Abstract
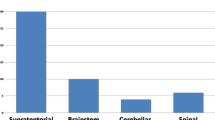
Brain stem cavernomas (BSCs) are angiographically occult vascular malformations in an intricate location. Surgical excision of symptomatic BSCs represents a neurosurgical challenge especially in developing countries. We reviewed the clinical data and surgical outcome of 24 consecutive cases surgically treated for brain stem cavernoma at the Neurosurgery Department, Alexandria University, between 2006 and 2014. All patients were followed up for at least 12 months after surgery and the mean follow-up period was 45 months. All patients suffered from at least two clinically significant hemorrhagic episodes before surgery. There were 10 males and 14 females. The mean age was 34 years (range 12 to 58 years). Fourteen cases had pontine cavernomas, 7 cases had midbrain cavernomas, and in 3 cases, the lesion was found in the medulla oblongata. The most commonly used approach in this series was the midline suboccipital approach with or without telovelar exposure (9 cases). There was a single postoperative mortality in this series due to pneumonia. Fourteen cases (58.3 %) showed initial worsening of their preoperative neurological status, most of which was transient and only three patients had permanent new deficits and one case had a permanent worsening of her preoperatively existing hemiparesis. There was neither immediate nor long-term rebleeding in any of our cases. In spite of the significant associated risks, surgery for BSCs in properly selected patients can have favorable outcomes in most cases. Surgery markedly improves the risk of rebleeding and should be considered in patients with accessible lesions.



Similar content being viewed by others
References
Abla AA, Turner JD, Mitha AP, Lekovic G, Spetzler RF (2010) Surgical approaches to brainstem cavernous malformations. Neurosurg Focus 29(3), E8. doi:10.3171/2010.6.FOCUS10128
Abla AA, Lekovic GP, Turner JD, de Oliveira JG, Porter R, Spetzler RF (2011) Advances in the treatment and outcome of brainstem cavernous malformation surgery: a single-center case series of 300 surgically treated patients. Neurosurgery 68(2):403–414. doi:10.1227/NEU.0b013e3181ff9cde
Awad IA, Robinson JR, Mohanty S, Esters ML (1993) Mixed vascular malformations of the brain: clinical and pathogenetic considerations. Neurosurgery 33:179–188
Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, Sure U (2002) Cerebral cavernomas in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25(1–2):1–53
Bertalanffy H, Gilsbach JM, Eggert HR, Seeger W (1991) Microsurgery of deep-seated cavernous angiomas: report of 26 cases. Acta Neurochir (Wien) 108(3–4):91–99
Brown AP, Thompson BG, Spetzler RF (1996) The two-point method: evaluating brain stem lesions. BNI Q 12(1):20–24
Cantore G, Missori P, Santoro A (1999) Cavernous malformation of the brainstem. Intra axial anatomical pitfalls and surgical strategies. Surg Neurol 52(1):84–93
Chen L, Zhao Y, Zhou L, Zhu W, Pan Z, Mao Y (2011) Surgical strategies in treating brainstem cavernous malformations. Neurosurgery 68(3):609–620. doi:10.1227/NEU.0b013e3182077531
Chen X, Weigel D, Ganslandt O, Fahlbusch R, Buchfelder M, Nimsky C (2007) Diffusion tensor-based fiber tracking and intraoperative neuronavigation for the resection of a brainstem cavernous angioma. Surg Neurol 68(3):285–291
Cohen DS, Zubay GP, Goodman RR (1995) Seizure outcome after lesionectomy for cavernous malformation. J Neurosurg 83:237–242
Dukatz T, Sarnthein J, Sitter H, Bozinov O, Benes L, Sure U, Bertalanffy H (2011) Quality of life after brainstem cavernoma surgery in 71 patients. Neurosurgery 69(3):689–695. doi:10.1227/NEU.0b013e31821d31b7
Fahlbusch R, Strauss C, HukW RG, Kompf D, Ruprecht KW (1990) Surgical removal of pontomesencephalic cavernous hemangiomas. Neurosurgery 26(3):449–457
Ferroli P, Sinisi M, Franzini A, Giombini S, Solero CL, Broggi G (2005) Brainstem cavernomas: long-term results of microsurgical resection in 52 patients. Neurosurgery 56(6):1203–1214
Fritschi JA, Reulen HJ, Spetzler RF, Zabramski JM (1994) Cavernous malformation of the brainstem: a review of 139 cases. Acta Neurochir (Wien) 130:35–46
Garcia RM, Ivan ME, Lawton MT (2015) Brainstem cavernous malformations: surgical results in 104 patients and a proposed grading system to predict neurological outcomes. Neurosurgery 76(3):265–277. doi:10.1227/NEU.0000000000000602
Gross BA, Batjer HH, Awad IA, Bendok BR (2009) Brainstem cavernous malformations. Neurosurgery 64(5):E805–E818
Hauck EF, Barnett SL, White JA, Samson D (2009) Symptomatic brainstem cavernomas. Neurosurgery 64(1):61–71. doi:10.1227/01.NEU.0000335158.11692.53
Houtteville JP (1997) Brain cavernoma: a dynamic lesion. Surg Neurol 48:610–614
Kondziolka D, Lunsford LD, Kestle JR (1995) The natural history of cerebral cavernous malformation. J Neurosurg 83:820–824
Kyoshima K, Kobayashi S, Gibo H, Kuroyanagi T (1993) A study of safe entry zones via the floor of the fourth ventricle for brain-stem lesions. Report of three cases. J Neurosurg 78(6):987–993
Li H, Ju Y, Cai BW, Chen J, You C, Hui XH (2009) Experience of microsurgical treatment of brainstem cavernomas: report of 37 cases. Neurol India 57(3):269–273. doi:10.4103/0028-3886.53269
Lüdemann W, Ellerkamp V, Stan AC, Hussein S (2002) De novo development of a cavernous malformation of the brain: significance of factors with paracrine and endocrine activity: case report. Neurosurgery 50(3):646–649
Maraire JN, Abdulrauf SI, Berger S, Knisely J, Awad IA (1999) De novo development of a cavernous malformation of the spinal cord following spinal axis radiation. Case report. J Neurosurg Spine 90:234–238
Maraire JN, Awad IS (1995) Intra-cranial cavernous malformation: lesion behaviour and management strategies. Neurosurgery 37:591–605
Notelet L, Houtteville JP, Khoury S, Lechevalier B, Chapon F (1997) Proliferating cell nuclear antigen (PCNA) in cerebral cavernomas: an immunocytochemical study of 42 cases. Surg Neurol 47:364–370
Ohue S, Fukushima T, Kumon Y, Ohnishi T, Friedman AH (2010) Surgical management of brainstem cavernomas: selection of approaches and microsurgical techniques. Neurosurg Rev 33(3):315–322. doi:10.1007/s10143-010-0256-7
Pandey P, Westbroek EM, Gooderham PA, Steinberg GK (2013) Cavernous malformation of brainstem, thalamus, and basal ganglia: a series of 176 patients. Neurosurgery 72(4):573–589. doi:10.1227/NEU.0b013e318283c9c2
Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, Zabramski JM (1999) Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg 90(1):50–58
Recalde RJ, Figueiredo EG, de Oliveira E (2008) Microsurgical anatomy of the safe entry zones on the anterolateral brainstem related to surgical approaches to cavernous malformations. Neurosurgery 62(3 Suppl 1):9–15. doi:10.1227/01.neu.0000317368.69523.40
Rohde V, Berns E, Rohde I, Gilsbach JM, Ryang YM (2007) Experiences in the management of brainstem hematomas. Neurosurg Rev 30(3):219–224
Royo A, Utrilla C, Carceller F (2013) Surgical management of brainstem-expanding lesions: the role of neuroimaging. Semin Ultrasound CT MR 34(2):153–173. doi:10.1053/j.sult.2013.01.006
Samii M, Eghbal R, Carvalho GA, Matthies C (2001) Surgical management of brainstem cavernomas. J Neurosurg 95(5):825–832
Sanai N, Mirzadeh Z, Lawton MT (2010) Supracerebellar-supratrochlear and infratentorial-infratrochlear approaches: gravity-dependent variations of the lateral approach over the cerebellum. Neurosurgery 66(6 Suppl Operative):264–274. doi:10.1227/01.NEU.0000369653.12185
Sandalcioglu IE, Wiedemayer H, Secer S, Asgari S, Stolke D (2002) Surgical removal of brain stem cavernous malformations: surgical indications, technical considerations, and results. J Neurol Neurosurg Psychiatry 72(3):351–355
Sola RG, Pulido P, Pastor J, Ochoa M, Castedo J (2007) Surgical treatment of symptomatic cavernous malformations of the brainstem. Acta Neurochir (Wien) 149(5):463–470
Sure U, Butz N, Schlegel J, Siegel A, Mennel HD, Bien S, Bertalanffy H (2001) Endothelial proliferation, neoangiogenesis and potential de novo generation of cerebral vascular malformations. J Neurosurg 94:972–977
Ulrich NH, Kockro RA, Bellut D, Amaxopoulou C, Bozinov O, Burkhardt JK, Sarnthein J, Kollias SS, Bertalanffy H (2014) Brainstem cavernoma surgery with the support of pre- and postoperative diffusion tensor imaging: initial experiences and clinical course of 23 patients. Neurosurg Rev 37(3):481–491. doi:10.1007/s10143-014-0550-x
Vajtai I, Varga Z (1998) Origin of de novo central nervous system cavernomas. J Neurosurg 88:616–617
Wurm G, Schnizer M, Fellner FA (2007) Cerebral cavernous malformations associated with venous anomalies: surgical considerations. Neurosurgery 61(1 Suppl):390–404. doi:10.1227/01.neu.0000279231.35578.da
Yagmurlu K, Rhoton AL Jr, Tanriover N, Bennett JA (2014) Three-dimensional microsurgical anatomy and the safe entry zones of the brainstem. Neurosurgery 10(Suppl 4):602–619. doi:10.1227/NEU.0000000000000466
Zimmermann RS, Septzler RF, Lee KS, Zabramski JM, Hargraves RW (1991) Cavernous malformations of the brainstem. J Neurosurg 75:32–39
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Helmut Bertalanffy, Hannover, Germany
This important and timely publication furnishes evidence of a new quality of neurosurgical management in Egypt. The authors of this article eloquently demonstrate that intrinsic surgery within the brainstem is not only feasible in their country but is possible even with excellent results. Regrettably, too many neurologists, neurosurgeons, or radiooncologists are still unaware about this possibility. As shown by doctors Farhoud and Aboul-Enein, brainstem surgery requires not only microsurgical skillfulness but also appropriate technical equipment and—most importantly—the clinical know-how for patient selection, adequate indication for surgery, and correct choice of the surgical approach including the precise entry zone into the brainstem. All these prerequisites are now available in Egypt as I could convince myself on many occasions while visiting this country. More than a decade ago, both authors have been my pupils, studying with me in Germany for a significant period of time. Over the past years, they have become experienced and talented neurosurgeons, able to safely treat patients even with difficult brainstem lesions. I wish to commend both authors for their achievements and the good results in this remarkable patient series.
I also wish to encourage more colleagues in Egypt and elsewhere to take notice of this progress in the microsurgical management of brainstem lesions in a developing country and to consider direct brainstem surgery in selected cases or to send their patients with brainstem lesions to experts in the field such as doctors Ahmed Farhoud and Hisham Aboul-Enein.
Rights and permissions
About this article
Cite this article
Farhoud, A., Aboul-Enein, H. Surgical management of symptomatic brain stem cavernoma in a developing country: technical difficulties and outcome. Neurosurg Rev 39, 467–473 (2016). https://doi.org/10.1007/s10143-016-0712-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-016-0712-0