astion DJ, Wilber JH, Scoles PV (1995) Avascular necrosis of the capital femoral epiphysis after intramedullary nailing for a fracture of the femoral shaft. A case report. J Bone Joint Surg Am 77(7):1092–1094
Buckaloo JM, Iwinski HJ, Bertrand SL (1997) Avascular necrosis of the femoral head after intramedullary nailing of a femoral shaft fracture in a male adolescent. J South Orthop Assoc 6(2):97–100
Gonzalez-Herranz P et al (1995) Intramedullary nailing of the femur in children. Effects on its proximal end. J Bone Joint Surg Br 77(2):262–266
Raney EM, Ogden JA, Grogan DP (1993) Premature greater trochanteric epiphysiodesis secondary to intramedullary femoral rodding. J Pediatr Orthop 13(4):516–520
Gordon JE et al (2004) Intramedullary nailing of femoral fractures in children through the lateral aspect of the greater trochanter using a modified rigid humeral intramedullary nail: preliminary results of a new technique in 15 children. J Orthop Trauma. 18(7):416–422; discussion 423–424
Keeler KA et al (2009) Antegrade intramedullary nailing of pediatric femoral fractures using an interlocking pediatric femoral nail and a lateral trochanteric entry point. J Pediatr Orthop 29(4):345–351
Flynn JM et al (2001) Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop 21(1):4–8
Ziv I, Blackburn N, Rang M (1984) Femoral intramedullary nailing in the growing child. J Trauma 24(5):432–434
Maruenda-Paulino JI et al (1993) Kuntscher nailing of femoral shaft fractures in children and adolescents. Int Orthop 17(3):158–161
Edgren W (1965) Coxa plana. A clinical and radiological investigation with particular reference to the importance of the metaphyseal changes for the final shape of the proximal part of the femur. Acta Orthop Scand Suppl 84:1–129
Reynolds RAK, Legakis JE, Thomas R, Slongo TF, Hunter JB, Clavert J-M (2012) Intramedullary nails for pediatric diaphyseal femur fractures in older, heavier children: early results. J Child Orthop 6:181–188
Townsend DR, Hoffinger S (2000) Intramedullary nailing of femoral shaft fractures in children via the trochanter tip. Clin Orthop Relat Res 376:113–118
Russell TA (2011) Intramedullary nailing: evolutions of femoral intramedullary nailing: first to fourth generations. J Orthop Trauma 25(Suppl 3):S135–S138
Kuntscher GB (1958) The Kuntscher method of intramedullary fixation. J Bone Joint Surg Am 40-A(1):17–26
Herndon WA et al (1989) Management of femoral shaft fractures in the adolescent. J Pediatr Orthop 9(1):29–32
Timmerman LA, Rab GT (1993) Intramedullary nailing of femoral shaft fractures in adolescents. J Orthop Trauma 7(4):331–337
Reeves RB, Ballard RI, Hughes JL (1990) Internal fixation versus traction and casting of adolescent femoral shaft fractures. J Pediatr Orthop 10(5):592–595
Ramseier LE et al (2010) Femoral fractures in adolescents: a comparison of four methods of fixation. J Bone Joint Surg Am 92(5):1122–1129
Ramseier LE et al (2007) Treatment of open femur fractures in children: comparison between external fixator and intramedullary nailing. J Pediatr Orthop 27(7):748–750
Stans AA, Morrissy RT, Renwick SE (1999) Femoral shaft fracture treatment in patients age 6 to 16 years. J Pediatr Orthop 19(2):222–228
Valdiserri L, Marchiodi L, Rubbini L (1983) Kuntscher nailing in the treatment of femoral fractures in children. Is it completely contraindicated? Ital J Orthop Traumatol 9(3):293–296
Wu CC, Tai CL (2006) A biomechanical comparison of unlocked or locked reamed intramedullary nails in the treatment of mid-third simple transverse femoral shaft fractures. Chang Gung Med J 29(3):275–282
Bankston AB, Keating EM, Saha S (1992) The biomechanical evaluation of intramedullary nails in distal femoral shaft fractures. Clin Orthop Relat Res 276:277–282
Rabenseifner L, Hirasawa Y (1987) A comparative study of biomechanical property of Kuntscher nail and Otte–Plansee nail. Nihon Geka Hokan 56(3):304–312
Letts M et al (2002) Complications of rigid intramedullary rodding of femoral shaft fractures in children. J Trauma 52(3):504–516
Kanellopoulos AD, Yiannakopoulos CK, Soucacos PN (2006) Closed, locked intramedullary nailing of pediatric femoral shaft fractures through the tip of the greater trochanter. J Trauma 60(1):217–222; discussion 222–223
Beaty JH et al (1994) Interlocking intramedullary nailing of femoral-shaft fractures in adolescents: preliminary results and complications. J Pediatr Orthop 14(2):178–183
Skak SV et al (1996) Internal fixation of femoral shaft fractures in children and adolescents: a ten- to twenty-one-year follow-up of 52 fractures. J Pediatr Orthop B 5(3):195–199
Tortolani PJ et al (2001) Tibial nails for femoral shaft fractures in adolescents: “off-label” usage. Orthopedics 24(6):553–557
Park KC et al (2012) Intramedullary nailing versus submuscular plating in adolescent femoral fracture. Injury 43(6):870–875
Jencikova-Celerin L et al (2008) Flexible interlocked nailing of pediatric femoral fractures: experience with a new flexible interlocking intramedullary nail compared with other fixation procedures. J Pediatr Orthop 28(8):864–873
Kirby RM, Winquist RA, Hansen ST Jr (1981) Femoral shaft fractures in adolescents: a comparison between traction plus cast treatment and closed intramedullary nailing. J Pediatr Orthop 1(2):193–197
Blasier RD (2009) Surgical technique for adolescent femur fractures: the trochanteric entry intramedullary nail. Oper Tech Orthop 19(1):24–30
Moroz LA et al (2006) Titanium elastic nailing of fractures of the femur in children. Predictors of complications and poor outcome. J Bone Joint Surg Br 88(10):1361–1366
Leet AI, Pichard CP, Ain MC (2005) Surgical treatment of femoral fractures in obese children: does excessive body weight increase the rate of complications? J Bone Joint Surg Am 87(12):2609–2613
Park H, Kim HW (2012) Treatment of femoral shaft fracture with an interlocking humeral nail in older children and adolescents. Yonsei Med J 53(2):408–415
Fernandez Dell’Oca AA (2002) The principle of helical implants. Unusual ideas worth considering. Injury 33 Suppl 1:SA1–SA27
Prasarn ML et al (2010) The effect of entry point on malalignment and iatrogenic fracture with the Synthes lateral entry femoral nail. J Orthop Trauma 24(4):224–229
MacNeil JA, Francis A, El-Hawary R (2011) A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop 31(4):377–380
Miller DJ et al (2012) Locked intramedullary nailing in the treatment of femoral shaft fractures in children younger than 12 years of age: indications and preliminary report of outcomes. J Pediatr Orthop 32(8):777–780
Egol KA et al (2004) Mismatch of current intramedullary nails with the anterior bow of the femur. J Orthop Trauma 18(7):410–415
Ehmke LW et al (2006) Femoral nailing through the trochanter: the reamer pathway indicates a helical nail shape. J Orthop Trauma 20(10):668–674
Ogden JA (1981) Hip development and vascularity: relationship to chondro-osseous trauma in the growing child. Hip 139–187
Bong MR et al (2007) Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg 15(2):97–106
Synthes GmbH (2012) Expert Adolescent Lateral FemoralNail: technique guide. http://www.synthes.com/MediaBin/International%20DATA/036.000.648.pdf. Accessed 1 Aug 2012
Beaty JH (2005) Operative treatment of femoral shaft fractures in children and adolescents. Clin Orthop Relat Res 434:114–122
Kocher MS et al (2009) Treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Surg 17(11):718–725
Flynn JM, Schwend RM (2004) Management of pediatric femoral shaft fractures. J Am Acad Orthop Surg 12(5):347–359
Patman LJ, Szalay EA (2013) Relative osteopenia after femoral implant removal in children and adolescents. Orthopedics 36(4):e468–e472
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Angadi, D.S., Shepherd, D.E.T., Vadivelu, R. et al. Rigid intramedullary nail fixation of femoral fractures in adolescents: what evidence is available?. J Orthopaed Traumatol 15, 147–153 (2014). https://doi.org/10.1007/s10195-013-0270-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-013-0270-y