Abstract
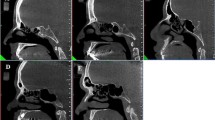
In the present study, we investigated the types and ratio of posterior clinoid process (PCP) pneumatization in paranasal sinus multidetector computed tomography (MDCT). Paranasal MDCT images of 541 subjects (227 males, 314 females), between 15 and 65 years old, were included into the study. Pneumatization of anterior clinoid process and pneumatization types (I, II, or III) were evaluated in the males and females. PCP pneumatization was detected in 20.7 % of the males and 11.5 % of the females. Right, left, and bilateral PCP pneumatizations were detected in 7.9, 5.7, and 7.0 % of the males and 2.9, 3.2, and 4.5 % of the females, respectively. PCP pneumatization of the males is significantly higher than the females. The most detected type of pneumatization was type I (61.2 %) for all groups. In right, left, and bilateral pneumatizations separately, type I pneumatization was the most detected pneumatization type with the ratio of the 70.4, 65.2, and 50.0 %, respectively. In males, type I (61.7 %), and similarly in females, type I (60.6 %) pneumatization were detected more. Type II and type III pneumatizations were detected in decreasing order in both groups. In younger subjects, pneumatization of posterior clinoid process was found as higher, and in older subjects, PCP pneumatization was found as lower. Sclerosis process related to the aging may be responsible for the lower pneumatization ratios in older subjects. Structure of the surrounding regions of PCP is important for surgical procedures related to cavernous sinus, basilar apex aneurysms, and mass lesions. Preoperative radiological examinations are useful for operative planning. Any anomalies to PCP can cause unnecessary injury to the neurovascular complex structure around the cavernous sinus or postclinoidectomy CSF fistulas. Posterior clinoidectomies should be avoided in patients with type III PCP pneumatization to prevent CSF fistulas.





Similar content being viewed by others
References
Standring S, Ellis H, Berkovitz BKB et al (eds) (2005) The anatomical basis of clinical practice. In: Gray’s anatomy. Elsevier Churchill Livingstone, New York. p 462
Tang CT, Baidya NB, Tseng KY, Ma HI (2012) Posterior clinoid process as a landmarker in current endoscopic-assisted neurosurgical approaches. Formos J Surg 45:45–50
Tubbs RS, Salter EG, Oakes WJ (2007) Quantitation of and measurements utilizing the sphenoid ridge. Clin Anat 20:131–134
Kier EL, Rothman SLG (1976) Radiologically significant anatomic variations of the developing sphenoid in humans. In: Bosma JF (ed) Development of the Basicranium. Department of Health, Education, and Welfare, Bethesda, pp. 107–140
Arey LB (1965) Developmental anatomy, 7th edn. W.B. Saunders Co, Philadelphia, p. 306
Gordon MB, Bell AL (1922) A roentgenographic study of the sella turcica in normal children. New York State J Medic 22:54–59
Mahmoud ME-S (1958) The sella in health and disease: the value of the radiographic study of the sella turcica in the morbid anatomical and tomographic diagnosis of intracranial tumors. Brit J Radiol 31:1–100
Berger PE, Harwood-Nash DC, Fitz CR (1976) The dorsum sella in infancy and childhood. Pediatr Radiol 4:214–220
Abuzayed B, Tanriover N, Biceroglu H, Yuksel O, Tanriover O, Albayram S, Akar Z (2010) Pneumatization degree of the anterior clinoid process: a new classification. Neurosurg Rev 33:367–374
Kinnman J (1977) Surgical aspects of the anatomy of the sphenoidal sinuses and the sella turcica. J Anat 124:541–553
Yune H, Holden R, Smith J (1975) Normal variations and lesions of the sphenoid sinus. Am J Roentgenol 124:129–138
Fujioka M, Yung L (1978) The sphenoid sinuses: radiographic patterns of normal development and abnormal findings in infants and children. Radiology 129:133–139
Liu S, Wang Z, Zhou B (2002) Related structures of the lateral sphenoid wall anatomy studies in CT and MRI. Lin Chuang Er Bi Yan Hou Ke Za Zhi 16:407–409
Bolger WE, Butzin CA, Parsons DS (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 101:56–64
Vidic B (1968) The postnasal development of the sphenoidal sinus and its spread into the dorsum sellae and posterior clinoid processes. Am J Roentgenol Radium Therapy, Nucl Med 104:177–183
Sirikci A, Bayazit YA, Bayram M et al (2000) Variations of sphenoid sinus and related structures. Eur Radiol 10:844–848
Birsen U, Gulsah B, Yasemin K et al (2006) Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28:195–201
Burulday V, Muluk NB, Akgül MH, Kaya A, Öğden M (2016) Presence and types of anterior clinoid process pneumatization, evaluated by multidetector computerized tomography. Clin Invest Med 39(3):E105–E110
Dolenc VV (2003) Surgical management of a meningioma in the retrosellar region. Acta Neurochir 145(3):220
Kassam AB, Prevedello DM, Thomas A et al (2008) Endoscopic endonasal pituitary transposition for a transdorsum sellae approach to the interpeduncular cistern. Neurosurgery 62(3suppl 1):57–72 discussion 72-54
Salma A, Wang S, Ammirati M (2010) Extradural endoscope-assisted subtemporal posterior clinoidectomy: a cadaver investigation study. Neurosurgery 67(3 Suppl Operative):ons43–ons48 discussion ons48
Gonzalez LF, Amin-Hanjani S, Bambakidis NC, Spetzler RF (2005) Skull base approaches to the basilar artery. Neurosurg Focus 19(2):E3
Figueiredo EG, Zabramski JM, Deshmukh P, Crawford NR, Preul MC, Spetzler RF (2006) Anatomical and quantitative description of the transcavernous approach to interpeduncular and prepontine cisterns. Technical note. J Neurosurg 104(6):957–964
Bambakidis NC, Gonzalez LF, Amin-Hanjani S et al (2005) Combined skull base approaches to the posterior fossa. Technical note. Neurosurg Focus 19(2):E8
Chanda A, Nanda A (2002) Anatomical study of the orbitozygomatic transsellar-transcavernous-transclinoidal approach to the basilar artery bifurcation. J Neurosurg 97(1):151–160
Nutik SL (1998) Pterional craniotomy via a transcavernous approach for the treatment of low-lying distal basilar artery aneurysms. J Neurosurg 89:921–926
Dolenc VV, Skrap M, Sustersic J et al (1987) A transcavernous-transsellar approach to the basilar tip aneurysms. Br J Neurosurg 1(2):251–259
Seoane E, Tedeschi H, de Oliveira E, Wen HT, Rhoton AL Jr (2000) The pretemporal transcavernous approach to the interpeduncular and prepontine cisterns: microsurgical anatomy and technique application. Neurosurgery 46(4):891–898 discussion 898-9
Author contributions
Veysel Burulday: Planning, designing, data collection, and literature survey.
Mehmet Hüseyin Akgül: Planning, designing, data collection, and literature survey.
Nuray Bayar Muluk: Planning, designing, literature survey, statistical analysis, and writing.
Mehmet Faik Ozveren: Literature survey.
Ahmet Kaya: Data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study is retrospective. Ethics committee approval was obtained, and there is no need to take informed consent because the data was evaluated retrospectively.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There are no funds for this article.
Rights and permissions
About this article
Cite this article
Burulday, V., Akgül, M.H., Muluk, N.B. et al. Evaluation of posterior clinoid process pneumatization by multidetector computed tomography. Neurosurg Rev 40, 403–409 (2017). https://doi.org/10.1007/s10143-016-0794-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-016-0794-8